Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
A A A A C CC C A A A A D D D D Eeee M M M M IIII C CC C S S S S C CC C IIII Eeee N N N N C CC C Eeee S S S S
Caricato da
makerk82Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
A A A A C CC C A A A A D D D D Eeee M M M M IIII C CC C S S S S C CC C IIII Eeee N N N N C CC C Eeee S S S S
Caricato da
makerk82Copyright:
Formati disponibili
Academic Sciences
International Journal of Pharmacy and Pharmaceutical Sciences
ISSN- 0975-1491 Vol 4, Issue 2, 2012
Research Article
IN-VITRO ANTIFUNGAL ACTIVITY OF HYBANTHUS ENNEASPERMUS F MUELL
NAPOLEON ARUMUGAM*, SASIKUMAR KANDASAMY, M.SEKAR**
Pharmaceutical Chemistry Division, School Of Advanced Sciences, Vit University, Vellore, Tamil Nadu 632 014, India. **Ehrlich Laboratory, Chennai, India. Email: aanapoleon@vit.ac.in, neppharma@yahoo.co.in. Received: 13 Dec 2011, Revised and Accepted: 10 Feb 2012 ABSTRACT The aim of present investigation was to evaluate the antifungal efficacy of the different plant extracts of Hybanthus enneaspermus. The antifungal property of the petroleum ether, chloroform and methanol extracts of the plant Hybanthus enneaspermus, were tested against a group of fungi, viz., Aflatoxin producing fungi, Aspergillus flavus, Aspergillus fumigatus and human pathogenic fungi Candida albicans and Candida tropicalis by well diffusion method. The methanol extract exhibited significant antifungal activity on most of the fungal strains, viz. Aspergillus flavus, Aspergillus fumigatus, Candida albicans and Candida tropicalis followed by the petroleum ether extract and chloroform extract. This report is first of its kind showing antifungal activity of Hybanthus enneaspermus. Preliminary phytochemical screening revealed that the petroleum ether extract shows presence of both triterpenoids and steroids, chloroform extract shows presence of steroids only and methanolic extracts shows presence of steroids, alkaloids, flavonoids, saponins, phenolic compound, amino acid, protein and tannins. Keywords: Hybanthus enneaspermus, Antifungal activity, Phytochemical, Fluconazole, Aspergillus flavus, Candida albicans
INTRODUCTION Plants that are traditionally used in the treatment of bacterial and fungal infections or related ailments could be a good source for new safer drugs and could offer potential lead in the development of novel herbal medicines that are active against pathogenic micro organisms. Many plants are gaining importance due to fungi toxicity. Natural products of higher plants may possess a new source of antimicrobial agents with possibly novel mechanism of action. They are effective in the treatment of infectious diseases, while simultaneously mitigating many of the side effects that are often associated with synthetic antimicrobials1. Numerous research works has been done aiming to know the different antimicrobial and phytochemical constituents of medicinal plants and in using them for the treatment of microbial infections (both topical and systemic applications) as possible alternatives to chemically synthetic drugs to which many infectious microorganisms have become resistant2. Hybanthus enneaspermus3 F. Muell (Synonyms: Ionidium enneaspermus DC, Family: Violaceae) is native of high altitude Himalaya region and warmer parts of India from Delhi to Bengal and throughout Deccan Peninsula. It is reported to be used as a tonic, diuretic4, anti-gonorrhoetic and demulcent. Roots are given in urinary infections and for bowel complaints of children5. The plant has been reported to have anti-inflammatory6, antitussive7, antiplasmodial8, anticonvulsant9, free radical scavenging activity and antidiabetic10. Hybanthus enneaspermus: A small, suffrutescent perennial herb 15-30cm high, with many diffuse or ascending branches, glabrous or more or less pubescent stem sparingly branched with woody base and spreading erect branches. Root spindle shaped, cylindrical, rough and light yellow in colour leaves linear or lanceolate, 4-5cm. by 3-8mm, subsessile, entire or with serrated margins; stipules gland tipped, subulate. Flowers red, axillary, solitary, pedicels shorter than the leaves, 6-12mm long, erect, slender; bracts small, above the middle of the pedicel. Capsules are about 6mm diameter, subglobose with ribbed seeds. Seeds ovoid, acute, longitudinally striate, yellowish white, about 1.5mm long. Hybanthus collected from sandy soil has been identified for possible cultivation in gardens for ornamental purposes. Their small sized body leaves and flowers are of different interesting conformation and colour which can attract many people. The components of the plant dipeptide alkaloid (Aurantiamide acetate), a Triterpene (Isoarborinol) and Sitosterol are previously isolated from Hybanthus enneaspermus. Although chemical studies were shown for the presence of alkaloids, flavonoids, triterpene and steroids in this species, but no data are available concerning its
