Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Em Article C Diff
Caricato da
sgod34Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Em Article C Diff
Caricato da
sgod34Copyright:
Formati disponibili
Player With a New Hand in the Game
Treatments for C difficile, an increasingly common infection among hospitalized patients, range from antibiotic withdrawal and administration of antimicrobials in traditional, pulsed, or tapered regimens to colectomy for fulminant disease and novel approaches such as fecal transplantation for recurrent episodes.
Clostridium difficile: An Old
James D. Morris, MD, and Fred A. Lopez, MD, FACP
lostridium difficile has emerged as a major nosocomial pathogen for patients undergoing antibiotic therapy and receiving inpatient hospital or institutionalized care. At particular risk are those in the elderly population. Since 2000, the number of cases of C difficile, as well as the disease-associated financial burden, has grown enormously. Preventing, recognizing, and combating this disease process is paramount for all health care organizations, particularly in the ED, as it is the gateway to hospital care.1
12
EMERGENCY MEDICINE | NOVEMBER 2009
www.emedmag.com
2009 Scott Bodell
Dr. Morris is an instructor of clinical medicine in the section of gastroenterology and hepatology at the Tulane University Health Sciences Center, Southeast Louisiana Veterans Affairs Healthcare System, and Louisiana State University Health Sciences Center in New Orleans. Dr. Lopez is the Richard Vial Professor and vice chair in the department of medicine, section of infectious diseases at the Louisiana State University Health Sciences Center in New Orleans.
C difficile infection (CDI) is the recommended terminology for C difficileinduced disease, which encompasses pseudomembranous colitis or antibiotic-associated diarrhea. Recent literature indicates that CDI costs the US health care system more than $1.1 billion each year, with approximately 15% to 20% of hospitalized patients becoming infected.2,3 The overall incidence of the disease has been increasing at a substantial rate, as documented by multiple epidemiologic studies in the United Kingdom, Canada, and the United States. A particularly virulent strain has emerged in Quebec and in the United States (specifically Georgia, Illinois, Maine, New Jersey, Oregon, and Pennsylvania), resulting in a significant increase in mortality.4,5 C difficile virulent strain NAP-1/027, which appears to have increased toxin A/B production, fluoroquinolone resistance, and production of binary toxin, has been associated with severe infection and
CLOSTRIDIUM DIFFICILE
high mortality. Fluoroquinolone use has greatly expanded in recent years, due to the agents broad spectrum of activity and the ease of once- or twicedaily administration. Use of any class of antibiotic with antibacterial activity constitutes a theoretical risk factor for CDI, although, historically, clindamycin, aminopenicillins, and cephalosporins have had the strongest associations.6,7 C difficile is an anaerobic, gram-positive, sporeforming, toxin-producing bacillus transmitted among humans via the fecal-oral route.8 The bacteria are typically transmitted in hospitals. Alcohol-based rubs/gels have little or no activity against the spores of C difficile. Additional risk factors for C difficile colonization include older age (nursing home or rehabilitation center admission), antibiotic use, bowel surgery,9 use of a feeding tube, and chemotherapy (rarely methotrexate). Children up to age 18 months may be carriers of the organism (up to 60% to 70% are colonized); however, colitis rarely develops.2 Colonization usually disappears within a few months and is thought to result from a lack of receptors for C difficileassociated toxins.10 Inanimate objects in a patients room may harbor the acid- and antibiotic-resistant spores for weeks to months, thus necessitating comprehensive cleansing of contaminated spaces in health care facilities. Acid suppression has an unclear role in CDI, with conflicting data supporting or refuting its association with infections. Inflammatory bowel disease also appears to be a risk factor for superimposed infection, and its presence together with active inflammation may also make it difficult to detect CDI on endoscopy.11 To control CDI, the following precautions are paramount: contact isolation (with patients in a single room and no sharing of bathrooms), wearing gloves, washing hands with soap and water, terminal room cleaning with 1:10 household bleach, avoidance of use of rectal thermometers, decreased length of hospitalization, decreased antibiotic usage, and early isolation of suspected infected patients.10,12 CLINICAL PRESENTATION Presentation varies from mild symptoms to severe toxic colitis.2 Diarrhea can range from a nuisance to more than 20 watery bowel movements daily. Crampy lower quadrant abdominal pain may be present in addition to variable degrees of fever. Leukocytosis (particularly >20,000 leukocytes/mm3) may also be present and, when it appears with renal dysfunction (elevated crewww.emedmag.com
