Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Long case format and data for MBBS final exam
Caricato da
whee182Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Long case format and data for MBBS final exam
Caricato da
whee182Copyright:
Formati disponibili
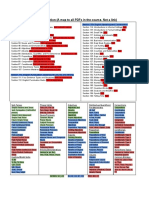
Long case MBBS(Malaya) 06/11 Final Exam Data Store Please present your long case following this
s format. 1. lecturers who took u 2. specialty 3. chief complaint 4. brief history 5. PE finding 6. diagnosis 7. questions asked by lecturer about a week ago Report Post Marked as Irrelevant about a week ago Show Post Post Marked as Irrelevant about a week ago Show Post Post Marked as Irrelevant about a week ago Show Post Post Marked as Irrelevant about a week ago Show Post
Nurulsyuhadah Bt Mohd Ramli 1. lecturers who took u : prof saw aik (menguap), prof ikram (menguap jgk) , prof mtkoh (senyap je) 2. specialty : sooooo not into ORTHO 3. chief complaint : knee pain 1 year 4. brief history : errrr...... typical knee pain ;p 5. PE finding : varus, crepts, limited movement. 6. diagnosis : RIGHT KNEE OA 7. questions asked by lecturer : how to manage? :) p/s: 1 patient for 2 students!!! me sharing with Aiman~ (obviously he did better than me.. arghhh!!!!!!) about a week ago Report
Lim Xin Jie 1. lecturers who took u-prof philip poi,prof dharmendra,prof cheah-external paed 2. specialty-PCM/Med 3. chief complaint-right big toe swelling-1st presentation(10 years ago) 4. brief history -during the 10 years, multiple joint involve as well.but everytime 1 joint...ass stiff and affect function..ambulating wheel chair after 3 attack..last attack 2 years ago,right knee pain ass swelling and fever..background history of HPT. 5. PE finding-cushing facies + u all noe,deformity finger(boutonnier),fix left ankle joint. 6. diagnosis-gouty arthritis,uncontrol HPT,steroid coz cushing n mayb metabolic 7. questions asked by lecturer-what investigation u want to do?he want ESR and CRP and uric acid... -is it uric acid normal meant no gout?no -whic joint aspiration u want to take?mid size joint -what u see in aspiration?monosodium urate crystal, negative birefringent.. -how u like to manage? NSAIDS-indomethacin -S/E NSAIDS?UGIB,gastritis,... -others TX-allopurinol..when u wan to start?after d acute attack?why??i answer will aggravated d acute state..then prof philip said nwm..is HIGH5 -others Mx-rehydration,diet and control HPT.. -what do u think about the Med Compliance... -how u assess d compliance med of this patient? there are still questions will b asking during history and PE...n i m sharing patient with perak students... about a week ago Report
MBBS(Malaya) 06/11 Final Exam Data Store From Michael,same patient with Sow Cheng A bit screwed up... =( Haiz... 1. lecturers who took u: Prof CT Tan,Prof Siti,Prof Woo,Dr Pan(External) 2. specialty: Medicine Nephrology 3. chief complaint: Nil
4. brief history: Background history of SLE diagnosed 3 years ago with lupus nephritis. Initially presented with rash,artritis,oral ulcer and progressive worsening of both lower limb and facial puffiness worsening on morning. HIstory of preterm baby and 2 miscarriage. 5. PE finding: Pedal oedema up to knee level.Multiple bruises seen on knee and forearm. 6. diagnosis: Lupus Nepritis 7. questions asked by lecturer -Proteinuria: why 24 hours urinary protein instead of urine dipstick -Does the pregnancy you want to concern related to her problem? -Her son preterm,how preterm is preterm?On how many weeks?Related to her problem? How about the miscarriage? -Does she on remission or the disease is active? -What is her current problem?(I say no active chief complaint? Is she come just for your exam sake? (She really no C/C) -Let see the patients.Show me the finding u think relevant?(Bruises,pedal oedema) -Moonface(They seem not agree)?Do you exposed probably?How about the hair loss? -Any kidney ballotable? -Go back to room.She got multiple bruises,what do you think the causes?Low platelet cause bruises like this?(He want petechaie =( ) -How you know her disease is active? HOW??? Clinically??? -Investigation you want to do?Renal profile,elaborate more on renal profile. -C3,C4.what is C3,C4? -what you will see on microscopic examination of urine? -Proteinuria detected?Mild or what?Of course more than 3+ lo... -What is nephrotic symdrome? -No management discussed...... =( Really pray hard this time...All the best to coming group... about a week ago Report
MBBS(Malaya) 06/11 Final Exam Data Store Siti Zarina Jahan. Please present your long case following this format. 1. lecturers who took u Prof KJ Goh, Prof Azad, Prof Azmi 2. specialty Medicine.
3. chief complaint vomiting 1 week 4. brief history 26 year old Malay gentleman, well untl 5 years ago when he developed vomiting 1 week. a/w low grade fever, diarrhea, lethargy, palpitation, irritability, tremor. then suddenly 1 day history of SOB, admitted, 5 days, CXR, EC and thyroid function test was done and was told to have hyperthyroidism. on medication carbimazole for 1 and half year, propanolol for 2 months and ranitidine for few weeks. currently euthyroid. has been married for 5 years but still do not have children. adopted a child, 2 and a half year. infertility still on investigation. 5. PE finding normal. no hyper/hypo/goitre/grave's. just have pigmented lesions on the foot. 6. diagnosis thyrotoxicosis secondary to grave's? or MNG. 7. questions asked by lecturer - PE: asked to demonstrate eye signs. what are the differences btween grave's and hyperthyroid signs. how do we know the disease activity. - in the room: why is the patient has vomiting? and why is it resolved after he is euthyroid? what are yr investigations. why this pt has normal T4 but low TSH. what is your management? how long is carbimazole given? propanolol? side effects of carbimazole? if pt has neutropenia what will u do? can it be given to pregnant lady? of failed 3x carbimazole, what wil u give? (radioisotope iodine) what is the mechanism? tell me about everything you know. if failed medical treatment, what will u do?--surgery. what are the complications of thyroid surgery?-thyroid storm, bleeding, recurrent laryngeal nerve injury, and parathyroid gland injured. what are the signs that you know of parathyroid deficiency?-carpopedal spasm dll. then dah.. belum loceng lagi dah kena suruh keluar.huhu. good luck kawan2 and my beloved juniors :) about a week ago Report
Farah Hanani 1.lecturers : prof khoo, prof adeeba, external examiner 2. specialty : surgery 3. brief history : 65/chinese/gentlemen presented with right HPC pain+early satiety+bloating+consitutional symptoms. problems started last year, only went to UMMC after his friends advice him. chronic smoker, likes to skip lunch due to satiety. k/c/o of DM with retinopathy, hypertension, hypercholesterolaemia. went
to UMMC early this year. OGDS, CT scan and blood investigations were done. CT scan shows lung and liver mets. 4. PE finding : normal except he looks cachexic and pallor. he told that his doctor said he has palpable left supraclvicular nodes. but i double check, no lymph node. little bit of hernia~aishhh 5. diagnosis : stage 4 stomach ca with lung and liver involvment 6. questions - symptoms of anaemia - physiology of lymphatic drainage - demonstrate abdominal PE and why you do so - differential diagnosis - interpret CT scan - other investigation - how to manage palliative....~good luck guys about a week ago Report
Mohammad Faaizzin Jamaluddin 1. lecturers; Prof MTK, Prof Saw, Prof Ikram 2. specialty; Paediatric (haematology) 3. chief complaint Abdominal discomfort 4. brief history 16yo boy presented with intermittent abdo discmfrt and mild scleral jaundice. Was diagnosed with thalasaemia at 13yo and need mothly blood transfusion. Had prvious history of intermittent fever, pale and jaundice and diagnosed with G6PD deficiency. Other systems were normal. 5. PE finding Hepatosplenomegaly, scleral jaundice. delayed puberty ( pubic hair stage 1, penis stage2). Height and weight equivalent to 50th centile of 11yo boy. 6. diagnosis Thalsaemia minor or intermedia, with delayed puberty. 7. questions asked by lecturer Pathophysiology of G6PD Pathophysiology of thalasaemia Diagnose type of thalasaemia from histry alone Examination of blood transfusion complication Assess severity of anaemia
Pubertal stage Investigation about a week ago Report
Kin Wong Chan Prof KL Goh Prof Azad Prof Azmi Speciality: Surgery C/O: Recurrent Epigastric Pain x 1 year Brief Hx: 43 y/o Malay Lady, well till 1 year ago develop epigastric pain, sharp, gradual onset over few hours, tolerable pain, assoc w eating, relieved by bending forward & radiate to the back. Frequency of the acute pain is about twice a month until 3 months ago when the pain starts to become more frequent and she had it almost daily now. Most of the time the pain will resolve spontaneously our a few hours. However there's 2 episodes where she experienced a severe pain with score of 10/10 3 months ago and 3 weeks ago. During these severe episodes, she had jaundice, fever, chills, rigors which was preceeded by the pain. She came to UMMC for both the episodes and pain resolved after some treatment antibiotics, painkiller & fluids. The jaundice was also resolved with treatment. She was told to have a liver condition 3 months ago & after radiological ix she was told of some pancreatic condition which she was unsure of. diagnosis: gallstone pancreatitis questions: PE: abdo examination, signs that i would look for(pt was completely normal with no signs at the moment) room: ask about differentials & why (coz didnt mention the wanted dx stated above although mentioned common bile duct stone w reflux pancreatitis) Ix: fbc, lft, serum amylase, US & reasons why give blood ix results of one of the acute attacks and asked to interpret (Bilirubin, ALP, GGT, amylase high) mx: what to be done if pt acutely admitted with the above ix results (resus,med, ercp) others: why pt w stones hv intermittent pain ask why bilirubin can b high but no conjunctival jaundice what does tea-coloured urine imply discussing over the final diagnosis out of my differentials about a week ago Report
Salahuddin Abd Jaafar 1. lecturers who took u: Prof Khoo Ee Ming (PCM), Prof Adeeba Kamaruzzaman (Medicine), Dr Zygmunt (External, dia senyap sepanjang masa) 2. specialty: Medicine and PCM 3. chief complaint: come for exam. currently under follow up for: endometrial Ca (post-TAHBSO) asthma deep vein thrombosis obesity and Diabetes Mellitus (ini main problem dia) 4. brief history suhaili, 35, malay, lady a) asthma, since childhood, well controlled, currently on bicotide and ventolin b) dvt, currently on warfarin 8mg OD, INR:2-3, well controlled c) endoM Ca, done TAHBSO, 15 round of chemo, and brachytherapy. currently well, no sign of mets/recurrence d) Diabetes: currently on metformin 850mg, diamicron 1 tablet OD, insulatard 10U before bed. last follow up HBA1c is 12.1. Poorly control. claim take medication and controll diet. however do not exercise. 5. PE finding (positive finding only) random blood sugar: 13.1mmol/l obese: BMI 37.37 left leg swelling with varicose vein 6. diagnosis uncontrolled DM with obesity. and currently on medication for DVT 7. questions asked by lecturer during PE: demonstrate how u confirm swelling, what is the causes of unilateral leg swelling, when patient started to develop diabetic neuropathy as this patient only diasnosed DM incidentally for 3 years, what can be the causes of the swelling in this patient (lymphoedema???) back in room: what is the current status of her DVT, what is the patient current concern (uncontrolled DM), if HBA1c is 11.1 what does it means, what other investigation would you do for this patient, in UFEME if protein 1+ what does it means, (contamination??UTI??), how to rule out this, other investigation, give all other investigation and managament for DM in this patient. (ting tong... times up). that's all i managed to get asked. about a week ago Report
Fadya Nabiha lecturer: prof kf Chin, Prof Rokiah panjang, prof mk.Thong speciality:paed chief complain: coming 4 exam..(ha3) brief history: 2year 10 month old girl. early childhood got history of eczema on trunk, allergy to seafood-uricaria...nocturnal symptoms, daytimel cant assess as pt woke at 10 a.m. exacerbation at 1 y/o-not interfere with sleep , activity n eat pn...x severe...4 months, refer to a&e PPUM -inhaler fluticasone n sabutamol...basically assess pt control..1 year later, change to seretide n salbutamol...partially controlled asthma p.E-harrison sulcus, hyeperinflated chest..wt at 50th centile, length 90th centile diagnosis-partially control asthma question:1. what is aerochamber, differentiate with nebuliser...name of d noisy machine..function 2.signs of severe asthma 3.allergy rash4.how to diagnosed asthma-prof thong want the bronchodilator test 5.why hyper resonance in astma, the name?-air trapping about a week ago Report
Chee Woei Yap 1. Prof Lee WS, Prof Jamiiah and external from NUS 2. Paeds. 3.C/O:7 year old malay boy presented 3 days ago with fever and bilateral LL swelling started on DOA. 4.picture of nephrotic syndrome.1st episode. father got nephrotic syn at 22 years old. biopsy done but not sure bout the Dx. on Pred for 3 monthy then no more recurrent. Devp normal..no other problem. started to devp scrotal swelling in the ward. 5. PE: demonstrate pedal edema, ascites, and pleural effusion. patient has generalised edema and scrotal swelling...wat is this call?.... Anasarca 6.diagnosis: nophrotic syndrome. 7.wat is the different between edema in AGN and nephrotic Syn? y do u ask about URTI and skin rashes in the past 1/12? TRO AGN father has nephrotic syndrome, any relation?