detailed structural data11 and its biological activities. Hybanthus enneaspermus is of considerable chemotaxonomic importance, as it constitutes the first reported of a Violaceae plant to elaborate a peptide alkaloid12. In the present investigation, phytochemical screening and efforts were made to find out the antifungal activity of different extracts of H.enneaspermus on Aflatoxin producing fungi, Aspergillus flavus, Aspergillus fumigatus and human pathogenic fungi Candida albicans and Candida tropicalis by well diffusion method. MATERIALS AND METHODS Plant material collection The plant of Hybanthus enneaspermus (family: Violaceae) for present studies were identified by a Mr. Prabhakaran, Horticulturist in VIT University. The entire plant and plant powder used for present studies were collected from the Sri Vinayaga Herbals Madurai. The powdered plant materials (shade dried) were used for the extraction and isolation purpose. Preparation of extracts The dried powdered plant material (500gm) of Hybanthus enneaspermus were extracted petroleum ether (60-80C) by using Soxhlets apparatus for 9hrs and the solvent was removed after the completion of extraction process, the extracts were concentrated by distillation under vaccum. The petroleum ether marc was air dried before extracting with chloroform and the chloroform extracts were concentrated by distillation under vaccum. The same chloroform marc was taken and air dried and it is extracted with methanol. Methanolic extracts were concentrated by distillation under vaccum. Solvents were removed from all the three extracts under vacuum and a semisolid mass was obtained. The extracts were stored in a refrigerator. Preliminary phytochemical studies Preliminary phytochemical studies were carried out for the presence of saponins, tannins, flavonoids, anthraquinones, terpenoids and alkaloids using various color reactions to identify the nature of phytoconstituents presence13, 14(Table 1). Antifungal Assay Preparation of test solution Accurately weighed dried extracts were dissolved in Dimethyl Formamide (DMF) in sterile test tubes to obtain concentration of 2mg/mL; 4mg/mL and 5mg/mL of the each extract (Petroleum ether, Chloroform and Methanolic extract) and subjected to
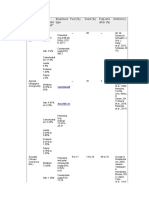
Arumugam et al. Int J Pharm Pharm Sci, Vol 4, Issue 2, 594-596 antifungal screening. 0.5gm of plant powder mixed with 20ml of Potato Dextrose Agar (PDA) medium constitute 25mg/ml. the control (a) contained only 20mL of PDA medium, control (b) contained 200mg of Bavistin (fungicide) added to 20mL of PDA medium with (10mg/ml). Media The culture media used for antifungal testing were Potato Dextrose Agar (PDA) of HiMedia Pvt. Ltd., Mumbai, India. Microorganisms Used Aspergillus flavus, Aspergillus fumigates, Candida albicans and Candida tropicalis Inoculum Preparation The fungal stock cultures were maintained on Potato Dextrose Agar slant, which were stored at 4C. Each microorganisms maintained on PDA agar base were used to assess the antifungal activity of the plant extracts. Three or five similar colonies were selected and transferred to 50ml Potato Dextrose broth cultures were incubated for 48h at 25C. Inoculum of the test organisms were prepared by inoculating a loopful of organism into sterile saline from 24hrs old cultures on PDA agar slants incubated at 25C. The turbidity was matched with 0.5 McFarland standards15 which correspond to 1.5 X 108 CFU/mL. One mL of this suspension was diluted aseptically to 10mL with sterile saline to give culture density of about 107 CFU/mL. Antifungal Susceptibility Test (AST) Antibiotic sensitivity test was conducted against standard antibiotics Fluconazole (1000g/ml) for all fungal species by well diffusion method. Stock solutions of standards were prepared in DMF and diluted with same to obtained required standard concentration. Antifungal susceptibility test was performed by cup plate method as described under antimicrobial screening, where in the one cups were filled with 0.1mL (100 l) of respective stock solutions of antibiotics with micropipette. Preparation of standard drug (Fluconazole) 20 Fluconazole tablets (each tablet containing 150mg of Fluconazole16) are taken and weighed. The tablets are crushed in a mortar and the weight of powder equivalent to 100mg of Fluconazole is taken in a 100ml beaker and 50ml methanol is added to it. The solution is stirred well for 10mins and filtered. The residue is washed twice with 20ml methanol each. The filtrate is taken in a 100mL volumetric flask and the volume is made to 100mL with methanol. The resultant solution contains 1000g/mL of solution. 