Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
What Clinical Audit
Caricato da
Wulan SuciCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
What Clinical Audit
Caricato da
Wulan SuciCopyright:
Formati disponibili
Clinical audit: what it is and what it isn t isnt
WHA T HAT
IS CLINICAL AUDIT?
What is clinical audit?
Clinical audit involves systematically looking at the procedures used for diagnosis, care and treatment, examining how associated resources are used and investigating the effect care has on the outcome and quality of life for the patient (Department of Health, 1993).
Audit is a word which has acquired different meanings over time in relation to health care quality. The above definition, provided by the Department of Health, emphasises the fact that clinical audit can be used to examine all aspects of patient care from assessment through to outcomes.
In brief, clinical audit provides a method for systematically reflecting on and reviewing practice
In the literature about clinical audit methods, the following terms are often mentioned: criteriabased audits; adverse occurrence screening; critical incident audits; peer reviews; and case note analysis. These are used inconsistently by different authors and tend to add to the general confusion about the clinical audit process. We would recommend ignoring this labyrinth of terminology since there is only one clinical audit method the clinical audit cycle. This method involves completing a number of stages and activities as described in chapter 2, Undertaking a clinical audit project.
There is only one clinical audit method the clinical audit cycle
WHY
IS CLINICAL AUDIT IMPORT ANT? IMPORTANT
There are a number of reasons why clinical audit is an important activity. The main reason is that it helps to improve the quality of the service being offered to users. Without some form of clinical audit, it is very difficult to know whether you are practising effectively and even more difficult to demonstrate this to others. The benefits of clinical audit are that it: identifies and promotes good practice and can lead to improvements in service delivery and outcomes for users can provide the information you need to show others that your service is effective (and cost-effective) and thus ensure its development provides opportunities for training and education helps to ensure better use of resources and, therefore, increased efficiency can improve working relationships, communication and liaison between staff, staff and service users, and between agencies.
The overarching aim of clinical audit is to improve service user outcomes by improving professional practice and the general quality of services delivered
WHA T HAT
AREAS CAN YOU
AUDIT?
There are numerous topics which are suitable and relevant for clinical audit. Several ways of subdividing clinical audit topic areas have been devised. A useful framework has been provided by Donabedian (1966) who classified topics under three headings: Structure The availability and organisation of resources and personnel. Process The activities undertaken, that is, what is done with the services resources.
Outcome The effect of the activities on the health/well-being of the service user, that is, changes for the individual which can be attributed to the clinical intervention they received.
HOW
MUCH TIME IS REQUIRED TO DO A CLINICAL AUDIT
PROJECT?
For some clinical audit projects, data collection, analysis and action plans can be carried out in an hour or two. Similarly these audit stages can take one or more years to complete. What is important is to design a clinical audit project which will produce meaningful data and which can be finished within the budget and time available. The most time-consuming element of any clinical audit project is the implementation of required changes. It is suggested that projects be kept simple and cover areas in which changes can be achieved.
Clinical audit can be both simple and quick
WHO
SHOULD BE INV OL VED IN THE CLINICAL AUDIT PROJECT? INVOL OLVED
A clinical audit project is more likely to be successful and beneficial to service users if all of the key stakeholders are involved from the outset. These may include: clinical and non-clinical staff providing the service service users people whose support may be required to implement resulting changes in practice (e.g. managers, referrers, trust board members).
As many of the above groups as possible should be represented on the clinical audit project team. If individuals are unable to attend team meetings, then they will need to be consulted and kept informed about the clinical audit project throughout the process.
Key stakeholders should be involved in the clinical audit project from the start
THE CLINICAL AUDIT PROJECT TEAM
A clinical audit project team works together from the early stages when decisions are being made about what to audit and how to design the audit. Roles and responsibilities within the team will need to be identified, for example audit project lead, data collector.
WHA T IS HAT AUDIT?
THE DIFFERENCE BETWEEN MEDICAL AND CLINICAL
What is clinical audit?