TABLE 1. Risk Factors for Severe
Clostridium difficile Infection
Severe diarrhea High fever, >38.9 C High leukocytosis (>20,000 leukocytes/ mm3) Renal failure Ileus Age >60 years
Albumin <2.5 mg/dL Pseudomembranous colitis
Data extracted from Leffler and LaMont.2
atinine), may lead to a higher risk for severe colitis and increased mortality (Table 1).2 CDI is a protein-losing enteropathy that can result in low serum albumin levels. In more severe disease, pseudomembranous colitis may develop with characteristic white plaques scattered throughout the colon and sometimes even the small intestine. In the worst cases, a fulminant colitis may develop. Perforation is rare. Fecal leukocytes are commonly present but provide only a general clue to an infectious or inflammatory etiology.13 CLINICAL DIAGNOSIS CDI can generally be diagnosed using both clinical and laboratory information. The use of radiologic imaging (CT) or endoscopic evaluation is usually not required. Stool cytotoxicity assays initially were introduced for the detection of CDI; however, they have largely been replaced by enzyme immunoassays. Detection of both toxins A and B is suggested, as a small number of strains will produce only cytotoxin >>FAST TRACK<< B.14 These newer tests may In the presence of strong lack the sensitivity/speciclinical suspicions in ficity of earlier cytotoxicity acutely ill patients, assays. In the presence of therapy for CDI should strong clinical suspicions in be initiated early, even acutely ill patients, therapy if immunoassays are for CDI should be initiated negative. early, even if immunoassays are negative. Stool culture using special media may also be performed, but this technique is limited to only a few specialized centers and is most useful in epidemiologic studies. As this infection becomes more endemic, suspected CDI should prompt only one immunoassay, as the majority of the first samples
NOVEMBER 2009 | EMERGENCY MEDICINE 13
CLOSTRIDIUM DIFFICILE
will be positive. The diagnostic yield of repeated enzyme immunoassays is low and leads to unnecessary expense.15 Radiologic examination with plain films or cross-sectional imaging (CT) may provide supportive evidence of infection and prove valuable in patients presenting with fulminant colitis. Severe disease is suggested on CT by colonic wall-thickening, colonic dilation, and ascites.16 TREATMENT
General Issues
Not all patients with positive immunoassay results and clinical evidence of symptoms require therapy. Withdrawal of an antimicrobial agent may lead to eradication of CDI in a quarter of cases but should be limited to the mildest cases. However, most patients present with acute disease and require antibiotic treatment. Toxin-binding resins and probiotics have not definitively been proven as effective treatment. Cholestyramine binds vancomycin in the gastrointestinal (GI) tract, ie, decreasing the effectiveness of vancomycin and requiring a 2- to 3-hour alternating period between drug administrations. In addition, drugs that impair GI motility, including narcotics, should be avoided.2
Antibiotic Issues
significant in patients with mild infection (P=.36) but achieved significance in favor of vancomycin for those with severe infection (P=.02).19 For the first recurrence of CDI, the patient should be re-treated with the original drug (ie, oral vancomycin or oral metronidazole).1 Oral vancomycin has minimal side effects, although patients may experience gastric upset and nausea. Side effects associated with parenteral administration, including ototoxicity, nephrotoxicity, and red man syndrome, have not been observed with oral dosing. Metronidazoles side effects include headache, nausea, metallic taste, and a disulfiram-like effect when alcohol is ingested. Prolonged exposure to metronidazole (>1 month) may cause a potentially irreversible neuropathy.2
Fulminant Disease
Antibiotics are usually curative, although severe cases may necessitate a colectomy (Table 2).1,2,16,17 Initial choice of antibiotic therapy continues to generate much discussion. Oral metronidazole (500 mg 3 times a day or 250 mg 4 times a day for 10 to 14 days) has historically been the initial choice for treatment of CDI18; however, oral vancomycin (125 mg 4 times a day for 10 to 14 days) is >>FAST TRACK<< the only agent approved by the FDA for the treatment For the first recurrence of CDI, the patient should of this condition. Metronidazoles lower cost provides be re-treated with the an argument for its initial original drug (ie, oral use in mild disease, but vancomycin or oral recent studies suggest that metronidazole). the drug is less efficacious than vancomycin. Use of vancomycin may promote the development of vancomycin-resistant enterococci, but resistance has also been noted with metronidazole. Studies supporting initial therapy with vancomycin are emerging. In one series, the difference in response rates between vancomycin and metronidazole was not