10ml of the solution is then taken and it is evaporated to dryness in a Round Bottom flask. The dried contents are then dissolved in 5ml of Di-methyl formamide (DMF) and poured in a sample vial. The RB flask is washed two times each with 2ml of DMF and finally the volume of the sample vial is made into 10ml with DMF. The DMF solution contains 1000g/mL of Fluconazole. Antifungal Screening Well Plate Diffusion Method The plant extracts were tested for antifungal activity by cup plate (well plate diffusion17) method using four bacterial cultures. 0.1mL of fungal suspension was thoroughly mixed with 25mL of sterile molten PDA agar and poured in presterilized petri plates and set aside. After congealing the seeded agar was punched out with sterile cork borer in order to make three cups (6mm) at a spaced out position in the petri plate. The entire three well were filled with 0.1mL (100 L) of the Petroleum ether extract at three different concentrations 2mg/mL, 4mg/mL and 5mg/mL. This procedure is repeated for other extract like chloroform and methanol extract. Culture control and DMF as solvent control were also maintained. These agar plates were set aside at room temperature for one hour for diffusion and then incubated at 25C for 48 hours. After incubation, the diameter of zone of inhibition was measured in millimeter (mm) and the value was recorded. RESULT AND DISCUSSION In the present investigation, the methanolic extract showed maximum inhibitory effect on the four fungal strains, viz. Aspergillus flavus, Aspergillus fumigatus, Candida albicans and Candida tropicalis followed by the petroleum ether extract and chloroform extract (Table 2). The results indicated that as the concentration of the plant extract increased, the zone of inhibition produced also found to be increased. All the extracts showed high to moderate zone of inhibition against four fungal strains when compared to the standard drug. This report is first of its kind showing antifungal activity of Hybanthus enneaspermus. The results of this study support the use of these plants for human and animal disease therapy and reinforce the importance of the ethnobotanical approach as a potential source of bioactive substances
Comparison of Zone of Inhibition (Highest) of Hybanthus Extracts with Standard Drugs against Human Pathogenic Fungi
30 25 25 20 20 15 15 10 5 0 14
11 14 14 18 16
23 20 15
15 15
Petroleum Ether Chloroform Methanol Fluconozole
14
14
Aspergillus flavus
Aspergillus fumigatus
Candida albicans
Candida tropicalis
Fig. 1: Comparison of zone of Inhibition (highest) of Hybanthus extracts with standard drugs against human pathogenic fungi.
595
Arumugam et al. Int J Pharm Pharm Sci, Vol 4, Issue 2, 594-596 Table 1: Phytochemical Investigation of the different extracts of Hybanthus enneaspermu S.No 1 2 3 4 5 6 7 8 9 Phytochemical Test Triterepenoids Steroids Alkaloids Flavonoids Phenolic Compounds Tannin Saponin Amino acid Protein Petroleum Ether + + Chloroform + Methanol + + + + + + + +
Table 2: Antifungal activity of plant extract of H.enneaspermus at 25C 2C Plant Extract Concentration mg/mL Microorganisms (zone of inhibition in mm) Aspergillus flavus Aspergillus fumigatus 20 25 8 13 10 14 14 15 8 11 10 13 11 14 10 12 11 15 14 18 Candida albicans 20 9 12 14 10 12 14 10 12 16 Candida tropicalis 23 11 14 15 10 11 15 10 12 15
Fluconazole DMF Petroleum ether
Chloroform
Methanol
1 2 4 5 2 4 5 2 4 5
ACKNOWLEDGEMENT The authors wish to thank the Chancellor and Vice chancellor and Colleagues of VIT University, Vellore, TN, India for their constant encouragement and providing necessary facilities to carry out this study. REFERENCES 1. Sowmya G. Shetty, Vinayachandra, Syed Hidayathulla, K.R. Chandrashekar. Antimicrobial activity and phytochemical screening of Pterospermum reticulatum wight & arn. International Journal of Pharmacy and Pharmaceutical Sciences. 2011: 3(5): 35-37. Surekha Shukla, Sanjukta Chatterji, Deepak Kumar Yadav, Geeta Watal. Antimicrobial efficacy of raphanus sativus root juice. International Journal of Pharmacy and Pharmaceutical Sciences. 2011: 3(5): 89-92. Krithikar.K.R, Basu.B.D (1975). Indian Medicinal Plants, International Book Distributors, Dehra Dun, 212-213. Chopra.R.N, Nayar S.L, Chopra I.C (1956). Glossary of Indian medicinal plants (CSIR, New Delhi), 129-130. Khare. C.P (2007). Indian medicinal plants, Springer International Edition, 329-330. Boominathan.R, Parimaladevi.B, Mandal. S.C, Ghoshal. S.K. Antiinflammatory evaluation of Ionidium suffruticosam Ging. in rats. Journal of Ethnopharmacology. 2004: 91:367-370. Boominathan.R, Parimala Devi. B, Mandal. S.C. Evaluation of antitussive potential of Ionidium suffruticosam Ging. (Violaceae) extract in albino mice. Phytotherapy Research. 2003: 17: 838-839
8.
9.
10. 11. 12.
2.
3. 4. 5. 6.
13. 14.
15.
16. 17.
7.