Clinical audit tends to be used as an umbrella term for any audit conducted by professionals in health care
Audits conducted by doctors are often referred to as medical audits, although the term clinical audits could also be used. It is important to stress that very few health care procedures involve just one professional discipline and that non-clinical staff such as receptionists, secretaries, porters, managers, etc. play a vital role in the quality of the service provided. Clinical audit, therefore, is usually a multi-disciplinary activity. Many clinical audits are also multi-sectoral, that is, they may involve health and social services, primary and acute care providers, education and health.
IS
SERVICE EV ALU ATION THE SAME AS CLINICAL AUDIT? EVALU ALUA
Service evaluation may be defined as:
A set of procedures to judge a services merit by providing a systematic assessment of its aims, objectives, activities, outputs, outcomes and costs (NHS Executive, 1997).
There are many different approaches to service evaluation. Whichever method is used, the process should provide practical information which helps to inform the future development of a service. Clinical audit may be one activity which takes place during a service evaluation, alongside other activities such as routine data gathering, incident reporting, and interviews with staff and service users. In order to conduct an evaluation, services need to consider their aims, objectives and then identify their key evaluation questions. Further texts to assist in service evaluation are listed at the end of this book.
HOW
DOES CLINICAL AUDIT DIFFER FROM RESEARCH?
Clinical audit is not research, but it does make use of research methodology in order to assess practice
Key differences between clinical audit and research are outlined in Table 1.1. Although research and clinical audit are two distinct activities with different purposes, they are interrelated in several ways, as described by Black (1992): Research provides a basis for defining good-quality care for clnical audit purposes. Clinical audit can provide high-quality data for non-experimental evaluative research. Research into the effectiveness and cost-effectiveness of clinical audit is needed. Research needs to be audited to ensure that high-quality work is performed.
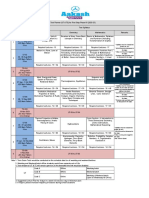
TABLE 1.1 Differences between research and clinical audit. Adapted from Madden (1991) and FirthCozens (1993) irth-Cozens RESEARCH Aims to establish what is best practice CLINICAL AUDIT Aims to evaluate how close practice is to best practice and to identify ways of improving the quality of health care provided Is specific and local to one results are not transferable Aims to improve services Is usually led by service providers Is practice -based practice-based Is an ongoing process Never involves allocating patients randomly to different treatment groups Never involves a placebo treatment Never involves a completely new treatment particular patient group to other settings
Is designed so that that its results can similar groups
it can be replicated and so be generalised to other
Aims to generate new knowledge/increase the sum of knowledge Is usually initiated by researchers Is theory driven Is often a one - off study oneMay involve allocating service users randomly to different treatment groups May involve administration of a placebo May involve a completely new treatment
EXAMPLES
OF DIFFERENT TYPES OF STUDIES IN AN IN-PATIENT
TING DISORDERS UNIT FOR ADOLESCENTS WITH EA EATING
A study to examine whether adolescents admitted to the unit benefit most from group or individual psychotherapy is research. A study to examine whether the following standard set by staff at the unit is being achieved: All adolescents admitted to the unit will receive a team assessment within two days of admission to decide whether they will receive group or individual psychotherapy , is a clinical audit project. A study involving: (a) collecting information about service users to see whether the service is reaching the target population, and (b) obtaining feedback from service users, referrers and providers about various aspects of the service (e.g. accessibility, acceptability, effectiveness) is a service evaluation.