14 EMERGENCY MEDICINE | NOVEMBER 2009
In those patients with severe disease represented by a leukemoid reaction, renal dysfunction, ileus, inability to tolerate oral intake, and/or high fever, ICU admission should be considered. Diarrhea may be absent in some of these cases, thereby complicating the ability to make a diagnosis. Early surgical evaluation should be considered in patients with fulminant disease. Functionality of the gut should be assessed within 24 to 48 hours of presentation, and clinical improvement should be expected in 3 to 5 days.16 The functionality of the GI tract is an important consideration when determining whether oral antibacterial agents can be administered to a patient. In patients with a functional GI tract who are unable to tolerate oral intake, a nasogastric tube may be used for delivery of metronidazole or vancomycin. If ileus is present, vancomycin administered by enema may be considered (0.5 to 1.0 g in 100 to 200 mL normal saline given as a retention enema with the rectal tube clamped for 60 minutes every 4 to 12 hours). Adjunctive IV metronidazole may also be given; however, less than 15% of the IV dose is excreted via the fecal route; thus, this treatment may have limited efficacy in the presence of ileus. Surgical treatment is indicated in patients with signs of organ failure, shock, vasopressor dependence for hemodynamic stability, worsening signs on CT, peritonitis, bowel perforation, clinical worsening, or lack of response within 72 hours (or sooner if morbidity is more severe). Delays in diagnosis and treatment increase mortality. Currently, total abdominal colectomy with end ileostomy is the operative procedure
www.emedmag.com
CLOSTRIDIUM DIFFICILE
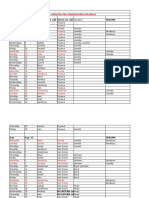
TABLE 2. Antimicrobial Therapy Strategy Choices for
Clostridium difficile Infection
All Cases: Stop or change antibiotics, use supportive therapy, enforce infection control precautions, isolate patient Mild Disease Metronidazole 500 mg orally 3 times daily for 1014 days with daily assessments Severe Disease For patients with a functional GI tract Vancomycin 125 mg oral/nasogastric tube 4 times daily for 1014 days with daily assessment metronidazole 500 mg IV every 6 hours for 10 days For patients with ileus Vancomycin 500 mg in 100200 mL normal saline as retention enema clamped for 60 minutes every 412 hours for up to 10 days metronidazole 500 mg IV every 6 hours for 10 days Early surgical evaluation for colectomy Infectious disease consultation Possible gastroenterology consultation for colonoscopy No response or worsening of symptoms in 7 days Vancomycin 125 mg orally 4 times daily for 1014 days Infectious disease consultation Gastroenterology consultation Possible surgical referral if severe symptoms (leukocytosis, renal dysfunction, ileus, hypotension) No response or worsening of symptoms in 72 hours Daily assessment Colectomy If colectomy not warranted, vancomycin 500 mg orally every 6 hours up to 1014 days Consider IVIG, 400 mg/kg
GI=gastrointestinal; IV=intravenous; IVIG = intravenous immunoglobulin Data extracted from Kelly and LaMont1; Leffler and LaMont2; Jaber et al16; Gerding et al.17
of choice for fulminant CDI. The reported mortality rate in surgical treatment of CDI ranges from 30% to 80%.16
Recurrent Disease
Approximately 20% of patients will develop a recurrence of symptomatic CDI.1,2,16,17 Older patients and those with a history of CDI recurrence are at increased risk. Most recurrences occur shortly after the end of therapy (ie, 7 to 14 days). Repeat exposure to C difficile spores or lack of eradication of the bacteria can lead to these repeat episodes. Host immunity also contributes to recurrent disease. Development of immunoglobulin G antitoxin A at high levels appears to be protective for recurrent disease, while
www.emedmag.com
low levels may confer risk for recurrent disease.1 Failure to achieve eradication with the same antibiotic following the second course of treatment should prompt reevaluation of the patient. Stool immunoassay studies for C difficile toxins should be repeated, as postinfectious irritable bowel syndrome and other bacterial infections may have similar presentations. Antimicrobial resistance to vancomycin has not been reported, and resistance to metronidazole is rare.17 In recurrent CDI, regimens with tapering or pulsed vancomycin administration resulted in fewer recurrences, with recurrence rates of 31% (P=.01) for tapering and 14.3% (P=.02) for pulsed administration when compared to standard metronidazole or vancomycin treatments.1 Table 3 shows treatment strategies
NOVEMBER 2009 | EMERGENCY MEDICINE 15
CLOSTRIDIUM DIFFICILE
TABLE 3. Treatment Strategies for refractory Clostridium difficile Infections
