Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Cardio MurmursOutline
Caricato da
swoljaswol1Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Cardio MurmursOutline
Caricato da
swoljaswol1Copyright:
Formati disponibili
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 4/4/2011
Definition: A heart murmur is as a series of vibrations of varying intensity, pitch, configuration, and duration. It is generally agreed upon that murmurs result from turbulent flow due to: 1. High flow, 2. Flow through an irregular orifice, or 3. A combination of both. Obesity, emphysema, and the presence of significant pericardial or pleural effusion will decrease the intensity of a murmur, whereas a thin body habitus often will accentuate it. Clinical significance The association of murmurs with palpable thrills is always clinically significant (except in the case of a tiny VSD), as are all diastolic murmurs. Innocent murmurs are systolic ejection murmurs which are usually less than Grade 3 and are accomopanied by an otherwise unremarkable cardiovascular examination. They often vary with inspiration, diminish in the upright position, and are most frequently heard in thin individuals. Functional murmurs represent benign systolic ejection murmurs experienced during highflow states, but are excluded from the innocent category due to their association with abnormal physiology. They include murmurs of thyrotoxicosis, pregnancy, anemia, fever, exercise, and peripheral arteriovenous fistula. Characterization of adventitious heart sounds Intensity: systolic murmurs of grade 3 or more in intensity are usually hemodynamically significant. Grade 1: so faint that it can be heard only with special effort Grade 2: faint but can be heard easily Grade 3: moderately loud Grade 4: very loud Grade 5: extremely loud and can be heard if only the edge of the stethoscope is in contact with the skin but cannot be heard if the stethoscope is removed from the skin. Grade 6: exceptionally loud and can be heard with the stethoscope just removed from contact with the chest. Diagnostic Maneuvers Preload : Standing, valsalva, vasodilators (Ex. nitrates) LV volume, venous return Less flow decreases intensity of most murmurs except MVP, HCM Preload : Lying down, squatting, hand grip, elevating legs, vasoconstrictors LV volume More flow intensity of most murmurs except MVP, HCM Handgrip afterload MVP, AR HCM, AS
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 1/4/2011
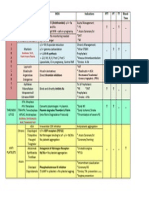
Systolic Holosystolic: Merge with S1 and persist through S2. Obliterates S2. Tend to have a uniform intensity throughout systole Usually represent regurgitation of atrioventricular flow: Mitral regurgitation: maximal at the apex or axilla. Tricuspid regurgitation or VSD: best heard at the sternal border Rarely in isolation. Usually secondary to right heart dilation. Decrease with expiration and Valsalva Pulsatile liver, prominent V waves Ebsteins Anomaly: Lithium. Downward displacement of tricuspid valve makes right atrium appear larger Ejection (Midsystolic): Begin after S1 and end before S2 Tend to have a crescendo-decrescendo pattern. Intensity closely parallels changes in cardiac output. Usually represent high flow and/or flow across a narrowed ventricular outflow tract: ASD likely if accompanied by fixed splitting of S2 Aortic stenosis (congenital or acquired). Severe when area < 0.8 cm2 Best heard at the first or second interspace Usually accomanied by S4 Usually associated with aortic regurgitation as well. Asymptomatic AS needs no treatment. Hypertrophic cardiomyopathy Worse in low-flow states (ex. dehydrated young athletes) since the irregular septum bulges over to obstruct the outflow tract. Pulmonic stenosis: almost always associated with Tetrology of Fallot Diastolic: Always clinically significant High-pitched (blowing): imply flow from a high-pressure to low-pressure chamber Pulmonic regurgitation in pulmonary hypertension and pulmonary artery dilation Primary PH and Eisenmenger syndrome Aortic regurgitation: worse by afterload from backflow