patient on pred, wat is the changes in the FBC picture?...... wat are the S/E of pred? patient went back with pred, father complaint of patient bcome aggitated and angry....wat happen? temper tantrum y doing CR: Alb ratio?wat is the principle behind?y have to take early morning urine? wat is ur Ix and Mx? wat is the pathophysio of edema in nephrotic Syn?( by external)
about a week ago Report
Michelle Low Lecturers: Prof. Philip Poi (keep texting and jotting) Dr. Cheah xx (external Paeds Consultant) Prof Dharmendra (funny position) Specialty : Paediatric Chief complaint: breakthrough seizure Brief History : 12 year-old Indian girl who has background history of Epilepsy since 9 months old, on Epilin, carbamazepine, and ADHD on Ritalin, presented with breaktrough seizure. Compliance problem, average student, attain menarche at 11 year-old, strong family history of Epilepsy, able to join school activities...BMI 22.9 I forgot to take developmental history and Diet hx! p/e: Demonstrate hyperreflexia on UL and presence of nystagmus. Diagnosis : Breakthrough seizure Questions 1. What physical signs would you like to show us to suggest to you that recurrent seizure is familial? -neurocutaneous sign; what cutaneous sign? - cafe au lait, ash leaf sign, and sebaceous adenoma? (tuberous sclerosis); what is the significance of cafe au lait- Neurofibromatosis ; what is the nerve root of biceps? 2. How to monitor compliance besides asking history? - monitor drug serum level, which one?.... 3. Are you satisfy with the current drug dosage? why? - puberty, side effect, 4. Pertaining to BMI... relation to drug...side efffect, must ask dietary history to rule out lifestyle causes...
5. causes of pathological jaundice - ABO incompatibility, rhesus, g6pd 6. Since she is having multiple seizures despite on medication, based on p/e, are you happy with the current drug pescription? how would you do? - investigate to rule out CNS pathology about a week ago Report
Tan Zi Kheng Tan Zi Kheng 1.prof jamiyah, prof lee way siah, dr.Lang (external) 2.O&G 3.coming in for IOL at 38 weeks of POG. 4. 42yo, G6P4+1, background history of DM for 2 years, on diet control only. currently, at 37 weeks of POG. unwanted and unplanned pregnancy. antenatal uneventful. started on insulin at 12 weeks POG. (As usual, DM history starting 2 years ago...until now. Luckily she is a stuff nurse, so she can tell all the results for blood glucose.) 5. PE finding: singleton pregnancy, longitudinal lie with cephalic presentation. not engaged, adequate liquor volume. estimated fetal weight 2.6kg 6. normal pregnanvy with 2 years history of DM 7. Prof J interuppted me along the way I presented. Everything was in a hurry. Never stop asking qustions...even on the way to the examine the patient. The 2 other examiners just follow at the back. What do you mean by POG? How to calculate EDD? What is the EDD for this pt? since my patient's EDD is confirmed by U/S. Why she didn't have OGTT done this time? Why you say the control is suboptimal? What is her contraception method? How you ask for complication of DM? I already answered all, but she is expecting smthg else. What is the definition of stillbirth? Why peripheral neuropathy in pregnant lady? pt complaint of numbness over the fingers, but bedside when I examine in front of examiners, she kept on saying 'Tajam tajam.."zzzz How to do GCT? How to do OGTT? how to advice pt before OGTT? normal value? How to investigate the mother? ( I said all tests,even fructosamine.haha. still duno what she wanted) How to do monitoring? bla bla bla... what is the weight gain allowed in this pt?
what is the normal weight gain? What do you expect to find in U/S? I said cardiac anomalies. and also nuchal translucency in Down's. (prof lee noded at the side) she asked cardiac defects in DM or GDM? I answer GDM. but WHY? When do you want to deliver the pregnancy? PE: show me how to do peripheral neuropathy? how you clinically estimate the week of gestation? Is the head engaged? What are the signs of complication you are looking for in this pt? How to calculate BMI? ( prof I didn't calculate hers but i know is above 25.) How you know? huh, got faster way? (Yup) Show me.. what is the urine glucose test results?
about a week ago Report
Huey Jiun Tan 1. Prof Ikram, Prof MTK and Prof Saw Aik 2. Medicine 3. 78 years old chinese gentleman with underlying HPT and diagnosed to have chronic kidney disease for 2 years. oher problem, gout and hyperlipideamia. 4. PE: just present the findings... no bedside examinations ( loook for complications of HTN) 5. How to grade the severity of intermittent claudication? Answer: distance claudication How is the patient's BP control? what do u think? wat is ur IX and MX ? wat usually caused CKD patient died? heart attack about a week ago Report
Winy Jojo WinyJ 1. examiners: Prof Aili (child psychiatric), Prof CK Liam, external (Mary) 2. specialty: psychiatric
3. c/o: 31/C/M, single n unemployed. abnormal change of behaviour x17years 4. brief history: - started to notice weird repetitive habit since secondary school (form 2). going in n out of house to check if house door was closed, folding clothes neatly if got messed up, wrote certain markings in school work. - few months later developed new set of symptoms: whenever touched anyone, washed hand quickly, took bathed quickly once got home, washed wallet n blablabla.. (real long psych hx!!) - dev secondary MDD a/w 3 episodes of suicidal attempt. -no psychotic or manic sx. no subs abuse. no underlying medical condition - fhx of depression (father). mother died of breast ca. - had appendicectomy during childhood. few years ago had IO due to intussusception, emergency laparotomy. then got dx with IBS - currently on lexapro 30mg OD 5. PE -prof only asked me to elicit his thought pertaining to his current condition 6. diagnosis - OCD with secondary MDD (his low mood is very well controlled now. thats why i didnt mention MDD secondary to OCD. at least d former dx emphasize more on OCD. tho it may mean d same. hehehe.....) 7. q asked: only prof aili actively grilling me. d rest asked 1 or 2 pertaining to hx only. - stressor, social n occupational functioning, n some other q related to hx 2. - dx, mx - lotsa time spent in presenting d hx. i was fumbling away. used >5 pages of paper to clerk!! so its all written here n der. ggggrrrr..... (apneic episode) - no dsm criteria was asked or any definitions. - couldnt present full hx just like in d clerking sheet. prof just wanted hopi n related hx only. (limited time kot) overall comment: never clerked ocd before. huhuhuhu!! so blessed to have prof aili. she was really patient n soft spoken. hehehe! gudluck dear friends!!! about a week ago Report
Raymond Yii Shi Liang 1. Lecturers who took u: Prof. C.K Liam (silent), Prof Mary (Caucasianexternal,the main examiner) & Prof Aili (silent) 2. Specialty: Gynaecology 3. Chief complaint: Sundravalli, a 49-year-old Indian lady, para 5, presented with menorrhagia for 2 months.
4. Brief history - Menorrhagia for 2 months since Oct 2010. - flooding, blood clots of multiple size with the largest one 20 cent-sized, daily 5-6 pampers fully soaked with blood. - It was associated with severe persistent abdominal pain localized at lower abdomen extending to both right and left iliac fossa. There was also low back pain. Other associated symptoms such as abdominal distension and pressure sx (urinary freq and tenesmus) were absent. No history suggestive of PCOS. - sought treatment in HTAR and was told that US showed fibroid. 5. PE finding - Conjunctival pallor, left iliac fossa tenderness, mass in left iliac fossa (I couldn't feel it, but the examiner could feel it - what a disastrous thing happening to me!) - I also told that there were scleral jaundice and hepatomegaly. But Prof CK Liam confirmed that there was none. So, be careful of the lighting condition when u're checking for scleral jaundice. - Pelvic exam was not performed becoz the patient refused. The examiner asked me what would I look for in pelvic exam: Speculum exam: vaginal bleeding, prolapsed endocervical polyps and cervical carcinoma Bimanual vaginal exam: Size, site, consistency, tenderness and mobility of uterine fibroid. 6. Diagnosis - The examiner never asked me about this. Because the history itself had already revealed the diagnosis. - My differential diagnoses: cervical CA, PCOS, DUB, endometrial CA, adenomyosis and endocervical polyps. 7. Questions asked by lecturer - Can u plz tell how would u investigate for this lady and reason for each test? Basic investigation: FBC - anemia, microcytic hypochromic due to bleeding RP & LFT - baseline for pre-op Coagulation profile - ensure that the bleeding is not due to coagulopathy Pap smear test - for cervical CA ( The examiner then asked: ' Why would u want to repeat this again since this had been done on Feb this year?' 'How long is the interval for the next smear?' If first two consecutive results are negative, then every three years. Imaging: Transabdominal US scan - fibroid (size and site) - endometrial thickness >4mm for endometrial hyperplasia and CA Examiner asked: 'What is the endometrial thickness of a pre-menopausal woman? I dunno. 'Is endometrial thickness of >4mm common in premenopausal woman? I answer no, but the answer is yes. ' Is endometrial hyperplasia common in pre-menopausal woman?' I answered no. Then she asked further: 'In wat situation the endometrial hyperplasia is commonly seen in pre-menopausal woman?' PCOS. Biopsy: Endometrial sampling by hysteroscopy/pipelle - to assess the histology of endometrium for hyperplasia or CA.