Initial Recurrence Repeat regimen of metronidazole 500 mg orally 3 times daily for 1014 days OR Vancomycin 125 mg orally 4 times a day for 1014 days (severe disease or intolerant of metronidazole) Second Recurrence Taper regimenVancomycin 125 mg orally 4 times daily for 7 days, 125 mg 2 times daily for 7 days, 125 mg once daily for 7 days, 125 mg once every 2 days for 8 days, and 125 mg once every 3 days for 15 days Pulse regimenVancomycin 125 mg orally 4 4 times daily for 14 days, then 125 mg 3 times a week for an additional 4 weeks
Third Recurrence Vancomycin 125 mg orally 4 times daily for 14 days with a subsequent change in therapy to rifaximin 400 mg twice daily for 14 days Additional Recurrences IVIG 400 mg/kg every 3 weeks for 3 doses, fecal transplantation therapy, rifaximin, nitazoxanide, probiotics, suppressive therapy with oral vancomycin for elderly patients and those with multiple comorbidities
IVIG = intravenous immunoglobulin Data extracted from Kelly and LaMont1; Leffler and LaMont2; Jaber et al16; Gerding et al.17
for refractory disease.1,2,16,17 In one oral vancomycin tapering strategy, doses of 125 mg are given every 6 hours for 7 days, then 125 mg every 12 hours for 7 days, then 125 mg daily for 7 days, then 125 mg every other day for 8 days, and finally 125 mg every 3 days for 15 days. Another pulsed-dose regimen comprising oral vancomycin 125 mg every 6 hours for the initial 2 weeks followed by 125 mg 3 times a week for an additional 4 weeks has been successful in treating some cases of CDI recurrence.2,11,17,20
Multiple Recurrences and Resistant Disease
also been considered for use in controlling recurrent CDI but are not FDA approved for this indication.17 Fecal transplantation therapy using a blended fecal filtrate (usually, donated stool from a relative) with delivery via colonoscope or nasogastric tube has also been reported to be effective. In patients with severe CDI that is refractory to medical therapy, immunoglobulin therapy at a dose of 400 mg/kg IV every 3 weeks for three doses can be considered.1 CONCLUSION Nosocomial C difficile infections have become a major issue for patients in residential health care settings and hospitals; C difficile also affects patients who have been treated with antibiotics in the recent past. Although resistance to metronidazole and vancomycin is not common, novel epidemic strains of C difficile that are associated with greater morbidity and mortality are emerging. Consistent infection control measures are imperative to prevent spread of CDI. Recognition of fulminant disease early in the course of infectionalong with resultant implementation of more aggressive supportive measures, use of oral vancomycin for severe disease, and early
www.emedmag.com
For multiple recurrences of CDI, the disease process can be disabling and require alternative approaches to treatment. Probiotics have been used in the prevention of antibiotic-associated diarrhea; however, efficacy data for Lactobacillus and Saccharomyces boulardii for prevention of CDI are mixed. Used as monotherapy, none of the probiotics has been shown to be effective in treating CDI, but these agents may be considered as adjunctive therapy. A slight risk for bacteremia or fungemia exists with the use of probiotics in critically ill, immunocompromised patients. Rifaximin and nitazoxanide have
16 EMERGENCY MEDICINE | NOVEMBER 2009
CLOSTRIDIUM DIFFICILE
surgical consultation for possible colectomyimproves survival rates for patients with severe CDI. For recurrent disease, retreatment with vancomycin or metronidazole is effective; however, additional recurrences of CDI may require novel approaches. Q The views expressed in this article are those of the authors and do not necessarily reflect those of the US government or any of its agencies. Work completed on this article is independent of Dr. Morris capacity as a federal employee.
REFERENCES
1. 2. 3. Kelly CP, LaMont JT. Clostridium difficile--more difficult than ever. N Engl J Med. 2008;359(18):1932-1940. Leffler DA, LaMont JT. Treatment of Clostridium difficile-associated disease. Gastroenterology. 2009;136(6):1899-1912. Kyne L, Hamel MB, Polavaram R, Kelly CP. Health care costs and mortality associated with nosocomial diarrhea due to Clostridium difficile. Clin Infect Dis. 2002;34(3):346-353. Loo VG, Poirier L, Miller MA, et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med . 2005;353(23):2442-2449. McDonald LC, Killgore GE, Thompson A, et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005;353(23):2433-2441. OConnor JR, Johnson S, Gerding DN. Clostridium difficile infection caused by the epidemic BI/NAP1/027 strain. Gastroenterology. 2009;136(6):1913-1924. Ppin J, Saheb N, Coulombe M, et al. Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin Infect Dis. 2005;41(9):1254-1260.
8.
9.
10.
11. 12.
13. 14. 15.
16.
4.
17. 18.
5.
6.
19.
7.
20.