Weniger.B, Lagnika.L, Vonthron Senecheau.C, Adjabimey.D, Gbenou.J, Moudachirou.M, Brun. R, Anton. R, Sanni. A. Evaluation of ethnobotanically selected Benin medicinal plants for their in vitro antiplasmodial activity. Journal of Ethnopharmacology. 2004: 90: 279. Hemlatha. S, Wahi. A.K, Singh.P.N, Chansouria.J.P.N. Anticonvulsant and free radical scavenging activity of Hybanthus enneaspermus: A preliminary screening. Indian Journal of Traditional Knowledge.2003: 2 (4): 383-388. Irfan Ali Khan, Atiya Khanum (2005). Herbal Therapy for Diabetes Volume I, Ukaaz Publications. Hyderabad, 36-37. Warnhoff. E.W (1970). Foertschritte der chemie organischer naturstoffe, Volume 28, (Springer-Verlag, Berlin), 162-203. Raveendra Retnam, John De Britto. Antimicrobial activity of a medicinal plant Hybanthus enneaspermus (Linn.) F.Muell. Journal of Natural Product radiance. 2007:6: 366-368. Kokate.C.K, Purohir.A.P, Gokhale.S.B (2001). Pharmacognosy, 17th edition, Nirali Prakashan Publication, 607-611. Harborne. J.B (2001). Phytochemical Methods, a guide to modern technique of plants, 3rd Edition, Springer Private Ltd, New Delhi, 40-100. Finegold.S.M, Baron.E.J. (1986). In Finegold and Baron E.J, edited. Diagnostic Microbiology, 7th edition. The C.V Mosby Co. St. Louis, 176-177. Indian Pharmacopoeia, Volume II, (2010), Indian Pharmacopoial Commission, Ghaziabad, India, 1354-55. Perez. C, Pauli. M, Bazer.P. An antibiotic assay by the well agar method. Acta Biologiae et Medicine Experimentalis. 1990: 15: 113-115.
596
Potrebbero piacerti anche
- Review of Related LiteratureDocumento8 pagineReview of Related LiteratureKassNessuna valutazione finora
- Cytotoxic, Antioxidant and Antimicrobial Activities and Phenolic Contents of Eleven Salvia Species From IranDocumento10 pagineCytotoxic, Antioxidant and Antimicrobial Activities and Phenolic Contents of Eleven Salvia Species From IranIsmael GuardiaNessuna valutazione finora
- Article 1454269320Documento5 pagineArticle 1454269320Dhivya kothandanNessuna valutazione finora
- Abrus Precatorius L. Seed Extracts AntimicrobialDocumento4 pagineAbrus Precatorius L. Seed Extracts AntimicrobialDr. Varaprasad Bobbarala100% (1)
- Phytochemical and Pharmacological Screening of Combined Mimosa Pudica Linn and Tridax Procumbens For in Vitro Antimicrobial ActivityDocumento4 paginePhytochemical and Pharmacological Screening of Combined Mimosa Pudica Linn and Tridax Procumbens For in Vitro Antimicrobial Activityimyourfan2001Nessuna valutazione finora
- Sajp 42124 131Documento8 pagineSajp 42124 131syamsu nurNessuna valutazione finora
- TC 15025Documento4 pagineTC 15025MD MuntaharNessuna valutazione finora
- Antimicrobial Activity of Lemon Peel (Citrus Limon) Extract: Original ArticleDocumento4 pagineAntimicrobial Activity of Lemon Peel (Citrus Limon) Extract: Original ArticleFortunato Flojo IIINessuna valutazione finora
- Antifungal and Phytotoxic Properties of Crude Methanolic Extract and Various Fractions From Strobilanthes Urticifolia Wall. Ex KuntzeDocumento5 pagineAntifungal and Phytotoxic Properties of Crude Methanolic Extract and Various Fractions From Strobilanthes Urticifolia Wall. Ex KuntzeBaru Chandrasekhar RaoNessuna valutazione finora
- Phytochemical Screening, Quantitative Estimation of Total Phenolic, Flavanoids and Antimicrobial Evaluation of Trachyspermum AmmiDocumento8 paginePhytochemical Screening, Quantitative Estimation of Total Phenolic, Flavanoids and Antimicrobial Evaluation of Trachyspermum Ammijamonline100% (1)
- Preliminary Phytochemical and Antimicrobial Activity Studies On The Leaves of The Indian Plant Thevetia Neriifolia JussDocumento8 paginePreliminary Phytochemical and Antimicrobial Activity Studies On The Leaves of The Indian Plant Thevetia Neriifolia JussfahmatNessuna valutazione finora
- Matovu Henry. Phytochemical Profiling and Larvicidal Activity of Synadenium GrantiiDocumento8 pagineMatovu Henry. Phytochemical Profiling and Larvicidal Activity of Synadenium GrantiiJohn KakemboNessuna valutazione finora
- In Vitro Activity of Lawsonia Inermis (Henna) On Some Pathogenic FungiDocumento6 pagineIn Vitro Activity of Lawsonia Inermis (Henna) On Some Pathogenic FungiTuấn Nguyen AnhNessuna valutazione finora