- 'In one word, describe how would u manage this patient?' Mx depends on the age, parity and desire for future childbearing. Since this lady had completed her family, hysterectomy is the option. - 'If the woman wants her uterus, what alternative would u opt for?' Myomectomy, but it's a/w risk of bleeding. - 'I don't want this answer, any other?' HIFU - High Intensity Focus Sonography. All the best to those who are going to have their long case on Tues and Wed. May all of us pass the exam! about a week ago Report
Li Keat Oon lecturer: Prof J (O&G), Prof Lee Way Seah, External Specialty: Obstetric I got a very easy case (Pregestational DM with vaginal discharge), but I struggle remembering things to be covered in a Obstetric history, so experienced multiple thought blocks in the exam. (run back in last minute to ask for blood group, infective scan and booking) So, please look tru the clerking details before going in. Prof J conducted the exam. Her question was easy but want really specific answers... (Like many other examiners), So, please know what's important before u "vomit" ur theories. She was surpricingly nice & I heard her questions was standard in the rounds (So, juniors, pls don't skip her round as I did =p ) Chief complaint: non, only for follow up in clinic, except for a vaginal discharge investigated very long ago. History 40yo? Malay lady. G6P4+1. in 37w POG LNMP: 11. June 2010 EDD: 18 March 2011 REDD: 15 April 2011 Past Obs: 3 uneventful but post date, then followed by 1 w history of GBS infection but no PPROM & baby healthy full term. all baby ranges 2.9-3kg. No fetal abnormalities. DM diagnosed 3 years ago after miscarriage in 2009. Previously under diet control but started insulin on 12w POG Discharge thin whitish yellow, non-foul-smelling, non-pruritic, previously investigated but nothing found. PE:
- SFH: 36cm. - everything else normal except for a Grade 3 ESM at LSE, non-radiating, changes with position. Questions: 1. Difference between POA & POG (I said scan but she want sthg like conception and ovulation) 2. Fetal abnormalities in 1st trimester (I answered sacral agenesis, but she wanted more) 3. Ix (I think she want us to say "serial" blood glucose and ultrasound) 4. Common infection in GDM (candidiasis like in usual DM) 5. What is HbA1c (I think she want to stress it's not important in GDM) 6. Induction, complication and medication used. 7. Why deliver at 38w (I answered lung maturation, shoulder dystocia..., but she wanted sthg else...) 8. things u tell the nurse when the baby delivered (monitor glucose, jittering, respi distress...) 9. When u wana measure the glucose, give a specific time. (I think I may had skewed up by bombarting a number, should have said I don't know) 10. she keep on stressing on Cx of polyhydramnios in GDM in few discussions, donl't really understand some of her questions, so couldn't remember, so junior pls go explore during her rounds. Prof Lee 1. How u detect erb's palsy (asymmetric moro) 2. What u wana do if u suspect erb's (refer ortho? Prof Lee: isit?) 3. What position u will like to placed the baby if he has erb's palsy) Good luck every1... about a week ago Report
Roszita Bt Mokhtar 1.examiners:prof philip poi(geriatric),prof dhamendra(neurosurg),Dr cheah(external-paed) 2.speciality:surgery 3.c/o: 65y/o/C/M -per rectal bleeding-2 weeks.DM + HTN for 4 years on meds 4. Brief history. Previously well,1st episode,hx of passing out fresh blood associated with mucus and loose stool.no abdominal pain or swelling, no symptoms of infection,no loa low.ex-smoker stopped 10 years back.previously smoke 40 sticks/day for 25 years.occ drinker, fx of esophageal carcinoma.
5.PE midline scar,stoma on left iliac fossa,chemo port insertion scar, incisional hernia over the distal part of the scar. 6. Diagnosis colorectal carcinoma 7.Question asked by lecturer 1.what do u mean by tenesmus? 2.how u diff melena and fresh blood?why they are diff? 3.is the patient depress? 4.pe:ilicit hernia,do hernia examination, 5. ix: what is diff between barium enema and colonoscopy? 6.mx:follow up patient what do u want to look for?-NUTRITION! Gud luck guys:) about a week ago Report
Li Keat Oon oh ya... in PE, she asked me: clinically, do u think the abdomen correspond to the date (I said I wana do a SFH, she said no, just look!) looking at her espression, my mind was like: Shit, did I measured wrongly?... I freaked out and remained silent (as this is a life or death answer...) Then she said: the fundus reached the xiphoid process, so? Then only I releved: Haha... yayaya.... Other Questions in PE: 1. What other examination u will do in GDM 2. What's the estimated weight in this baby? (luckily my patient told me the estimated number during the last scan. 3. How to perform OGTT? (75g..blablabla...) & values in GDM about a week ago Report
MBBS(Malaya) 06/11 Final Exam Data Store From : Suriaraj Lecturers: Prof Nor Azmi, Prof KL Goh and Prof Azad..... =) Specialty: Obstetrics PC: Anaemia in pregnancy
HOPI: 36 year lady G9P7+1(miscarriage) and one neonatal death currently at 34 weeks period of amenorrhea. pregnancy unplanned but wanted. Did conformation of pregnancy at 15 weeks POA at private clinic by UPT and ultrasound scan.Given obimin tablets bcoz of anaemia history in previous pregnancies.. (All 8 pregnancy got aneamia with 4th pregnancy requring pre delivery blood transfusions) booking at ummc at 27 weeks POA.. found Hb to be 9.1.. prescribed ferrous fumarate (1 tab OD), obimin (1 tab OD) and calcium carbonate.. at 31 weeks POA second visit to UMMC found Hb to be 8.4 and thus ferrous fumarate dose increased to 2 tabs daily. past obs hx she had history af large babies ranging from 3.8kg to 4.48kg and hx of fetal shoulder dystocia during 4th pregnancy. No GDm hx in any pregnancy.. at 30 weeks POA onwards she started developing symptoms of anemia such as SOB, reduced effort tolerance, lethargy and occasional palpitation.. PE: all normal, baby cephalic presentation in longitudinal lie.. Got palmar crease pallor and conjunctival pallor.. Questions: no question on history.. after history i was brought to the patient and Prof Azmi told me "examine this patient".. so, i started from the peripheral examinaton eliciting the palmar crease pallor and conjunctival pallor. (make sure compare your palm with patient's to show palmar pallor). Then i proceded with abdominal palpation, presented the fetal presentation, lie and the head palpable per abdomen. Prf ask me wht is the estimated weight of fetus (i said 2.5-3, he said ok), and he ask wheter clinically liquor volume adequate or not (i said adequate).. Back in the room, profAzmi ask me when will u transfuse patient.. I said if Hb less than 8. Prof KL goh ask me wht other criteria for transfusion (ans: clinical feature of severe anaemia..) Prof Azmi asked me if i see this patient first time at antenatal clinic, how would i manage this patient?? I said start from blood ix to look for cause of anaemia and the i elaborated from there.. I said i would prescribe oral iron supplements.. he ask wht is the possible cause of the anaemia in this pt?? I said patient is a grand multipara with no spacing between pregnancy, so the iron stores are depleted.. Key word is iron store depletion.. (prof KL goh wanted to hear that) He then asked me if patient comes and tell u that her friend claims that parenteral iron is better, hw would u advice patient?? - i said efficacy of both is same but side effect profile differ and compliance is better with parenteral.. he ask me if this patient is going into labour, what are the problems u anticipate?? I said main concern is the anaemia as severe anaemia during delivery can cause a cardiovascular collapse and i said that there is possibility of shoulder dystocia coz got hx of large babies..
He ask me wht else possible complication?? -i said PPH coz she is a grand multipara thus got risk of uterine atony.. he then ask me management of PPH.. He wanted to hear uterine massage initially after syntocinon infusion and hysterectomy when all else fail.. He ask me, if u see this patient after 6 weeks of delivery and delivery uneventful, wht would you advice to patient?? - i said main concern is family planning and contrception. so he ask me about the different type of contraceptive available?? -Prof Azad's only question was wht other contraceptive method( after i have said everything on the women point of view)- I said vasectomy and he said yes.. prof azmi ask about Pap smear.. "tell me about Pap smear??".. Then he ask if patient got CIN II how u want to manage.. I said LLETZ Then he ask if patient got CIN II and severe dysmenorrhea and menorrhagia due to adenomyosis wht would u do.. The ans is hysterectomy (Prf KL Goh whispered the ans to me.. =p ) P/S: Me and Fikri shared the same pt.. I m the second student.. so make sure to ask ur pt wht the lecturer ask the previous student during PE.. The patient knows and this may help.. Good luck for the rest!!! =) about a week ago Report
Aidy Azuan Afifi (patient same as fadya) lecturer: prof kf Chin, Prof Rokiah panjang, prof mk.Thong speciality:paed chief complain: coming 4 exam..(ha3) brief history: 2year 10 month old girl. early childhood got history of eczema on trunk, allergy to seafood-uricaria...nocturnal symptoms, daytimel cant assess as pt woke at 10 a.m. exacerbation at 1 y/o-not interfere with sleep , activity n eat pn...x severe...4 months, refer to a&e PPUM -inhaler fluticasone n sabutamol...basically assess pt control..1 year later, change to seretide n salbutamol...partially controlled asthma p.E-harrison sulcus, hyeperinflated chest..wt at 50th centile, length 90th centile diagnosis- control asthma
question: 1. what is aerochamber, differentiate with nebuliser. 2. ask about immunization schedule 3.signs of severe asthma 4.how to diagnosed asthma-prof thong want the bronchodilator test 5.advice to mother: 1st i tell about how to control asthma, the prof rokiah ask any advice regarding developing eczema......(she want answer about avoid detergent) 6. ask what u can see in chronic asthma.... i jwb growth problem.... then he ask about the the chest, i answer increase AP diameter n hyperinflanted lung....., he want chest deformity.... about a week ago Report
Mahirah Rar 1. lecturers who took me: prof Pon Khoon-ORTHO (external kot, tak penah dengar), prof CT Tan-NEUROMEDICINE, prof Siti Zawiyah-OBS N GYNAE. 2. specialty- ORTHOPAEDIC 3. chief complaint- left (L) knee pain. 4. brief history - 40 y/o Indian gentleman with no known medical illness came with L knee pain. - History started 15 years back after one episode of MVA. during that time, he had soft tissue injury associated with immediate L knee swelling. L knee X-ray done, showed no fracture. referred to UMMC after episode of joint 'give away' sensation about 3 m after MVA. other 3 series of knee X-ray done n no MRI done. - Currently, has knee pain on regular thermal therapy for pain relief and physiotherapy to improve function. 5. PE finding.. Prof ask to demonstrate relevant -ve n +ve findings. - crepitus over L knee (forget to demonstrate), fluid shift n patella tap -ve (no swelling) - for varus n valgus stress test, pt complaint pain on lateral side of L knee. (not sure?) - quadriceps muscle wasting (mild je kot, i didn't noticed pn..) :( - no evidence of posterior sagging (??), but +ve posterior drawer test. 6. diagnosis From PE, pt has PCL tear. But examiners keep asking me about the progression of the pain. why pt still has L knee pain until now despite it has been 15 yrs since the MVA.. Actually prof want me to say.. secondary osteoarthritis (OA) due to mechanical factors which in this case is PCL tear.. (which i just realized after demonstrate signs to the examiners)
7. questions asked by lecturers from hx, - definition of locking n give away? - progression of the patient? prof want me to relate the injury past 15 yrs n the sustained L knee pain now? ---> secondary OA.. back to the room, - mechanism of PCL tear?---> direct posterior force to the proximal tibia when fall with knee flex.. - next, if the posterior force transmitted upward, what u need to aware? ---> post dislocation of the hip. - investigation for OA and expected findings. - what cause reduce joint space? - what is the management of OA? how u advice pt? so, lesson- must think secondary OA in pt who has previous trauma history.. best of luck kawan2~ reliable source to refer- http://emedicine.medscape.com/article/90514-overview about a week ago Report
Maximilien Liew My case: Schizophrenia Examiner: Prof. Steven, Prof. April, Prof. Choy Lang (External) (Med), plus observer Dr. Koh (psychiatry) Present history until HPI. (Give me the relevant positive and negative.) What is the positive findings in your MSE? What is the cognition of this patient? Formulate your differential diagnosis (at least 3) Give you reasons. No PE Questions from Prof Steven. Write me a prescription for this patient. What are the indication to start clozapine (give 2) What are you concerned off if you start risperidone in a female? What are the side effects of clozapine (name at least 5, he will wait for one by one) Pass to External examiner. What are the criteria for metabolic syndrome? Name all, state which criteria. HDL level less than 1.0, is that for female of male? If you see a patient with this condition, what is you management? What is the mechanism for exercise to reduce insulin resistance? What are the classes of anti-diabetic drugs? (name all one by one) What is the mechanism of action for the class thiazolidinedione? What is the complications that has caused this drug to be withdrawn. What is the common side effects of metformin? Before metformine is introduced, what is the one drug in the same class? Whats the name?