Elmer GW, Surawicz CM, McFarland LV. Biotherapeutic agents. A neglected modality for the treatment and prevention of selected intestinal and vaginal infections. JAMA. 1996;275(11):870-876. Gerding D, Muto C, Owens RJ Jr. Measures to control and prevent Clostridium difficile infection. Clin Infect Dis. 2008;46(suppl 1): S43-S49. Fekety R. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 1997;92(5):739-750. Surawicz CM. Reining in recurrent Clostridium difficile infection-whos at risk? Gastroenterology. 2009;136(4):1152-1154. Bartlett JG. Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med. 2006;145(10):758-764. Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med. 2002;346(5):334-339. Bartlett JG. Historical perspectives on studies of Clostridium difficile and C. difficile infection. Clin Infect Dis. 2008;46(suppl 1):S4-S11. Nemat H, Khan R, Ashraf MS, et al. Diagnostic value of repeated enzyme immunoassays in Clostridium difficile infection. Am J Gastroenterol. 2009;104(8):2035-2419. Jaber MR, Olafsson S, Fung WL, Reeves ME. Clinical review of the management of fulminant clostridium difficile infection. Am J Gastroenterol. 2008;103(12):3195-3203. Gerding DN, Muto CA, Owens RC Jr. Treatment of Clostridium difficile infection. Clin Infect Dis. 2008;46(suppl 1):S32-S42. Nelson R. Antibiotic treatment for Clostridium difficile-associated diarrhea in adults. Cochrane Database Syst Rev. 2007;(3): CD004610. Zar FA, Bakkanagari SR, Moorthi KM, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45(3):302-307. Aslam S, Hamill RJ, Musher DM. Treatment of Clostridium difficileassociated disease: old therapies and new strategies. Lancet Infect Dis. 2005;5(9):549-557.
www.emedmag.com
NOVEMBER 2009 | EMERGENCY MEDICINE
17
Potrebbero piacerti anche
- Sample Questions: American Board of Medical MicrobiologyDocumento8 pagineSample Questions: American Board of Medical Microbiologyelattar.laila1891Nessuna valutazione finora
- Eye MCQs For UndergraduatesDocumento15 pagineEye MCQs For UndergraduatesZeeshan AbdulNasir100% (4)
- Absite Review VascularDocumento183 pagineAbsite Review Vascularsgod34Nessuna valutazione finora
- Clostridium Botulinum - Ecology and Control in Foods (1993)Documento762 pagineClostridium Botulinum - Ecology and Control in Foods (1993)RhynoHD100% (1)
- Medical English Vocabulary: Nurses and Medical ProfessionalsDocumento15 pagineMedical English Vocabulary: Nurses and Medical ProfessionalsEchan MitnickNessuna valutazione finora
- A Brief History of TattoosDocumento14 pagineA Brief History of TattoosramonxvsNessuna valutazione finora
- Medical Virology, IntroductionMedical VirologyDocumento88 pagineMedical Virology, IntroductionMedical Virologytummalapalli venkateswara rao100% (4)
- Antibiotic-Associated ColitisDocumento10 pagineAntibiotic-Associated ColitisHendraGusmawanNessuna valutazione finora
- C Diff PDFDocumento6 pagineC Diff PDFBobNessuna valutazione finora
- Nneoma Odoemena Preceptor Richard Williams February 23, 2018Documento3 pagineNneoma Odoemena Preceptor Richard Williams February 23, 2018Nneoma OdoemenaNessuna valutazione finora
- Clostridium Difficile: Isolation of The Hospitalized Patient: Control MeasuresDocumento5 pagineClostridium Difficile: Isolation of The Hospitalized Patient: Control MeasuresSizi DiazNessuna valutazione finora
- Practice - Parameter - Clostridium - Difficile - InfectionDocumento15 paginePractice - Parameter - Clostridium - Difficile - InfectionIfeanyichukwu OgbonnayaNessuna valutazione finora
- Clostridioides No IdosoDocumento14 pagineClostridioides No IdosoSCIH HFCPNessuna valutazione finora
- Physical, Laboratory, Radiographic, and Endoscopic Workup For Clostridium Difficile ColitisDocumento5 paginePhysical, Laboratory, Radiographic, and Endoscopic Workup For Clostridium Difficile ColitisJoaquin Martinez HernandezNessuna valutazione finora
- Clostridium DifficileDocumento9 pagineClostridium DifficileRita della ValentiniNessuna valutazione finora