- Ujmr 1 - 1 2016 - 009 PDFDocumento11 pagineUjmr 1 - 1 2016 - 009 PDFBahauddeen SalisuNessuna valutazione finora
- Asian Journal of ChemistryDocumento6 pagineAsian Journal of ChemistryDr. Sai Krushna PadhyNessuna valutazione finora
- Antecendes ProtuguesDocumento8 pagineAntecendes ProtuguesJho AnnaNessuna valutazione finora
- Evaluation of Antimicrobial Activities of Some Bangladeshi Medicinal PlantsDocumento6 pagineEvaluation of Antimicrobial Activities of Some Bangladeshi Medicinal PlantsJing ZangNessuna valutazione finora
- Phytochemical Screening and Anthelmintic Activity PDFDocumento4 paginePhytochemical Screening and Anthelmintic Activity PDFAdic KarNessuna valutazione finora
- Phytochemical Screening and Anthelmintic ActivityDocumento4 paginePhytochemical Screening and Anthelmintic ActivityAdic KarNessuna valutazione finora
- Kurinja KeeraiDocumento6 pagineKurinja Keeraimmarikar27Nessuna valutazione finora
- Antibacterial, Antifungal and Antitubercular Activity of Methanolic Extracts of Adansonia Digitata LDocumento9 pagineAntibacterial, Antifungal and Antitubercular Activity of Methanolic Extracts of Adansonia Digitata LIOSRjournalNessuna valutazione finora
- Antibakterijska Timus SerpilumDocumento2 pagineAntibakterijska Timus SerpilumNada PetrovićNessuna valutazione finora
- Antibacterial Activity of Acalypha Indica LDocumento4 pagineAntibacterial Activity of Acalypha Indica LMuhammad YusufNessuna valutazione finora
- Preliminary Phytochemical Screening, Quantitative Estimation and Evaluation of Antimicrobial Activity of Alstoniamacrophylla Stem BarkDocumento9 paginePreliminary Phytochemical Screening, Quantitative Estimation and Evaluation of Antimicrobial Activity of Alstoniamacrophylla Stem BarkInternational Journal of Science Inventions TodayNessuna valutazione finora
- Anti Amoebic and Phytochemical Screening of Some Congolese Medicinal PlantsDocumento9 pagineAnti Amoebic and Phytochemical Screening of Some Congolese Medicinal PlantsLuis A. CalderónNessuna valutazione finora
- Al Jadidi2016Documento4 pagineAl Jadidi2016Leandro DouglasNessuna valutazione finora
- Lack of Anthelmintic Activity of Kalanchoe Pinnata Fresh LeavesDocumento4 pagineLack of Anthelmintic Activity of Kalanchoe Pinnata Fresh Leavesphatak_rohan1983Nessuna valutazione finora
- 070117-PavanDocumento6 pagine070117-PavanSylviantie Adriana RosaNessuna valutazione finora
- Daodu, John OlabanjiDocumento44 pagineDaodu, John OlabanjiMovic IbNessuna valutazione finora
- Studies On Antimicrobial and Antioxidant Properties of Oyster MushroomDocumento6 pagineStudies On Antimicrobial and Antioxidant Properties of Oyster MushroomAKNessuna valutazione finora
- Comparative Study of The Quantitative Phytochemical Constituents and Antibacterial Activity of Five Tree SpeciesDocumento10 pagineComparative Study of The Quantitative Phytochemical Constituents and Antibacterial Activity of Five Tree SpeciesHuma RaoNessuna valutazione finora
- Hossain 2013Documento6 pagineHossain 2013Nur HudaNessuna valutazione finora
- 1 SMDocumento4 pagine1 SMAbraham YirguNessuna valutazione finora
- tmp9414 TMPDocumento8 paginetmp9414 TMPFrontiersNessuna valutazione finora
- The DoorDocumento3 pagineThe DoorAliah Necole EsquibelNessuna valutazione finora
- Wambugu PDFDocumento4 pagineWambugu PDFMauhibahYumnaNessuna valutazione finora
- Chapter One Introduction and Literature Review: Staphylococcus SP and Salmonella SPDocumento23 pagineChapter One Introduction and Literature Review: Staphylococcus SP and Salmonella SPOladimejiNessuna valutazione finora
- Comparative Efficacy of Herbal Essences With Amphotricin B and Ketoconazole On CandidaDocumento7 pagineComparative Efficacy of Herbal Essences With Amphotricin B and Ketoconazole On CandidaiisisiisNessuna valutazione finora
- Ashour2014 Article Anti-infectiveAndCytotoxicPropDocumento10 pagineAshour2014 Article Anti-infectiveAndCytotoxicPropamira PharmacienneNessuna valutazione finora
- Antimicrobial Activity of Plant Extracts ThesisDocumento4 pagineAntimicrobial Activity of Plant Extracts Thesiskimberlybundypittsburgh100% (1)