What is the new drug for diabetes and what is the name? What is the other name for alpha-glucosidase inhibitor? Pass back to Prof. Steven. Do you think this patient is at high risk of NMS? What are the risks for NMS? Do you think that this patient is at high risk of suicide? Why? Name me all the risks for suicide? If clozapine failed, what else can you do? Except ECT. What is the social management of this patient? Pass to External examiner How do you tell whether the patients is going to do well or not? What are the factors involved? about a week ago Report
Nor Fauziah lecturer who took u: a/p nortina, prof yop cheng har, prof eugene.. (all of them are so nice!!) specialty: medicine chief complaint: electively admitted for I/V antibitic.. brief history: 59 y.old malay lady, known to have bronchial asthma, hyperCmia, and BRONCHIECTASIS 5 years ago. (thanx God for give me this case...). initially presented with 1 week h/o fever chills n rigors, copious sputum, sob... keep on going here n there for m(x), finally go to tawakkal, do CT scan n confirm diagnosis.. then, for etiology, might be idioptahic.. hv TRO all 1st la.. (TB-no symptoms of TB, mantoux test was -ve , measles, congenital, blablabla).. currently on ventolin, seretide, antibiotic,acapella.. p/e: fine crepitation all over the lung.. reduce vocal fremitus over left long (whole) n right lower lobe... xanthelesma noted.. otherwise, all normal diagnosis: bronchiectasis la.. ;p question ask: 1. how can u come to this diagnosis?? - patient tell me.. hehehe.. btw, history itself suggestive bronchiectasis - long standing cough, copious sputum production, recurrent chest infection... 2. other dd(x)?? - pneumonia, AEBA, but these unlikely... this patient has long
history.. 3. how to confirm d(x)?? - spirometry (obstructive pattern..) CT scan, CXR... 4. let see, what this patient has... haaa CXR.. ok now interpret this CXR... features of bronchiectasis la.. cystic shadowing, blabla...;p 5. what the causes for this patient?? idiopathic maybe... other causes?? (congenital, infectious, etc) 6. how u gonna manage this patient?? - just follow what ummc did.. chest physio, acapella, prophylactic abx, dun forget acute management.. 7. acapella?? how does it help?? - help to clear secretion la... explain about pathophysio of bronchiectasis... 8. long term complication: recurent chest infection. 9. suddenly prof eugene open his mouth... let say, 5 years later this ptt come to u, what u expect to see in her ECG?? right ventricular hypertrophy! initially mentioned left, then he help me to come to answer.. thanx prof!! hehe~ 10. krrinnggggg!!!! u can go now.. thanx to all my dear prof.. u guys are so nice to me... all the best to my dear friends!! dun worry, smile always~ :) about a week ago Report
Faris Yusri emmm..... for my part, i got the same patient as maira.. same questions were asked. Mechanism of injury bla2.. the different is i diagnosed it as ACL tear. i said this because for me, it seems like there is no posterior sagging + the patient said, when he accidentally noticed knee instability, he was able to push it forward. +ve anterior drawers test +ve lachman test on the left. Rigid on the right. however, i still have doubt since patient is not active in sport, doesnt play football or futsal (ACL most likely a sport injury) & the causes for instability is MVA (i'm not sure if MVA can cause ACL as well) other questions are really 100% the same. about a week ago Report
Anis LobotoMe Examiner: Prof. Steven, Prof. April, Prof. Choy Lang (External) (Med), plus observer Dr. Koh (psychiatry) specialty : medicine ? surgery ? psychiatry ?
History : Instruction : Because patient have complicated history, please List down medical, surgical, social problems. ++ Questions . Summarize. Diabetes and HPT : screening, diagnostic and monitoring of blood levels, symptoms and signs of complications especially microvascular, investigations of a Diabetic patient, monitoring of hypertension in diabetics, sexual history(dysfunction), classes of anti-diabetic drugs, criteria for Metabolic Syndrome Poor stream urine: causes of urinary obstruction and symptoms and signs What other causes of polyuria and polydipsia ... pathophysiology ... Hyperparathyroidism : signs and symptoms of presentation, classification of causes of hyperparathyroidism, investigations of hyperparathyroidism, treatment and monitoring of hyperparathyroidism Hypercalcemia : signs and symptoms, causes of hypercalcemia, investigate hypercalcemia, why use corrected calcium, emergency treatment of hypercalcemia (how to examine multiple comorbidities?) ergh . Examination : sensation and vibration examination, demonstrate and name the term (peripheral neuropathy : glove and stockings or mononeuropathy ) Prolapsed Intervertebral Disc : interpret which level (dermatomal) ... Psychosocial aspects in this patient, Findings on Mental State Examination, possible psychiatric illnesses/psychological disturbances in this patient. Esther Lee 1. lecturers who took u: prof BK lim(O+G), prof wan arrifin(paeds), dr KL ng (surgery-not dr michael) 2. specialty: surgery 3. chief complaint: nil 4. brief history: 82/I/gentleman hx of BPH post op June 2010. prior to that, in 2009 one episode of AUR a/w abdo distension, fever one day.no urinary sympt prior, no other GI symp (pain, tenesmus, bloody diarrhoea). presented to A+E, catherized got haematuria, Xray KUB done, no stones.family was called middle of night that pt needed emergency op.found got perforated colon and colostomy was done. 5. PE finding distended abdo,laparotomy scar, left sided colostomy 6. diagnosis:??? discussion was lead to diverticular ds with lotsa hinting 7. questions asked by lecturer (so interested with AUR ended with colostomy, BPH ignored) Do u think that AUR and perforated colon related?
wat can cause perforated colon? why do u think it is a colostomy? complication of diverticular ds wat investigation u wanna do wat do u expect to find in barium enema BK lim was so nice today! hinted so much... hope i din irritate KL Ng by sudden aphasia at the end T.T huhu about a week ago Report
Iu Kwang Kwok My case: Gallbladder Carcinoma , p/m/Hx asthma and hypetension Examiner: Prof Subramaniam (External), Prof Pan (External), Prof CT Tan HOPI: Diagnosed gallbladder ca 7 month ago, presented with obstructed jaudice. 3 days post chemo Presented with Fever assoc with cough and sore throat. Examiner: Prof Subramaniam (External), Prof Pan (External), Prof CT Tan Question: Why do you said this is obstructed jaundice? What is the causes? Can u tell me what is the pathophysiology of him getting pale stool Why he get multiple episode of fever Tell me About hepatitis other than hepatitis B What u will do for this patient for his jaundice problem and the management What will you manage if he come to A n E with the similar complaint and what is ur management (mainly management about neutropenic sepsis) All the best............... about a week ago Report
Ho Kean Teng Same case with kwang kwok(neutropenic sepsis with underlying gall bladder CA) add on=what do you wanna do if you accidental found few stone in the gall bladder and the pt is asymptomatic. mirizzi syndrome. why puritus in obstructive jaundice?bile acid accumulation what cancer cause obstructive jaundice? what medical condition and drugs cause obstructive jaundice? how is the jaundice in pancreatic CA?progressive why periampullary CA will cause intermittent jaundice? about a week ago Report
Sharen Tian 1. lecturers who took u Prof David Choon (Main examiner), Prof Chee (Med), Prof Azmi (O+G) and external 2. specialty : ORTHO (OA knee) 3. chief complaint Left Knee Pain 1 Year 4. brief history 78 chinese lady, Retiree L knee pain for 1 year, worsening for past 4 months..typical OA history. Depression secondary to pain. Lumbar spondylosis. Patient on Cerebrex about 7 years d. Had suicidal thought 3 years ago, on lexapro and clonazepam. DM and HTN for 10 years. I emphasize a lot on social..LOL 5. PE finding Bilateral genu varus more on the left side Antalgic gait Bilateral knee crepitus, left knee loose body Muscle wasting The knee obviously deformed Bilateral hands also OA changes..Herbedens node and Bouchard nodes. Severely OA (but prof didnt emphasize on hand) 6. diagnosis Bilateral Knee OA 7. questions asked by lecturer Why u say OA? Differential : RA - he didn't really agree. He wants Neurogenic claudication. Then I say gouty. Prof Choon : how to diff OA and neurogenic claudication? He ask which 1 more pain when walk longer? I said OA..his reaction "Huh, sure?" Me : I think so Bring to patient, Knee examination. Where is medial joint line, pulses, how to confirm pt had wasting? Manage to guess it...Prof Choon guide me la ^-^ Go back to room Situation: You're the houseman, What to do for this patient b4 surgery CXR, ECG, Knee Xray, AP and lateral. I think they want to show me x-ray. but technical problem. The Prof Choon again, you dont want to take consent?