- Cis 551Documento8 pagineCis 551Lina Mahayaty SembiringNessuna valutazione finora
- Third Case Report Pseudomembranous Colitis Dr. Lisa FarianiDocumento18 pagineThird Case Report Pseudomembranous Colitis Dr. Lisa FarianirizkyauliautamaNessuna valutazione finora
- Uti - HarriDocumento9 pagineUti - HarrilololoNessuna valutazione finora
- Toxic Megacolon - A Three Case PresentationDocumento6 pagineToxic Megacolon - A Three Case PresentationsytaNessuna valutazione finora
- Cadazolid: A New Hope in The Treatment of Clostridium Difficile InfectionDocumento10 pagineCadazolid: A New Hope in The Treatment of Clostridium Difficile InfectionMaria KNessuna valutazione finora
- Crohn 1 EspDocumento8 pagineCrohn 1 EspRomina GonzálezNessuna valutazione finora
- Clostridium Difficile-Associated Diarrhea in The Oncology PatientDocumento7 pagineClostridium Difficile-Associated Diarrhea in The Oncology PatientK. O.Nessuna valutazione finora
- Czepiel2019 Article ClostridiumDifficileInfectionRDocumento11 pagineCzepiel2019 Article ClostridiumDifficileInfectionRLucas MontanhaNessuna valutazione finora
- Update Cdiff InfxnDocumento10 pagineUpdate Cdiff Infxnapi-83223044Nessuna valutazione finora
- Clostridium Difficile EpidemiologyDocumento36 pagineClostridium Difficile EpidemiologyIsha BhattNessuna valutazione finora
- C Difficile DiarrheaDocumento12 pagineC Difficile DiarrheaSi vis pacem...Nessuna valutazione finora
- Clostridium Difficile Infection. Review. European Journal of Clinical Microbiology and Infectious Diseases.Documento11 pagineClostridium Difficile Infection. Review. European Journal of Clinical Microbiology and Infectious Diseases.LibrosNessuna valutazione finora
- Clostridium Difficile ColitisDocumento33 pagineClostridium Difficile ColitisLaura Anghel-MocanuNessuna valutazione finora
- Pseudomembranouse ColitisDocumento37 paginePseudomembranouse ColitisFitria FieraNessuna valutazione finora
- Nejmra1315399invasive Candidiasisoct8-2015Documento12 pagineNejmra1315399invasive Candidiasisoct8-2015kendyNessuna valutazione finora
- Pediatric For KidsDocumento6 paginePediatric For KidsOasis LimitedNessuna valutazione finora
- Pi Is 1542356506013279Documento7 paginePi Is 1542356506013279rezzaready_815773768Nessuna valutazione finora
- Geriatric C Diff Diarrhea CaseDocumento7 pagineGeriatric C Diff Diarrhea CaseStarr NewmanNessuna valutazione finora
- Inflammatory Bowel Disease .. Last EditDocumento22 pagineInflammatory Bowel Disease .. Last EditRashed ShatnawiNessuna valutazione finora
- Internal Medicine Journal - 2020 - Gilmore - Cytomegalovirus in Inflammatory Bowel Disease A Clinical ApproachDocumento4 pagineInternal Medicine Journal - 2020 - Gilmore - Cytomegalovirus in Inflammatory Bowel Disease A Clinical ApproachDiego Fernando Ortiz TenorioNessuna valutazione finora
- Ulcerative Colitis: An Update: Authors: Jonathan P SegalDocumento5 pagineUlcerative Colitis: An Update: Authors: Jonathan P SegalManoel Victor Moreira MachadoNessuna valutazione finora
- Oropharyngeal Candidiasis: Review of Its Clinical Spectrum and Current TherapiesDocumento18 pagineOropharyngeal Candidiasis: Review of Its Clinical Spectrum and Current TherapiesDelbert GradyNessuna valutazione finora
- Hyaluronic Acid For Colitis Treatment Revision 5Documento16 pagineHyaluronic Acid For Colitis Treatment Revision 5Shabrina MaharaniNessuna valutazione finora
- Etiology and Evaluation of Diarrhea in AIDS: A Global Perspective at The MillenniumDocumento10 pagineEtiology and Evaluation of Diarrhea in AIDS: A Global Perspective at The MillenniumSri Nowo MinartiNessuna valutazione finora
- Colitis UlcerativaDocumento20 pagineColitis UlcerativaMargareth Vargas BéjarNessuna valutazione finora
- 2019 Article 3539.en - EsDocumento11 pagine2019 Article 3539.en - EsJuan CuaNessuna valutazione finora
- Invasivecandidiasis: Todd P. Mccarty,, Peter G. PappasDocumento22 pagineInvasivecandidiasis: Todd P. Mccarty,, Peter G. PappasAnonymous By8a7sArRNessuna valutazione finora