- Inhibitory Activity of Euphorbia Hirta Tawa Tawa Extracts Against Mycobacterium Tuberculosis and Other Non MycobacterialDocumento4 pagineInhibitory Activity of Euphorbia Hirta Tawa Tawa Extracts Against Mycobacterium Tuberculosis and Other Non MycobacterialArlene F. MontalboNessuna valutazione finora
- 2 51 1582878335 2ijmpsapr20202Documento10 pagine2 51 1582878335 2ijmpsapr20202TJPRC PublicationsNessuna valutazione finora
- Cytotoxic and Antimicrobial Activity of The Crude Extract of Abutilon IndicumDocumento4 pagineCytotoxic and Antimicrobial Activity of The Crude Extract of Abutilon IndicumApurba Sarker ApuNessuna valutazione finora
- PJB43 (5) 2613Documento5 paginePJB43 (5) 2613Leandro DouglasNessuna valutazione finora
- 1 PaperDocumento5 pagine1 PaperDr. Nilesh Baburao JawalkarNessuna valutazione finora
- Antifungal Activity of Selected Plant Leaves Crude Extracts Against A Pepper Anthracnose Fungus, (Ascomycota: Phyllachorales)Documento9 pagineAntifungal Activity of Selected Plant Leaves Crude Extracts Against A Pepper Anthracnose Fungus, (Ascomycota: Phyllachorales)MelanieNessuna valutazione finora
- Biological Activities of Extracts Obtained From Natural OriginDocumento5 pagineBiological Activities of Extracts Obtained From Natural OriginLeandro DouglasNessuna valutazione finora
- Phytochemical Analysis and Uses of Mimosa Pudica Linn. in ChhattisgarhDocumento4 paginePhytochemical Analysis and Uses of Mimosa Pudica Linn. in ChhattisgarhaisahNessuna valutazione finora
- tmpA4A TMPDocumento11 paginetmpA4A TMPFrontiersNessuna valutazione finora
- Calotropis Procera, Eichhornia Crassipes and Datura Innoxia LeavesDocumento4 pagineCalotropis Procera, Eichhornia Crassipes and Datura Innoxia LeavesSuhar TomiNessuna valutazione finora
- Anti-Bacterial and Anti-Fungal Activities of Various Extracts of Acanthospermum Hispidum DCDocumento4 pagineAnti-Bacterial and Anti-Fungal Activities of Various Extracts of Acanthospermum Hispidum DCEti ApriyantiNessuna valutazione finora
- In Vitro Antioxidant Antibacterial and ADocumento8 pagineIn Vitro Antioxidant Antibacterial and ANorlailaNessuna valutazione finora
- Antibacterial Activity Screening of Few Medicinal Plants From The Southern Region of IndiaDocumento4 pagineAntibacterial Activity Screening of Few Medicinal Plants From The Southern Region of IndiaDr. Varaprasad BobbaralaNessuna valutazione finora
- Phytochemical Screening and in Vitro Antimicrobial Activity of Typha Angustifolia Linn Leaves Extract Against Pathogenic Gram Negative Micro OrganismsDocumento4 paginePhytochemical Screening and in Vitro Antimicrobial Activity of Typha Angustifolia Linn Leaves Extract Against Pathogenic Gram Negative Micro Organismsumeshbt720Nessuna valutazione finora
- Ban Dot AnDocumento8 pagineBan Dot AnMaria Ina Dulce SNessuna valutazione finora
- IMJM Vol14No1 Page 77-81 in Vitro Antibacterial Activity of Eurycoma Longifolia PDFDocumento5 pagineIMJM Vol14No1 Page 77-81 in Vitro Antibacterial Activity of Eurycoma Longifolia PDFENjea LopiSma SPdieNessuna valutazione finora
- Alternanthera Philoxeroides (Mart.) GrisebDocumento4 pagineAlternanthera Philoxeroides (Mart.) GrisebRigotti Br100% (1)
- Pharmacology of Indian Medicinal PlantsDa EverandPharmacology of Indian Medicinal PlantsValutazione: 5 su 5 stelle5/5 (1)
- Homeopathy for Farm and Garden: The Homeopathic Treatment of Plants - 4th revised editionDa EverandHomeopathy for Farm and Garden: The Homeopathic Treatment of Plants - 4th revised editionNessuna valutazione finora
- Macerated, infusions, decoctions. Biodynamic preparations for the health of the garden and the vegetable garden.Da EverandMacerated, infusions, decoctions. Biodynamic preparations for the health of the garden and the vegetable garden.Nessuna valutazione finora
- Antibact AssayDocumento7 pagineAntibact Assaymakerk82Nessuna valutazione finora
- Antihypertensive Effects of Tannins Isolated FromDocumento13 pagineAntihypertensive Effects of Tannins Isolated Frommakerk82Nessuna valutazione finora
- "Effect of Bixin Isolated From Bixa Cardio NephrotoxicityDocumento11 pagine"Effect of Bixin Isolated From Bixa Cardio Nephrotoxicitymakerk82Nessuna valutazione finora
- 01 - Phosphate Buffer PDFDocumento1 pagina01 - Phosphate Buffer PDFmakerk82Nessuna valutazione finora