he interrupt along the way, Dr, when i can walk again? how long can i walk, can i climb stairs, can I drive....many many more I answered him, Prof, I'm very nervous...1 by 1 k..:-) Prof Azmi told prof Choon, "you tortured her enough" HAHA Show him the incision of TKR, consent...FINISH..within 15 MINUTES.. Well...to all my friends, the examiners are really nice... GOOD LUCK~! about a week ago Report
Hwang Ing Siong MBBS(Malaya) 06/11 Final Exam Data Store Hwang Ing Siong 1. lecturers who took u external caucasian (sur), chan lee lee (paed), nik sharina? (pcm) 2. specialty Surgery 3. chief complaint gradual abdominal distention 1 month 4. brief history 53/c/gentleman,underlying colon ca (caecal), c/o 1 month gradual abdominal distention, 2 weeks lower abdominal pain, vomiting 2 days prior to admission. pshx:acute appendicectomy find out to be malignant tumour. Thus, a midline open laparotomy done. 12 cycle chemo. 2nd CT scan revealed stage 4. 5. PE finding anaemia, scars, peritoneal drainage, ascites. 6. diagnosis IO secondary to colon ca 7. questions asked by lecturer - PE: show incisional hernia. do abdominal examination. - in the room: investigations, what iv fluids chosen, electrolytes imbalance of vomiting. show abdomen CT->small bowel obstruction and ascites, ix of acute IO, ix of ascites about a week ago Report
Tan Pei Pei Examiner: Prof Cheah (External-Paeds), Prof Sanjiv, Prof Razif Paeds: Hb H Constant Spring (thalassaemia) History: 8 y/o Malay girl who was dx with this when she was 1 year 5 months old. Currently no active complaint. Increase in frequency of transfusion recently. Serum ferritin: 500, not yet on iron chelating agent. No other side effect of transfusion or infection. PE: demonstrate palpation on splenomegaly. Demonstrate her growth on anthropometric chart Discussion: when to start on iron chelating agent, how, dosage, what is the side effects of iron overloading, what is the cure for thal patient other than Bone marrow transplant, What is HbH Constant Spring, What other investigations for the patient. about a week ago Report
Dana Qurratuaini 1. lecturers who took u Dr.Pan(external), Prof CT Tan, another external 2. specialtyOrthopaedics 3. chief complaint lower back pain 4. brief history 58 indian gentleman, back pain 1 year, radiating down to feet, numbness. Pensioner, previously work with Telekom, involved heavy lifting. history of MVA. MRI done, problem with L4-L5. ADL affected- need wife's help to bath. history of DM, HPT, Epilepsy. 5. PE finding spine terderness, step sign, positive SLR, positive stretch test, sensation,reflex... 6. diagnosis spondylolithesis 7. questions asked by lecturer differentials what type of tumor in this age osteoartritis in spine is also called? definition, mechanism, etiology, age of each degenerative differentials. -spinal stenosis
-PID -spondylolysis -spondylolithesis what most likely diagnoses in relation with previous job. what investigations what you expected to find interpret mri-forward lip of L4 on L5 common site L5-S1 goodluck to my colleagues and juniors ;) about a week ago Report
Jin Hui Ho 1. lecturers who took u Prof David Choon, Prof Chee KH, Prof Azmi, Chinese External 2. specialty Medicine 3. chief complaint 24/malay/ gentleman beta-thalassaemia major. Diagnosed since 1 year++. Monthly transfusion, preHb 6. Ferritin 5000. No splenectomy. Previously on deferasirox, stop 2 years ago. Non-compliance to desferrioxamine now. Hypothyroid, delay puberty. Anaemic symptoms appear 3 weeks post trasfusion. Both parents are carrier. 1 sibling affected. 4. PE finding slate gray hyperpigmentation skin, pallor, maxillary eminence, jaundice,very hyperactive precordium, ESM at upper left sternal edge. Splenomegaly. Tanner: PH 4, G4?? (not sure, they didn't look at it) Peripheral neuropathy-up to mid metacarpal and mid metatarsal, Glucostix- 5.7. Reflex normal, no prox myopathy. 6. diagnosis beta-thal major 7. questions asked by lecturer Why do u think he got hyperactive precordium? How do u confirm it is a spleen? =) Interpret FBC-microcytic hypochromic anaemia. Differential? How to differentiate all? What do u expect to see in PBF? If he is going to married, what will u do? screen the wife.
If she also thalassemia? U want them to separate? Aiyoh..prof...I didn't say that... Patient's automomy, he decide la. Ethics involved in antenatal diagnosis? They are very nice=) Good luck everyone!!!!! about a week ago Report
Swam Ng 1. lecturers who took u Prof Chin (external), prof Stephen J, Prof April 2. specialty Medicine 3. chief complaint Wheezing associated with productive cough for 3 days 4. brief history 48/Chinese/lady Bronchial asthma diagnosed at 3-year old. Very poor controlled. History of taking oral steroid 7 years ago ---> iatrogenic Cushing's syndrome + hypertension Secondary osteoarthritis due to MVA 25 years ago 5. PE finding Cushingoid features Lung findings: reduced chest expansion, generalized rhonchi with prolonged expiratory phase 6. diagnosis Mild AEBA secondary to URTI with underlying uncontrolled asthma Cushing's syndrome 7. questions asked by lecturer (all asked by external examiner) - Important differential diagnosis TRO in this patient - Cause of Cushing syndrome in this patient - Complications of steroid - How steroid causes DM and leg edema - Why patient is still Cushingoid as she already stopped taking oral steroids for 7 years - Investigations for Cushing's syndrome - Control of asthma in this patient - If this patient presented to A&E with AEBA, what investigations you want to do - Signs and symptoms suggested of severe asthma - What are the drugs for asthma about a week ago Report
Wan Nur Ainun Adnan 1. lecturers who took u-prof nik sherina(pcm),prof CLL(dia diam je),external examiner(dia ni diam je n siap tido) 2. specialty-pcm/med 3. chief complaint-exam(no active complaint) 4. brief history-69/M/M--dm, hpt more than 15yrs, gout, IHD 6yrs 5. PE finding-all normal, except loss of vibration(lecturer ask to demonstrate how to check peripheral neuropathy, how ti palpate cardioM, cannot feel, even on left lat position, so had to percusss) 6. diagnosis-dm, hpt, 7. questions asked by lecturer - DM HPT Cx, causes of blackout (patient claimed had MVA d2 blackout), interpret pt result, other Ix beside blood, how to calculate ot creat from age, side effect of drug-statin-myositis, y sodium low in this pt(not sure which drug cause it), what advice you wanna give the pt regarding the disease-control etc, advice on how to make pt compliance to meds. about a week ago Report
DumDum Lay Teng 1. prof yip, prof eugene n ??? 2. surgical 3. per rectal bleeding 4. 73 year old indian lady, c/o per rectal bleeding associated wif mild abdominal pain and loss of weight. history of hypertension past surgical hx: ectopic preg, cholecystectomy and TOP due to German measle 5. colon carcinoma 6.post op laparotomy scar, kocher scar 7. if colon ca: which site n y? investigation: what u expect to see from colonoscopy other easy ix to diagnose carcinoma how long is d sigmoidoscopy can reach risk of synchronous interpret chest X-ray y u wan to do CTscan if CTscan not good enough, wat u wan to do staging of carcinoma management of each staging tis pt need chemotherapy?
if not operable on laparotomy, wat u wan to do? post op complication if post op patient complain of vomting, wat u suspect? wat other sign n symptom u wan to look in post op wat cx of ectopic pregnancy about a week ago Report
Wan Nur Ainun Adnan ni ainura 1. lecturers who took u-prof david choon, prof noor azmi, 1Dr and 1 external 2. specialty-ortho 3. chief complaint-no active complaint- had Hx of MVA 4. brief history- MVA car vs motorcycle- BPI 5. PE finding- Erb's palsy, reduce sensation, muscle wasting, scar at neck region 6. diagnosis- upper BPI 7. questions asked by lecturer- what function can be restore after surg(surg next april), Ix you wanna do- nerve conduction study, can refer pt to what social organisation other than SOCSO, about a week ago Report
Anand Balakrishna From : B. Anand kumar Lecturers: Prof Rokiah, Prof Thong and Prof Chin..(fiuh..the names itself gives baseline tachy but trust me,they are super nice today,..the nicest they could eva be) Specialty: Medicine C/C: 52 y/o Malay lady who is a long standing diabetic pt presented tdy with no active complaint. HOPI: Pt was previously well when she was diagnosed to have GDM durin her first pregnancy. It was a planned and wanted pregnancy. Bookin and scanning was done and it correspond to the EDD. She was well at the beginning just with some morning sickness when she started to developed symp of '4p's around 6 month period of amenorr. Serial investgtn inludin OGTT and she was dx with GDM. Admitted and started on 2 injection regime. Nearing term,was found to have
cephalopelvic disproportion and electively admitted LSCS. Post pregnancy she was on insulin for 2 years because she was breastfeedin. After that she was found to have poor glucose control and started on OHA. This pattern went on for all her 3 pregnancies and after the 3rd pregnancy, she was decided to be kept on insulin cont'..as the OHA is not helpin to control the glucose questn1.why the OHA is not helpin now ? i said the dm itself has progressed frm resistance to insufficiency.. questn2.What are the other factor contibute to poor glcemic control now? i talked bout life style and also the fact that pt has gain more weight. questn3.What syndrome bout weight gain? i start to talk bout metabolic x.talk continously.dont stop.unless if they stop u :P continue with obstetric hx questn4.why pt has to go for LSCS? i said disproportionate CP.and maybe its macrosomic. its betta not to prolong the pregnancy as it has its own complicatn. like SIDS continue with hx questn5.why this patient has tendency for IHD?the DM status and also the high cholesterol level.. questn6.what atherosclerosis consists of? :P questn7.BMI of the pt ? :P continue with history questn8.why its importnt to know when the siblings was dx to have dm ? differentiate IDDM and NIDDM as NIDDM runs in the fmly. we also can assess the other sibling who are not really given adequate DM education..screen for others. summry.. went to see patient. questn9.elicit ankle oedema?what is the cause? i said nephropathy due to uncontrolld DM..what are the changes in renal? BM thickenin and mesangial proliferatn.. questn10.what abnormality with the face..i said it lookd like malar flush..so it could be due to.......hmmm..i ans mitral stenosis.(shit...) can i rephrase the ans,maybe its a facial flush due to premenopausal sx.(fiuh...) :P last questn11.what is the histopathology of CRF?...:P GOOD LUCK GUYS .....
about a week ago Report
Devanraj Selvam 1. Lecturers who took me. Prof Rokiah Ismail (*she was really nice today!), Prof Chin KF, Prof Thong 2. Specialty Surgery + Medicine 3. Chief complaint Elective admission for parathyroidectomy (Tertiary HyperPTH). Known case of CKD for 7 years. Secondary Hypertension (diagnosed at 21 years old) 4. Brief history 36 year old Chinese lady, single, with no family history, congenital problem, or any underlying cause. *I said possibly undetected scarred kidney due to recurrent UTI during childhood. (*Prof Thong said okay) 5. PE finding Post-surgical scar. Oedema causing RLN palsy-hoarseness of voice (*was asked why, what other post-op complications). BP high. Otherwise okay. *I was asked about pallor and leuconychia (*exact location) and the AVF(*why bruit/thrillstalk about different callibre of vessels, turbulent flow). Talk about scar, jaundice, anaemia, describe the mass at the neck. BMI, nutrition, 6. Diagnosis Tertiary HyperPTH due to a long standing CKD with a background history of secondary Hypertension. 7. Questions asked by lecturer Surgical question: If I am performing a parathyroid surgery, how do I do a simple test to differentiate the gland from a fat lump? Remember OT has water. I was like fill the water in a beaker and place the removed specimen. Suppose if it floats, it is fat lump. Why? Because of its density. Phew, Form 4 Physics saved me. Then the anatomy, size of gland. Hypocalcaemia. What clinical test. Chvostek and Trosseau. How do you do it? I could answer until show me how the hand would finally lie with Trosseau. I did like a claw hand because I thought it was carpo-pedal spasm. They were smiling and Prof Rokiah asked whether am I sure. I sheepishly smiled and said no. Apparently it is like http://www.kuwait-md.org/?q=node%2F923 . Haih. Very brief management of the CKD. Prognosis, how would you counsel the patient. I can't remember much la, they did ask few questions here and there. But I was glad when it finished. My final question was how a patient with CKD would get shortness of breath. I told the anaemia in CKD pathophysiology.