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Tugas PPI SurveillanceDocumento12 pagineTugas PPI SurveillanceWulan SuciNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- 4d2a1 HD Adequacy Self StudyDocumento31 pagine4d2a1 HD Adequacy Self StudyWulan SuciNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Utpa Concussion Management Algorithm: When An Injury Occurs: Trainer Does Sideline Evaluation (Graded Symptoms Checklist)Documento1 paginaUtpa Concussion Management Algorithm: When An Injury Occurs: Trainer Does Sideline Evaluation (Graded Symptoms Checklist)Wulan SuciNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Integrated Care PathwaysDocumento64 pagineIntegrated Care Pathwaysseftiana1221Nessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Clearing Negative SpiritsDocumento6 pagineClearing Negative SpiritsmehorseblessedNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Windows SCADA Disturbance Capture: User's GuideDocumento23 pagineWindows SCADA Disturbance Capture: User's GuideANDREA LILIANA BAUTISTA ACEVEDONessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Approach To Vaginal Discharge in ChildrenDocumento12 pagineApproach To Vaginal Discharge in ChildrensujataNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- AIM Mag Issue 22 April 2010Documento98 pagineAIM Mag Issue 22 April 2010Artisans in Miniature95% (19)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Welcome LetterDocumento2 pagineWelcome Letterapi-348364586Nessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- 576 1 1179 1 10 20181220Documento15 pagine576 1 1179 1 10 20181220Sana MuzaffarNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- FMEA 4th BOOK PDFDocumento151 pagineFMEA 4th BOOK PDFLuis Cárdenas100% (2)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Shielded Metal Arc Welding Summative TestDocumento4 pagineShielded Metal Arc Welding Summative TestFelix MilanNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- tf00001054 WacDocumento22 paginetf00001054 WacHritik RawatNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Robot MecanumDocumento4 pagineRobot MecanumalienkanibalNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Becoming FarmersDocumento13 pagineBecoming FarmersJimena RoblesNessuna valutazione finora
- PMS Past Paper Pakistan Studies 2019Documento3 paginePMS Past Paper Pakistan Studies 2019AsmaMaryamNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- E TN SWD Csa A23 3 94 009 PDFDocumento5 pagineE TN SWD Csa A23 3 94 009 PDFRazvan RobertNessuna valutazione finora
- Your Free Buyer Persona TemplateDocumento8 pagineYour Free Buyer Persona Templateel_nakdjoNessuna valutazione finora
- Counselling Goes To The Movies: Antwone Fisher (2002)Documento12 pagineCounselling Goes To The Movies: Antwone Fisher (2002)Azizul MohamadNessuna valutazione finora
- Marketing PlanDocumento41 pagineMarketing PlanMark AbainzaNessuna valutazione finora
- ObliCon Digests PDFDocumento48 pagineObliCon Digests PDFvictoria pepitoNessuna valutazione finora
- Joshua 24 15Documento1 paginaJoshua 24 15api-313783690Nessuna valutazione finora
- Mathsnacks05 InfiniteDocumento1 paginaMathsnacks05 Infiniteburkard.polsterNessuna valutazione finora
- 1973 PorbaixM LEC PDFDocumento351 pagine1973 PorbaixM LEC PDFDana Oboroceanu100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Hercules Industries Inc. v. Secretary of Labor (1992)Documento1 paginaHercules Industries Inc. v. Secretary of Labor (1992)Vianca MiguelNessuna valutazione finora
- Lewin's Change ManagementDocumento5 pagineLewin's Change ManagementutsavNessuna valutazione finora
- UT & TE Planner - AY 2023-24 - Phase-01Documento1 paginaUT & TE Planner - AY 2023-24 - Phase-01Atharv KumarNessuna valutazione finora
- Nielsen & Co., Inc. v. Lepanto Consolidated Mining Co., 34 Phil, 122 (1915)Documento3 pagineNielsen & Co., Inc. v. Lepanto Consolidated Mining Co., 34 Phil, 122 (1915)Abby PajaronNessuna valutazione finora
- Julie Jacko - Professor of Healthcare InformaticsDocumento1 paginaJulie Jacko - Professor of Healthcare InformaticsjuliejackoNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiDocumento6 paginePaediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiharnizaNessuna valutazione finora
- Springfield College Lesson Plan Template PHED 237: The Learning and Performance of Physical ActivitiesDocumento5 pagineSpringfield College Lesson Plan Template PHED 237: The Learning and Performance of Physical Activitiesapi-285421100Nessuna valutazione finora
- Theater 10 Syllabus Printed PDFDocumento7 pagineTheater 10 Syllabus Printed PDFJim QuentinNessuna valutazione finora
- A Photograph (Q and Poetic Devices)Documento2 pagineA Photograph (Q and Poetic Devices)Sanya SadanaNessuna valutazione finora
- Is 13779 1999 PDFDocumento46 pagineIs 13779 1999 PDFchandranmuthuswamyNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)