across incomp. valve. Ex. squatting, making a fist. Medical: if asymptomatic + stable Diuretic, vasodilator, ACE inhibitor, digoxin Surgery: Acute AR (ex. post MI) or EF < 55% VSD and PDA caused by large flow across the MV secondary to left-to-right shunt Low-pitched ("rumbles"): imply filling across an AV valve Mitral stenosis: Bad when area <1.5cm2 Correlates poorly with intensity, since as it get worse flow declines across the narrowed orifice. Duration of the murmur is better predictor of severity. Medical: Diuretic, warfarin (usually) Surgery: Percutaneous is good Tricuspid stenosis: Augmented with inspiration Almost always associated with mitral stenosis. Continuous: begins in systole and extends through S2 into part or all of diastole. PDA Central venous hum, mammary souffle of pregnancy (both benign)
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 1/4/2011
Sources O'Gara Patrick, Braunwald Eugene, "Chapter 230. Valvular Heart Disease" (Chapter). Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J: Harrison's Principles of Internal Medicine, 17e Bashore Thomas M, Granger Christopher B, Hranitzky Patrick, Patel Manesh R, "Chapter 10. Heart Disease" (Chapter). McPhee SJ, Papadakis MA: CURRENT Medical Diagnosis & Treatment 2011 O'Rourke Robert A, Shaver James A, Silverman Mark E, "Chapter 12. The History, Physical Examination, and Cardiac Auscultation" (Chapter). Fuster V, ORourke RA, Walsh RA, PooleWilson P, Eds. King SB, Roberts R, Nash IS, Prystowsky EN, Assoc. Eds.: Hurst's The Heart, 12e
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 1/4/2011
c-wave: r ventricle contracting bulges tricuspid valve slightly.
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 1/4/2011
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 1/4/2011
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 1/4/2011
Top. Normal physiologic splitting. During expiration, the aortic (A2) and pulmonic (P2) components of the second heart sound are separated by <30 ms and are appreciated as a single sound. During inspiration, the splitting interval widens, and A2 and P2 are clearly separated into two distinct sounds. Bottom. Audible expiratory splitting. Wide physiologic splitting is caused by a delay in P2. Reversed splitting is caused by a delay in A2, resulting in paradoxical movement; i.e., with inspiration P2 moves towards A2, and the splitting interval narrows. Narrow physiologic splitting occurs in pulmonary hypertension, and both A2 and P2 are heard during expiration at a narrow splitting interval because of the increased intensity and high-frequency composition of P2. (From JA Shaver, JJ Leonard, DF Leon, Examination of the Heart, Part IV, Auscultation of the Heart. Dallas, American Heart Association, 1990, p 17. Copyright, American Heart Association.)
USMLE Step 1 Cardiovascular Medicine - Murmurs
Mark Tuttle 1/4/2011
Best auscultation points for murmurs
Potrebbero piacerti anche
- Hematoma Type: EpiduralDocumento2 pagineHematoma Type: EpiduralRenata V CNessuna valutazione finora
- Nervat KranialeDocumento4 pagineNervat KranialeMarsiano QendroNessuna valutazione finora
- Nervat KranialeDocumento4 pagineNervat KranialeMarsiano QendroNessuna valutazione finora
- Drugs MOA Indications PTT PT TT Bleed-Time: Hirudin DerivativesDocumento1 paginaDrugs MOA Indications PTT PT TT Bleed-Time: Hirudin DerivativesRenata V CNessuna valutazione finora
- Autosomal Dominant: "Hat of Man Power-V" HDocumento4 pagineAutosomal Dominant: "Hat of Man Power-V" HRenata V CNessuna valutazione finora
- Disease Destroys Manifestations: Spinothalamic Tract (STT) ContralateralDocumento3 pagineDisease Destroys Manifestations: Spinothalamic Tract (STT) ContralateralRenata V CNessuna valutazione finora
- Poorly Gram Staining OrganismsDocumento1 paginaPoorly Gram Staining OrganismsRenata V CNessuna valutazione finora
- Brachial Plexus Chart - 0001Documento1 paginaBrachial Plexus Chart - 0001Renata V CNessuna valutazione finora
- Pressure Volume LoopDocumento4 paginePressure Volume LoopVinodh PerumalNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)