I got the same patient with Sahrul (*Tambah la apa-apa if I left out). Apparently they rotate 2 students per patient. Good luck guys! about a week ago Report
Hapsah Aripin 1. lecturers:prof wan ariffin, prof bk lim, dr kl ng, dr chew 2. specialty:paediatric 3. chief complaint: electively come for exam 4. brief hx: 8y/o, malay, boy Down's syndrome with congenital heart ds at birth..but the heart ds disappeared at 5month old...has global developmental delay..diagnosed with epilepsy last year n admitted twice..then,treated with lamotrigine. Other than that, he was also diagnosed with fatty liver. PE:features of down's syndrome, short stature, other systems were normal, DA delay (ht n HOC below 3rd centile, wt at 3rd centile- but he want me to said correspond to what age) 5. Question: -what do u think the causes of cong ht ds in his case?PDA, small VSD -how do u diag down's syndrome antenatally?US-nuchal thickening, amniocentesis-chromosomal study, he mentioned about 1 more test but i don't know -problems a/w down's syndrome..all in sunflower book -how duodenal atresia present in utero n after birth?polyhydramnios n bilious vomiting 2-3 hours after feeding -how long u want to treat pt with antiepileptic?until 2 years seizure free period -what is d name of association for Down's syndrome in M'sia? Down Syndrome Association of Malaysia.. -what is d mx u want to do after diagn d pt having down's syndrome?genetic counselling, check other ass prob such as hypothyroid -what do u want to tell parents to ease their burden taking care of down's synd child? they want d tve side of down's syndrome?they are adorable n funny -write the genetic for this pt's chromosome...47 XY -did u explore the mother's understanding about down's syndrome?i didn't but shoudl do -why do u think d pt is short?hypothyroid -pt hv hypopigmented spot above the eye, is it significant since pt is also having seizure n down's syndrome?i said yes..he asked what term can we use to classify it?i dunno, maybe neurocutaneous sign kot -can u classify this pt's IQ?moderate-severe do u think he has bad down's syndrome?no becauce he doesn't hv any serious illness like tumour about a week ago Report
Benjamin Lim Prof Sanjiv Mahadeva ( he was runnign da show, asking most of da questions....and dun expect him to hint u, he will never) Prof Cheah Fook Joe from UKM.....keep tambahing question to Prof Sanjiv Prof Razif....silent mine is same as anis.....malapetaka i think.....1st,i started out late, cause they cannot find da patient, 2nd, when i was doing halfway, anis came in with his lecturers for PE, another 10 minutes, total about 20-minutes....and i was given extra 10 minutes ( eveyrone given extra 10 minutes), so 50 minutes to clerk and PE for all da problem below, i was like, i am fking dead !neway, summary of da probem No CC, purely for examination purposes, TCA 24 April for ESWL f/u 25 years PTA: Right inguinal hernia repair with vasectomy 12 years PTA: DM, HTN 10 yr PTA: KUB calculi, surgery done to remove in pelviureteric junctiion, transfused blood once,r euccerence twice, with ESWL 10 yrs PTA: bilateral cataract surgery 10 yeras : dun ask me why, ev erything oso 10 yeasrs....PID, under ortho red team f/u, cured by physiotherapy 7 yeras PTA; Ix for Hyper Ca: Parathyroidectomy done 6 months PTA: LUTS, Uro f/u, under some medication, which i dunt know PE: peripheral neuropathy : glove stocking, and also L5 dermatome interestingly... and INTERESTINGLY!!!!! got bilateral pedal edema up to knee....i was like wtf....no bibasal crepitations i was stuck in Hx, and PE quite long, no reach Ix not Mgmt...... i thought i presented quite well m Hx ( despite being interrupted), can answer some of their question, but some i cant answer, but stuck a bit in PE, haih.....anyway.....hope i can pass and pray dat they can understand my case is a dam complicated with multiple prob case and pass me.....reli need lotsa lucks here.... about a week ago Report
Sarah Liyana 1. lecturers: Dr.Pan(external), Prof CT Tan, Dr. Subramaniam (external) 2. specialty medicine
3. chief complaint cough, 5 month 4. brief history 52 malay gentleman,cough 5 months, a/w sob, orthopnea, chronic smoker, work related to plumbum n radiation exposure, also had back pain and weakness right upper limb and lower limb 2 weeks ago, mother had colon ca, . PE finding-scar at right lower zone lateral side, percuss: dull at right lower zone, reduce breath sound at right lower zone 6. diagnosis- lung ca mets to brain and bone 7. questions asked by lecturer - pathophysiology orthopnea, given CTscan of brain and need to interpret, type of lung ca, from what cell the cancer is, how to comfirm diagnosis, differential for back pain, how to deferentiate malignant or degenerative causes...how to relate the brain ct scan finding with patient right upper and lower limb weakness about a week ago Report
Chin Yun Ann MBBS(Malaya) 06/11 Final Exam Data Store Please present your long case following this format. 1. lecturers who took u Prof BK Lim, Prof Wan Ariffin, Dr KL Ng 2. specialty Obstetrics 3. chief complaint no c/c 4. brief history 30+ years old, Malay lady antiphopholipd syndrome 1 yr recurrent abortion P7G4+2 no GDM or Hpt well with no cx 5. PE finding transverse lie no features of APS 6. diagnosis prof didn't ask
7. questions asked by lecturer How to manage patient if presented to you? What to monitor? How to deliver? Can undergo vaginal delivery? What sign in uterine rupture? How to induce pregnancy? about a week ago Report
Raymond Kok same patient as Salahuddin Abd Jaafar 1. lecturers: Prof Khoo Ee Ming (PCM), Prof Adeeba Kamaruzzaman (Medicine), Dr Zygmunt (initially silent) 2. specialty: Medicine and PCM 3. chief complaint: no active complains. came in for exam. under follow up at RUKA and O&G for: endometrial Ca (post-TAHBSO) asthma deep vein thrombosis obesity and Diabetes Mellitus 4. brief history suhaili, 35, malay, lady a) asthma, since childhood, well controlled, currently on bicotide and ventolin b) dvt, currently on warfarin 8mg OD, INR:2-3, well controlled. had 3 episodes c) endoM Ca, done TAHBSO, 15 round of chemo, and brachytherapy. currently well, no sign of mets/recurrence d) Diabetes: currently on metformin 850mg, diamicron 1 tablet OD, insulatard 10U before bed. 5. PE finding left leg swelling with varicose vein 20cm Pfannenstiel scar post TAHBSO 6. diagnosis uncontrolled DM with obesity. and currently on medication for DVT 7. questions asked by lecturer during PE: please examine her lower limbs. demonstrate how u confirm swelling (measure circumference of calf), what is the causes of unilateral leg swelling, what can be the causes of the swelling in this patient (uterine ca mets compressing on lympahtic drainage of left lower limb) back in room: how would you manage this patient knowing that she has the above problems (INR monitoring, Diabtetic control and complication detection), what blood Ix would you do for her? if HBA1c is 11.1 what does it mean and
what should you do? if protein 1+ what does it means does it mean she has diabetic nephropathy? what are the other causes? what sort of diet regime do you know of? her current BMI is 37.7, what should be the ideal? (18-22.9 for asians) that's still a long way to go for her and they laughed among themselves good luck ppl.. about a week ago Report
Shahila Ardain same patient like winnie... other question been asked: - what other causes can present as obsessessive - psychiatric formulation - management... about a week ago Report
Saturveithan Chandirasegaran 1. Lecturers Prof Mary Ann (external from United States-O&G) Prof Sajar (PCM) Prof Lucy Lam (Paeds) 2. specialty O&G 3. chief complaint GDM 4. brief history -34 years old Malay lady, -G5P4,at 34 weeks, -history of stillbirth(1st pregnancy) -Right oophorectomy due to teratoma -high risk of GDM -otherwise normal antenatal history and emphasize on GDM 5. PE finding -general examination,thyroid,breast was normal -SFH:34 weeks -singleton,longitudinal lie,cephalic presentation,not engaged, -adequate liquor volume & estimated birth weight-2.5kg 6. diagnosis
GDM 7. questions asked by lecturer (mainly by Prof Mary) -Tell me about GDM...everything...screening up to management -her risk factors for GDM -investigations...PIH,GDM -how you will manage her from now..34 weeks until the delivery -complications of GDM...fetal and maternal -classical picture of baby of a GDM mother...management... -then,started on asking questions on DVT -Metabolic syndrome-define and elaborate -half life of bromocriptine... -Last question, 2nd stage of labour, head is out, wat u wan 2 do?? Mc Roberts manouvre....elaborate.. -Bell rings!!!! Done... :) Good luck friends :) about a week ago Report
Lia Lea 1. lecturers Prof Lucy(Paeds) Prof Mary Ann (external from United States-O&G) Prof Sajar (PCM) 2. specialty : Paeds 3. chief complaint: nil 4. brief hx 3 y/o, malay, boy diagnosed to hv Down syndrome, immediately after birth together with PDA h/o recurrent chest infection and admission to the ward newly diagnosed to have hypothyroidism after presented with constipation 5. PE all signs of down syndrome developmental delayed resolved PDA 6. dx: downs syndrome with hypothyroidsm 7. question asked: -as he is having recurrent chest infection, they asked about asthma sx n med a bit -hx of last admission: more detailed -comment on development
-other sx of hypothyroidism -bring to patient: show signs of down syndrome - do DA in front of prof -go back to examiner room again: -asked to how to dx down syndrome antenatally -comment on growth chart: why weight not really affected, but height is affected: answer he's having hypothyroidism, apetite good but short stature -how to assess response to thyroxine, as he having hypothroidism -i answer, then immediately, bell rings....finito about a week ago Report