- Clostridioides Difficile Infection in Patients WitDocumento10 pagineClostridioides Difficile Infection in Patients WitElena Cuiban100% (1)
- Hospital Infection Control: Clostridioides Difficile: Nicholas A. Turner, MD, MHSC Deverick J. Anderson, MD, MPHDocumento10 pagineHospital Infection Control: Clostridioides Difficile: Nicholas A. Turner, MD, MHSC Deverick J. Anderson, MD, MPHJoaquin Martinez HernandezNessuna valutazione finora
- 10.1038@s41572 020 0205 XDocumento20 pagine10.1038@s41572 020 0205 XJesús Cortés HernándezNessuna valutazione finora
- Case Files 6 ClostridiaDocumento4 pagineCase Files 6 ClostridiaAHMAD ADE SAPUTRANessuna valutazione finora
- Toxic Megacolon: Daniel M. Autenrieth, MD, and Daniel C. Baumgart, MD, PHDDocumento8 pagineToxic Megacolon: Daniel M. Autenrieth, MD, and Daniel C. Baumgart, MD, PHDGoran TomićNessuna valutazione finora
- Crohns Epidemio Diagnositco y TratamientoDocumento16 pagineCrohns Epidemio Diagnositco y TratamientoSantiago ZamudioNessuna valutazione finora
- Acute Pancreatitis Diagnosis and TreatmentDocumento27 pagineAcute Pancreatitis Diagnosis and TreatmentkarlosNessuna valutazione finora
- Clostridium Caso ControlDocumento9 pagineClostridium Caso Controlmexivergas mustNessuna valutazione finora
- Clostridium 1Documento7 pagineClostridium 1Ioana AntonesiNessuna valutazione finora
- Clostridium Difficile InfectionDocumento10 pagineClostridium Difficile Infectionaj2713Nessuna valutazione finora
- Final Paper BiologyDocumento3 pagineFinal Paper Biologyapi-242268441Nessuna valutazione finora
- ACG Guideline Cdifficile April 2013Documento21 pagineACG Guideline Cdifficile April 2013Fitria FieraNessuna valutazione finora
- Tuberculosis - Disease Management - CompDocumento17 pagineTuberculosis - Disease Management - CompAhsan kamalNessuna valutazione finora
- Cdi and FMT Risks and BenefitsDocumento5 pagineCdi and FMT Risks and Benefitsapi-426734065Nessuna valutazione finora
- Epidemiologyand Pathogenesisofulcerative Colitis: Lillian Du,, Christina HaDocumento12 pagineEpidemiologyand Pathogenesisofulcerative Colitis: Lillian Du,, Christina HaVinicius BalanNessuna valutazione finora
- Invasivecandidiasis: Todd P. Mccarty,, Peter G. PappasDocumento22 pagineInvasivecandidiasis: Todd P. Mccarty,, Peter G. PappasthrewawayNessuna valutazione finora
- What Is The Role of Antimicrobial Resistance in The New Epidemic ofDocumento4 pagineWhat Is The Role of Antimicrobial Resistance in The New Epidemic ofcarrrrr567Nessuna valutazione finora
- Clostridium Difficile Infection - MRCEM SuccessDocumento5 pagineClostridium Difficile Infection - MRCEM SuccessGazi Sareem Bakhtyar AlamNessuna valutazione finora
- UEG Mistakes in Acute Severe Ulcerative Colitis and How To Avoid Them 2023Documento3 pagineUEG Mistakes in Acute Severe Ulcerative Colitis and How To Avoid Them 2023Mohamad MostafaNessuna valutazione finora
- Acute Sever UCDocumento11 pagineAcute Sever UClunaTSNessuna valutazione finora
- Elife 79397 v2Documento21 pagineElife 79397 v2lata.pauccaraNessuna valutazione finora
- Nanoparticle-Mediated-Therapeutic-Approach-for-Ulcerative-Colitis-TreatmentDocumento22 pagineNanoparticle-Mediated-Therapeutic-Approach-for-Ulcerative-Colitis-TreatmentAchudan JiiNessuna valutazione finora
- The Changing Epidemiology of Invasive Fungal InfectionsDocumento49 pagineThe Changing Epidemiology of Invasive Fungal InfectionsHèla HassenNessuna valutazione finora
- C. Diff Toxin AssayDocumento15 pagineC. Diff Toxin AssayMaira KhanNessuna valutazione finora
- Fast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careDa EverandFast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careNessuna valutazione finora
- Nutrition Support: Sean P Harbison MDDocumento42 pagineNutrition Support: Sean P Harbison MDsgod34Nessuna valutazione finora
- Surgery Preround Template SkeletonDocumento2 pagineSurgery Preround Template Skeletonsgod34Nessuna valutazione finora
- NOAC ChartDocumento2 pagineNOAC Chartsgod34Nessuna valutazione finora