- Apset2016keyc 00 01a PDFDocumento1 paginaApset2016keyc 00 01a PDFmakerk82Nessuna valutazione finora
- Hong Kong PHD Fellowship Scheme - Research Grants CouncilDocumento7 pagineHong Kong PHD Fellowship Scheme - Research Grants Councilmakerk82Nessuna valutazione finora
- Basmati Rice Farming (Organic) Info GuideDocumento13 pagineBasmati Rice Farming (Organic) Info Guidemakerk82Nessuna valutazione finora
- Life Sciences Part 1 Csir JRF Net Gate DBTDocumento132 pagineLife Sciences Part 1 Csir JRF Net Gate DBTmakerk82100% (1)
- 599Documento9 pagine599makerk82Nessuna valutazione finora
- Food and Nutraceutical Regulations - SOSDocumento8 pagineFood and Nutraceutical Regulations - SOSmakerk82Nessuna valutazione finora
- 474RDocumento7 pagine474RsdNessuna valutazione finora
- 2011 Article 269Documento11 pagine2011 Article 269makerk82Nessuna valutazione finora
- Nutra World ArticleDocumento5 pagineNutra World ArticleAki EspaldonNessuna valutazione finora
- Inhibition of DNA Synthesis by Carvacrol in Mouse Myoblast Cells Bearing A Human N-RAS OncogeneDocumento8 pagineInhibition of DNA Synthesis by Carvacrol in Mouse Myoblast Cells Bearing A Human N-RAS Oncogenemakerk82Nessuna valutazione finora
- Marine Plant DrugsDocumento12 pagineMarine Plant Drugsmakerk82Nessuna valutazione finora
- 2112Documento22 pagine2112makerk82Nessuna valutazione finora
- 2012 Article 277Documento7 pagine2012 Article 277makerk82Nessuna valutazione finora
- Apjtb 04 08 627Documento6 pagineApjtb 04 08 627makerk82Nessuna valutazione finora
- 1 s2.0 S0367326X13003316 MainDocumento6 pagine1 s2.0 S0367326X13003316 Mainmakerk82Nessuna valutazione finora
- 1 s2.0 S0731708506007114 MainDocumento7 pagine1 s2.0 S0731708506007114 Mainmakerk82Nessuna valutazione finora
- Art:10.1007/s12272 013 0206 3Documento5 pagineArt:10.1007/s12272 013 0206 3makerk82Nessuna valutazione finora
- 1 s2.0 S1156523313001704 MainDocumento8 pagine1 s2.0 S1156523313001704 Mainmakerk82Nessuna valutazione finora
- Ni Hms 787119Documento15 pagineNi Hms 787119makerk82Nessuna valutazione finora
- 1 s2.0 S094471131100523X MainDocumento5 pagine1 s2.0 S094471131100523X Mainmakerk82Nessuna valutazione finora
- Isolation of Mangiferin and Amyloid Β-protein FromDocumento6 pagineIsolation of Mangiferin and Amyloid Β-protein Frommakerk82Nessuna valutazione finora
- Phytochemical and Pharmacological Investigations On MangiferinDocumento14 paginePhytochemical and Pharmacological Investigations On Mangiferinmakerk82Nessuna valutazione finora
- 1-Genome Islands TrainingDocumento2 pagine1-Genome Islands Trainingmakerk82Nessuna valutazione finora
- Bio-Oil Scars BookletDocumento11 pagineBio-Oil Scars Bookletmakerk82Nessuna valutazione finora
- Preparative Isolation and Purification of Four CompoundsDocumento6 paginePreparative Isolation and Purification of Four Compoundsmakerk82Nessuna valutazione finora
- Antimicrobial Evaluation of Mangiferin and Its Synthesized AnaloguesDocumento4 pagineAntimicrobial Evaluation of Mangiferin and Its Synthesized Analoguesmakerk82Nessuna valutazione finora
- Mindoro Island - Ethnopharmacologic Documentation of Selected Philippine Ethnolinguistic Ggroups The Mangyan (Alangan) People of Mindoro IslandDocumento17 pagineMindoro Island - Ethnopharmacologic Documentation of Selected Philippine Ethnolinguistic Ggroups The Mangyan (Alangan) People of Mindoro IslandAgatha AgatonNessuna valutazione finora
- MS Ijbpas 2018 44801Documento9 pagineMS Ijbpas 2018 44801Charlene Mae AlcaideNessuna valutazione finora
- (Paganga, 1997) The Identification of Flavonoids As Glycosides in Human PlasmaDocumento5 pagine(Paganga, 1997) The Identification of Flavonoids As Glycosides in Human PlasmaSie ningsihNessuna valutazione finora
- Drugs Containing Saponin GlycosidesDocumento46 pagineDrugs Containing Saponin GlycosidesMuhammed Faruk JambazNessuna valutazione finora
- Tawa Tawa: For Natural Health and WellnessDocumento4 pagineTawa Tawa: For Natural Health and WellnessJaja CarlinaNessuna valutazione finora
- Ijiit OnionDocumento8 pagineIjiit OnionSandeep GargNessuna valutazione finora
- Phytochemicals in Foods: Elisha Gay C. Hidalgo, RNDDocumento49 paginePhytochemicals in Foods: Elisha Gay C. Hidalgo, RNDinkpen56789100% (1)