SOh Reza Prof Sajar (sangat baik dan supportive), Prof Mary Ann (dok senyum sampai abis exam) and Prof Lucy Lum Primary Care Medicine Chief complaint Currently, came for exam purposed, but presented 15 years ago with chief complaint of seizures for one day duration Brief history 44 years old Malay gentleman He was apparently well until 15 years ago, when he first develop seizures while sleeping (around 3-4am in the morning) - Upper limb held in flexion postion - Drooling of saliva - Bitting of toungue - Uprooling of eye ball - Last for 5-10minutes - Noticed by his wife - Nothing much done by the wife as she was panicking Post ictal he develop short term memory loss(canot remember the date,time,whether hes working or not) - lasted for one hour - associated with dizziness For the first time, did not seek medical attention as he taught it was normal. Then 3-4months later, develop second episode which was similar the first one but still did not seek for medical treatment Only for the third time he seek for medical attention as it was advice by his uncle So within one week, went to Hospital Tampin and was refer to PPUM for further investigations In PPUM, he was arranged for EEG was told the result was positive and was started on tegtigrol for 3months and withdraw because of side effect (rashes) Then medication was change to phenytoin until now Since 1997 up to now, his condition was improving (frequency of attack 1-2 times/ year) compared to previous one (3-4 times per year) and less bleeding of
tongue bitting For compliance Attend regular follow up (6 monthly), compliance to his medication, never miss medication - Last attack 6 months ago - Last follow up last 2 weeks, also noted BP high (140/90) Social history - Not affecting his jobs or daily activity as it usually occur during sleep - Chronic smoker for 20 years - No history admission because of seizure Sytemic review No low, no loa, no fever, no chronic cough, no contact with tb, no hemoptysis - No symptoms of hypoglycemia before attack - No early morning headache, no nausea, no vomiting, no blurring of vision - No chest pain, no sob - No olugouria, nocturia, urinary symptoms, no altered in bowel habit - No calf pain during walking, intermittent claudication - No history of MI/TIA/Stroke before PE findings O/e alert, conscious, responsive - no pedal oedema Vital sign BP 140/100 PR 80bpm NV RR No SC RR 20breaths/min T - febrile CNS Tone normal Power -5/5 Reflex Intact Sensation Intact Plantar Downgoing CVS Unable to locate the apex beat (huhuhuhu) S1,S2 heard, no murmur Lung Hyperinflated with loss of cardiac dullness and liver dullness Vesicular BS, equal air entry, no crepts or rhonchi Urine Dipstick Protenuria +1 Diagnosis Epilepsy with hypertension Questions asked 1. PE Comment on peripheral xm No pallor, no jaundice, no cyanosis, hydration status fair - Elicit the upper limb reflexes (biceps) - Demonstrate how you check for apex beat as I said I was unable to locate it - Why do you think apex is not palpable in this patient Bcos im shivering (they
all laugh..huhuhu) , wut else? - Thick chest wall - Hyperinflated lung (after prompt by examiner as she ask the relation between smoking and lung - Demonstate hyperinflated lung - Show me the normal site for apex beat (pointing at 5th left ICS) make sure show the midclavicular line and count the intercostals space from 2nd - Did you check for the fundus Im sorry I didnt have much time to do that but I would like to complete my examination by checking fundus for hypertensive retinopathy, sign of papillodema 2. In the room a. What do you think the patient has Epilepsy b. Why, give your reason repeated episode history of seizures c. How do you think hes condition now well controlled and getting better with treatment as frequency reduces (1-2times year) compared to previous one and currently tongue bitting less bleeding d. Is there any specific causing the seizures from the history, I could not find any specific reason for the seizures to occur as he had symptoms of low/loa, no fever, no cough, no contact with tb, no hemoptysis, no family history of epilepsy/brain pathology, and only occur when he was sleeping e. Let say the patient present to you for the first time, what are the things u should consider Considering the age of patient & late onset of seizures, few differential diagnosis that I should consider i. Intracranial pathology such SOL brain tumor ii. Infections Meningitis, encephalitis, TB abscess iii. Metablic disturbances Hypo/Hypernatremia, Hypocalcemia, Hypogylcemia iv. AVM f. For the metabolic cause, which one the most important cause of seizures Hypoglycemia (fair enuf) g. Let say the patient had brain pathology, how usually they present Early morning headache, nausea, vomiting, sign of papillodema h. If u suspect the patient hat tumor in the brain, what investigations u wanna order CT scan of brain to look for the lesion/mass, location, the size, shape, infiltration to surrounding structure, midline shift, inverventricular extension i. Now the EEG show patient had epilepsy, what is your further management? List problem that patient had now i. Epilepsy well controlled ii. High BP j. For the epilepsy put patient on regular follow up, make sure he is compliance to medication, and never miss medication k. How to access pt compliance to medication other than asking him (lost for a while), what are expect to see in blood? oh the level of drug within the blood system..huuhuhu l. How do you advice patient for his epilepsy? What is the absolute contraindication for the sports the he can not do? Avoid driving the car (if possible ask the wife to drive the car), certain jobs (lorry, bus driver, use the heavy machine like the construction site should be
avoided), for activity (no cycling, swimming, suddenly terkeluar football (zzzzz,then examiner ask why?hahahahh) m. What about the high BP Lifestyle modification smoking cessation, regular exercise, reduce weight Suddenly KRINGGGGGGGGGGGG!!!!!!GOSH!!!!Tak sempat abiskan..huhuhuuh P/S: Hopefully we all can pass..The examiner is very nice and try to help to so that we can pass..Gudluck everyone=) last Monday Report
Nor Atifah examiner: prof cheah, prof azhar, prof CT Tan speciality: paediatric! 17y/male.known case of thal major since 2 years old. regular BT, desferal, vit c. also on testosterone n thyroxine( miss these!!). Q: how u want to ask about effort tolerance in ptnt..? 2) PE: assess growth. ptnt is short. how u know? assess thyroid fx, secondary sex characteristic. 3) Ix. explain about finding in Hb electrophoresis. 4) what is the mode of inheritance for thal. last Monday Report
Khalidah Zainan lecturers who took u Dr Pan (external) Prof Mary (paeds) , Dr Nageulis (O&G) 2. specialty Ortho 3. chief complaint come for exam.. when ask what illness he had, he said back pain arthritis n dm.. so I asked which dr asked him to come.. DR chris.. so i focus on back pain 4. brief history back pain 1 year- asc with bilateral radiculating pain .pain during walking around 10 mins relieve when bending forward n rest .. no night pain, LOW,LOA,fever.. BO n urine Normal,neurological normal. no trauma, no history of artery prob (rule out intermittent claudication) also had bilateral knee pain , swelling, symptoms more like mechanical pain.. no morning stiffness , taken glucasamine (most likely OA)
func- normal, but previously active in sport currently only do yoga.. no more running,jogging.. pt expectation- don't want surgery, afraid bcome paralyse 5. PE finding stooped posture,shoulder tilt left, reduce extension, + SLRT left leg.. power normal. present of gloves n stocking numbness.. lost of proprioceptive.. knee- muscle wasting, swelling +patella tap, crepitation, 6. diagnosis lumbar stenosis secondary to spondylosis 7. questions asked by lecturer difference spinal claudication n intermittent claudication.. differential..why not malignancy... what type of malignancy do u expect . 2dary tumour... what ix u want to do.. which one better xray or MRI- so each time i did examination, he asked me q.. n he said SLRT + if <70 degree. i answered 60 dgree.what nerve u check for dorsal flex.. sciatic nerve. need to read lumbasacral xray-osteophyte.. last Monday Report
Thye Chee Keong 1. lecturers who took u: Prof Zuraidah (PSY), Prof Zygmunt, Prof Dunnowat Singh 2. specialty: Psychiatry (PSY) 3. chief complaint:19 year old Malay girl [Low mood and palpitations for 5 days] 4. brief history: Symptoms started since 16 years old when forced by parents to attend boarding school. Had very low mood, cries all the time, loss of interest, concentration, energy ans so on la. Saw a doctor and given Lexapro but not compliant and symptoms unresolved. Stopped schooling until now (didnt attend form 4 and form 5) but took SPM as a private candidate. Was not treated until Janury 2011 went for a private hospital. Complained to the doctor of [POOR CONCENTRATION], diagnosed with ADHD (gasp!) and given Ritalin and ?Somese. She DID NOT OFFER FULL HISTIRY TO THE DOCTOR. One month later, admitted to UMMC for overdose of Ritalin and Somese and rediagnosed as MDD. Prescribed with Lexapro, Zeldox, and Lorazepam when needed. Currently no mood symptoms. NEVER psychotic. Denies substance. Multiple suidide attempts (or parasuicide?) 5. PE finding: Normal MSE. Very good emotional and intellectual insight. Was asked to do thyroid exam hahahaha
6. diagnosis: MDD in remission state. 7. questions asked by lecturer a) Provisional diagnosis b) Differential diagnosis c) What medical condition you wanna suspect? [Hypo/Hyperthyroid] d) Let's say she's aggresive and suicidal now. How you manage? [Biopsychosocial lo. Just throw everything in] e) WHY do you think she does not have dysthymia? [Poor functioning] (almost dug a grave by saying dysthymia as differential diagnosis) f) WHY SSRI is the best drug? [Less side effect, tendency to overdose thus SSRI overdose is not fatal] OK that's all folks. All da best last Monday Report
Jareth Chong Chan Teng 1. lecturers who took u -Prof.Azad,Prof CT Lim and Dr Sofia 2. specialty -Surgery 3. chief complaint -67 y/o Chinese gentleman who work as a lorry driver -electively admitted for surgery tomorrow -history started from May 2010..presented with lower urinary tract obstructive symptom like frequency, incomplete bladder emptying, intermittency, terminal dribbling and poor urinary stream. No symptom of incontinence, nocturia or straining. One day later, presented with gross haematuria for one episode during the morning urination. No pain, dysuria, fever. Went to private clinic and referred to UMMC. Investigation was done show high PSA,CT scan and MRI and diagnosed. Start with medication which only take at night. Regular follow up at UMMC with PSA monitoring and it is fluctuating around 12 to 19 mg/dL. Currently do not have obstructive symptom except poor urinary stream.