- Modes of Mechanical VentilationDocumento4 pagineModes of Mechanical Ventilationsgod34100% (1)
- Master Schedule 10-22Documento65 pagineMaster Schedule 10-22sgod34Nessuna valutazione finora
- Veins More DistensibleDocumento27 pagineVeins More Distensiblesgod34Nessuna valutazione finora
- Colon CADocumento16 pagineColon CAsgod34Nessuna valutazione finora
- 7 MedEd Vascular Jonny Hodgkinson 12.11.12 1Documento35 pagine7 MedEd Vascular Jonny Hodgkinson 12.11.12 1sgod34Nessuna valutazione finora
- Venous DiseaseDocumento50 pagineVenous Diseasesgod34Nessuna valutazione finora
- Endoscopy TechniqueDocumento8 pagineEndoscopy Techniquesgod34Nessuna valutazione finora
- Anast Bleed MMDocumento17 pagineAnast Bleed MMsgod34Nessuna valutazione finora
- Resident Hernia LectureDocumento106 pagineResident Hernia Lecturesgod34Nessuna valutazione finora
- HD Monitoring ColoradoDocumento28 pagineHD Monitoring Coloradosgod34Nessuna valutazione finora
- Riker ABSITE ReviewDocumento36 pagineRiker ABSITE Reviewsgod34Nessuna valutazione finora
- A Case of Fungal KeratitisDocumento6 pagineA Case of Fungal KeratitisPhilip McNelsonNessuna valutazione finora
- Letter To ParentsDocumento1 paginaLetter To ParentsWSETNessuna valutazione finora
- Dengue Prevention & Control ProgramDocumento13 pagineDengue Prevention & Control ProgramJuliet Echo NovemberNessuna valutazione finora
- Research PaperDocumento15 pagineResearch PaperKeithryn Lee OrtizNessuna valutazione finora
- Endothelial KeratoplastyDocumento17 pagineEndothelial KeratoplastyZulva Fuadah ANessuna valutazione finora
- Peri-Implant Diseases Pathogenesis and TreatmentDocumento8 paginePeri-Implant Diseases Pathogenesis and TreatmentPaul IvanNessuna valutazione finora
- Colorphobia in New YorkDocumento3 pagineColorphobia in New Yorkapi-412124766Nessuna valutazione finora
- Cholesteatoma - Diagnosing The Unsafe EarDocumento6 pagineCholesteatoma - Diagnosing The Unsafe EarGuillermo StipechNessuna valutazione finora
- Polio Case StudyDocumento19 paginePolio Case StudyKatNessuna valutazione finora
- Worm InfestationDocumento1 paginaWorm InfestationMRS CHAKRAPANINessuna valutazione finora
- BibliographyDocumento7 pagineBibliographyptsievccdNessuna valutazione finora
- New PMDC Neb Format 2011Documento28 pagineNew PMDC Neb Format 2011AliHazratNessuna valutazione finora
- A Fascinating Story of Exploding Toads and Clever CrowsDocumento2 pagineA Fascinating Story of Exploding Toads and Clever CrowsDirham RevolusionerNessuna valutazione finora
- Toronto Notes Nephrology 2015 22Documento1 paginaToronto Notes Nephrology 2015 22JUSASB0% (1)
- 04 11 2016.tanzania National Guideline For Management Hiv and Aids May 2015. TaggedDocumento290 pagine04 11 2016.tanzania National Guideline For Management Hiv and Aids May 2015. TaggedArdilah Dwiagus SafitriNessuna valutazione finora
- David OnyangoDocumento16 pagineDavid OnyangoprabhasNessuna valutazione finora
- RickettsiaDocumento3 pagineRickettsiaFeroz MamunNessuna valutazione finora
- Effective Alternative Mosquito Repellent From Lemongrass As Candle Based FormulationDocumento14 pagineEffective Alternative Mosquito Repellent From Lemongrass As Candle Based FormulationFaith LagguiNessuna valutazione finora
- Mikroba Saluran PencernaanDocumento70 pagineMikroba Saluran PencernaanAde Yurga TonaraNessuna valutazione finora
- Letter MamburaoDocumento1 paginaLetter MamburaoZyreen Kate BC67% (3)
- Preventing and Managing COVID-19 Across Long-Term Care ServicesDocumento8 paginePreventing and Managing COVID-19 Across Long-Term Care ServicesMark Anthony MadridanoNessuna valutazione finora
- Review of Related LiteratureDocumento8 pagineReview of Related LiteratureDaniel Fancis Amabran BarrientosNessuna valutazione finora
- 0e893481 LotemaxgelDocumento2 pagine0e893481 LotemaxgelGhufron A. AzisNessuna valutazione finora
- Mohd Afiq Izzuddin Bin Rossli (1001336000) (Soft Tissue Swelling) 543. 15-16Documento23 pagineMohd Afiq Izzuddin Bin Rossli (1001336000) (Soft Tissue Swelling) 543. 15-16Star CruiseNessuna valutazione finora