- Bioactive Compounds: CarotenoidsDocumento4 pagineBioactive Compounds: CarotenoidsSaravana KumarNessuna valutazione finora
- DR Fuhrmans Cancer Fighting Diet FINALDocumento16 pagineDR Fuhrmans Cancer Fighting Diet FINALVirgiliu Teodorescu100% (1)
- Pigments in Fruits and Vegetables - Genomics and Dietetics (PDFDrive)Documento280 paginePigments in Fruits and Vegetables - Genomics and Dietetics (PDFDrive)abinaya100% (1)
- Orange Peel ProjectDocumento15 pagineOrange Peel ProjectSOMYAJULA KAVYANessuna valutazione finora
- Composicion de Fenoles y Carotenoides y Nutricional Facts de Main FruitsDocumento46 pagineComposicion de Fenoles y Carotenoides y Nutricional Facts de Main FruitsJuan Fernando Pineda GutierrezNessuna valutazione finora
- Structure-Antioxidant Activity Relationships of Phenols and FlavanoidsDocumento24 pagineStructure-Antioxidant Activity Relationships of Phenols and FlavanoidsThach NguyenNessuna valutazione finora
- Antioxidant Activity and Isolation of Xanthine Oxidase Inhibitor From Ruellia Tuberosa L. LeavesDocumento5 pagineAntioxidant Activity and Isolation of Xanthine Oxidase Inhibitor From Ruellia Tuberosa L. LeavesSandi VicoNessuna valutazione finora
- Acceptability of Kakawate Gliciridia Sepium Flower As A Commercial TeaDocumento58 pagineAcceptability of Kakawate Gliciridia Sepium Flower As A Commercial TeaAdiyanNessuna valutazione finora
- 2890 Manuscript 11889 1 10 20211209Documento10 pagine2890 Manuscript 11889 1 10 20211209Ratna RatiNessuna valutazione finora
- Pharmacogonostic and Phytochemical Properties of Aloe Vera.Documento14 paginePharmacogonostic and Phytochemical Properties of Aloe Vera.ABHINABA GUPTANessuna valutazione finora
- Lecture 3 GlycosidesDocumento18 pagineLecture 3 Glycosidessami ullahNessuna valutazione finora
- Total Antioxidant Capacity of Fruits: ArticleDocumento6 pagineTotal Antioxidant Capacity of Fruits: ArticleElfer Orlando Obispo GavinoNessuna valutazione finora
- Cyruta: Made From Buckwheat, Containing Powerful AntioxidantsDocumento2 pagineCyruta: Made From Buckwheat, Containing Powerful AntioxidantsVijay BhaskarNessuna valutazione finora
- Black Tea: of 14 Brands, 1 Failed The Pesticides TestDocumento10 pagineBlack Tea: of 14 Brands, 1 Failed The Pesticides TestKirtikaNessuna valutazione finora
- Ben's Trevo Presentation SlideDocumento69 pagineBen's Trevo Presentation SlideBenNessuna valutazione finora
- Herbal Drug Technology Practical Lab ManualDocumento51 pagineHerbal Drug Technology Practical Lab ManualPrasanthi BodduNessuna valutazione finora
- Functional Components of Cooked and Raw Banana Blossom (Decena, J.)Documento42 pagineFunctional Components of Cooked and Raw Banana Blossom (Decena, J.)Jas Decena100% (1)
- Journal of Food Composition and Analysis: E. Koh, K.M.S. Wimalasiri, A.W. Chassy, A.E. MitchellDocumento7 pagineJournal of Food Composition and Analysis: E. Koh, K.M.S. Wimalasiri, A.W. Chassy, A.E. MitchellAnonymous b2k9ABe7eNessuna valutazione finora
- Bawang ( - Sifat Etnomedisinal 3. Bawang ( - Sifat Etnomedisinal 3. Bawang ( - Sifat Etnomedisinal Dan TerapeutikDocumento8 pagineBawang ( - Sifat Etnomedisinal 3. Bawang ( - Sifat Etnomedisinal 3. Bawang ( - Sifat Etnomedisinal Dan TerapeutikRahmi KhoerunnisaNessuna valutazione finora
- Studies On The Insecticidal Properties of Chromolaena: Odorata (Asteraceae) Against Adult Stage of Periplaneta AmericanaDocumento4 pagineStudies On The Insecticidal Properties of Chromolaena: Odorata (Asteraceae) Against Adult Stage of Periplaneta AmericanaRicz PaulinoNessuna valutazione finora
- Antioxidant Activity and Melanin Inhibitory Effects of Yambean (Pachyrhizus Erosus) ExtractDocumento8 pagineAntioxidant Activity and Melanin Inhibitory Effects of Yambean (Pachyrhizus Erosus) ExtractFachrizal AuliaNessuna valutazione finora
- Extraction, Separation, Detection, and Structural Analysis of FlavonoidsDocumento26 pagineExtraction, Separation, Detection, and Structural Analysis of FlavonoidsHusnatul AyniahNessuna valutazione finora
- Acerola - Belwal - Potential Functional Food 2018Documento8 pagineAcerola - Belwal - Potential Functional Food 2018Reni WulansariNessuna valutazione finora