Past medical history of bronchial asthma--well controlled Questions asked by lecturer -history:1.why u specially stress he is a lorry driver?cos they may be have multiple sexual partner and he will prone to STD and get urethral stricture 2.U mean he is sexually active?(forgot to ask)..why is it important in this case? cos treatment will cause sexual dysfunction..psychosocial impact. -PE:Negative finding..ask to show what i have examine.. then i show no evidence of jaundice, anemia, hepatomegaly,spine tenderness(why?spinal metastases),inguinal lymph node -Ix u want to do?....i forgot to order UFEME..then prof prompt lo like ask how to investigate haematuria?i answer ultrasound and cystoscope...then he give me the answer UFEME. interpret UFEME and what information u can get from it and rule out other cause of haematuria. -PSA 9+ mg/dL?wat do u think?u want to do free or total PSA?which one? -how to do a transrectal ultrasound and biopsy?have u see one?wat is the complication? (bleeding, introduce infection) -how would u manage this patient..let say is early stage?i answer surgery like turp but actually prof want radical turp. -hormonal therapy..complication of orchidectomy?haha..osteoporosis -any role of chemotherapy?hormonal therapy better than chemotherapy -if patient come to clinic..how u monitor?history and pe to look for relapse and monitor PSA -wat is the prognosis..let say in early stage?good. good luck..my fren! last Monday Report
Norawaida Razali 1. lecturers who took u ----prof sofiah(o&g), prof azad(surgery) & prof ct lim(paed) 2. specialty ---o&g 3. chief complaint ---none
4. brief history ----40/m/g5p4 (one of the child is IUD at 38 pog)/currently at 24 pog.previous 3 pregnancy delivered via elective lscs.no other medical illness. 5. PE finding -----normal.SFH is correspond to date.got Pfannenstiel scar. 6. diagnosis -----normal pregnancy with previous 3 LSCS. 7. questions asked by lecturer ----why i said g5p4 instead of g5p3+1?..it is because the child is at 38 weeks already.the +1 is because of miscarrige less than 22 weeks. ----because this is normal pregnancy,they give situation if she had gdm..how to diagnose...screening test..value blood sugar..teatment ----mode of delivery for this current pregnancy ---consent before LSCS ----advice aftr deliver the current pregnancy gud luck everyone!!! last Monday Report
Zarith Natasha 1. lecturers who took u prof wan ariffin prof saw aik Dr (external) 2. specialty paeds 3. chief complaint generalised edema 1 week prior to day of admission 4. brief history generalised edema x 1 week- periorbital edema, ascites, UL & LL swelling, labia majora swelling. associated with diarrhoea x 3days. no sob,no chest pain, no jaundice, no fever no URTI symptoms. PU-normal. admitted to ummc for 2 weeks treated with steroid and albumin. achieve remission and discharged. then after one week, patient came for follow updevelop abdominal distention-re admitted. 5. PE finding
currently well.no edema. 6. diagnosis steroid dependence nephrotic syndrome 7. questions asked by lecturer -what is ur provisional diagnosis? and y? -what are the differential diagnosis? -cardiac,liver failure -do u think this patient is likely to have cardiac/ liver failure? - no, cause no symptoms suggesting cardiac or liver failure. -what is the correlation btw edema(in nephrotic) with diarrhoea? -what is the pathophysiology of edema in nephrotic syndrome and cardiac failure? oncotic pressure in nephrotic whereas in cardiac failure there will be increased hydrostatic pressure. -what other local causes of swelling? in the LL? - DVT cellulitis? in stroke patient? - immobility. went to patient's bed-where and how do u check for edema? pitting edema in LL, shifting dullness, respiratory for pleural effusion. others like periorbital edema, genital swelling and sacral edema. back to discussion room: -what diagnostic ix? -what are the diagnostic criteria for nephrotic? -what is the significance of creatinine to protein ratio? -what autoimmune condition can lead to nephrotic?- SLE, IgA nephropathy in children -discuss management -what are the indications to start on albumin-hypotensive.other than that? (i dont know) -do u think this patient is steroid resistant. i said no. but prof wan gave me the 'are u sure?' look. -what advice would you give to the parents? - compliance to drug. diet control. -what are the acute side effects of steroid? infection... ring!!! goodluck guys!xoxo last Monday Report
Azzah Aris examiner: prof mary, dr nuguelis, external specialty: paeds. 2yrs/malay/boy. came with cough 2m ago. just newly diagnosed asthma 1m ago. PE: no positive finding. dis child so irritable. cant do anything! Q:
1. how to diagnose asthma (used bronchodilator relieved or not?) 2.PE: whut is harison sulcus? in what situation u see clubbing? where to look for eczema, in severe asthma what u want to look for? (she want growth. so dun forget to plot chart) 3. if patient take steroid, did he will get cushing? what SE of steroid? 4. if patient have uncontrolled asthma, what u want to do? (asses compliance, mother know to used chamber or not, add another drugs) 5. what investigation u want to do? 5. JiEa AmIr 1. lecturers who took u~ prof azad,prof ct lim,prof sofia 2. specialty~surgery 3. chief complaint~painless hematuria 4. brief history~68y/o chinese gentleman presented 6 month ago with painless haematuria for 1 day. Assoc with LUTS and lethargy. No LOA n LOW. Non smoking. 5. PE finding~not much for abdmen n other system..PR~irregular prostate,cannot feel median sulcus,firm 6. diagnosis~ Prostate cancer~early stage,not mets yet 7. questions asked by lecturer ~diff diagnosis ~inv~ LFT, RP for wat? normal value psa? they gv me d value n ask whether high or not, TRUS n biopsy,wat complication can we get? n all about imaging inV.dUN 4get bone scan. Then, bed site~ wat u want to look?? demonstrate hw to check for bladder for urinary retention..wat u xpect if there is mets to lung? n finding for PR..luckily,i did d PR..=) wat do u think about this patient body build? Then, went to d room again.... ~ wat mx dat u want to do? How to take consent? wat complication from d surgery? wat other mx if pt refuse surgery?~hormonal therapy n radiotherapy ~wat risk factor for prostate ca for dis patient? wat diet can cause prostate ca? milk n fat..haha..prof azad tell me... ~ then prof ct lim ask pathophysiology haematuria...errkkk..then,kring!!!!!!! save by d bell~~heee last Monday Report
Wang Jie 1. Lecturers Prof Mary Ann (external from United Kingdom-O&G)Dublin Prof ong (Surgery) Prof Zuraini (PCM) 2. specialty O&G 3. chief complaint Postmenopausal painless per vaginal bleeding 4. brief history -67 years old Chinese lady, -P5,2 months history of abnormal pv bleed -had abdominal bloatiness with significant constitutional symptoms LOA,LOW and lethargy -The pv bleed increase in size and more frequent and with blood clot -No abnormal vaginal discharge or any foul smelling discharge no any dyspareunia as husband pass away 10 years ad -no any mets symptoms like tenesmus, bone pain, jaundice or any SOB -However, increased in BO 3 x times per day occasionally recently but no abd pain and had colonscopy done at private hospital but no abnormalities - had knee pain recently also and was agg by movement and relived by rest assured by doc is ok just arthritis and given glucosamine -Risk factors: menarche at 22 years old, no sexual promiscuity but unsure of husband , no vaginal discharge or genital tract ix b4, didnt smoke but husband do smoke at home regularly and later succumbed to it by lung ca, no OCP - Pt had done before polyp removal 10 years ago with similar presentation with bleed and dyspareunia. Biopsy normal finding B4 5 mins end clercking, pt only told me had IHD before 20 years ago and maybe angioplasty and on aspirin, antihypertensive and other CVS medication. I ad asked pt initially 5 mins got PMH ,any admission , pt said no...really SWEAT! - menopause 10 years ago and not taken any HRT and no symptoms at all -not on any supplement of vitamin or calcium only normal diet and regular brsik walking at house compound -had 5 children all breasfed and husband died now lives in Ansun with her youngest child -regular menstrual history and had regular pap smear every 1 to 2 year. (Have to ask Last Pap Smear and the result! as examiner marked down this point i noticed) -otherwise screen through MDD and any good social support from family -got guilty, sadness but no suicidal ideation...no MDD but only depressed a bit..and now ok as good support from the children otherwise just present as usual 5. PE finding -general examination,temporalis wasting but normal BMI 23.1l -abdomen no distension, no scar, no dilated vein, no obvious mass seen, many
red papule Campbell de Morgan i think in elderly,examiner said ya -Suprapubic mass 3x7 cm, hard,dull percussion, can get below and can get above, globular shape,no bruit -Inguinal bilateral lymphadenopathy and liver 3 cm, no jaundice -Pain had pain in the left hypochondrium ,umbilicus and left flank and very very vague mass around. i did present but luckily examiner din ask further..no ascites. very high suspicious of peritoneal mets as pt got tell me in history there was fluid accumulation in the abdomen b4 that.. -be gentle and good to pt at least it will please the examiner and also ask any pain b4 u do or b4 examiner ask you do again, tell examiner very painful and they wont let u cont..haha 6. diagnosis Stage 2 cervical Carcinoma (told by pt in Mandarin, please know the chinese terminology for dx if you think mandarin) 7. questions asked by lecturer (mainly by Prof Mary) -Tell me risk factors for this pt and also what will be the causes u have to rule out..talk about the postmenopausal bleed. -Investigation u do in the clinics: she wants speculum in which i managed to answer at last,.i said i thought that is under examination..then the other inv? she wants ultrasound of cervix tv, sweat -other ix? do usual blood FBC, LFT, RFT and also CT scan to stage -wat is the unusual thing in this pt? i said is risk factors not many in this pt?yup -others? a..u know how many percent of the smear negative pt had cervical cancer? i said quite high from my study..but i dunno the figure..around 20%? nope is 67% !! so precise...lolx -Wat is the staging of the cervical cancer? tell me? tell until stage 2 she was ok ad - U tell about cone biopsy..tell me about it.do when there was no spread of cancer and early focal lesion//she said for premalignant lesion.. -how you will manage her? aa...from pcm view, as prof zurainini there, i said all the explain educate, counsel and asurrance..haha she doesnt want it obviously -So for stage 2a pt, i would do Whertheim...she said no! in UK limted only to stage 1 pt..what is whertheim? and tell little about it..how do u think pt had whertheim will have? err..very bad as all the lymph nodes being removed and it will cause many problem..and she said YES! and she asnwer herself.. -So why? Err...pt had low survival chance from stage 2 as maybe there is spread -Then how u mange her? give her radiotherapy with chemotherapy..then ring ad p/s Good luck to all my fren!!! last Monday Report
Er Lz lecturers: prof zuraida(psy), gurdeep singh, and one mat salleh (dunno from where)
Specialties: surgery chief complaint: acute abdominal distension with epigastric pain a/w unable to pass urine and constipation X 1/7 brief history: (patient is not very educated, could not tell the diagnosis, could not name the doctor who asked him to come for exam). his chief complaint was almost 2 months ago. at that time he was admitted to sri kota hospital in klang and then only referred here. i totally hv no idea what's wrong with this pt until i saw his ultrasound report from sri kota hospital saying that he has necrotizing pancreatitis. the abd distension was acute, n epigastric pain was at that night itself. the previous night he consume alcohol as usual. PMH: hyperuricemia and hypercholesterolemia not on treatment chronic smoker and alcoholics for more than 20 years, unemployed. * beware: his complaint of unable to pass urine has nothing to do with his current complaint. it was there for long time, n he has symptoms suggestive of BPH. PE: tatoo at suprapubic area. 2 drainage tubes with bags at left hypochondrium and left loin draining some green brownish fluid. a mass 10 X10cm found at the left hypochondrium region, non-tender, smooth. per rectal - enlarged prostate with smooth surface. diagnosis: pancreatic pseudocyst secondary to acute pancreatitis. questions: -differential diagnoses for all his symptoms -causes for pancreatitis (memorize the GET SMASHED in Oxford handbook) -causes for a mass at left hypochondrium region -what is the fluid in the drainage bag -investigations to be done -interpret CT scan (the computer was opened with the patient's CT scan. i was asked to show him the normal structure first) -what would u see on the CT of someone with chronic pancreatitis -how to manage in the acute setting -what analgesic to give -what is the function of pancreas (exocrine and endocrine) what complications would they get in chronic pancreatitis -what is insulinoma and glucagonoma and what would they present with? the bell rang. good luck. last Monday Report
Lim Hooi Min 1. lecturers who took u Prof Saw Aik (ortho), Prof Wan Arrifin (pead), external examiner 2. specialty: ortho, sport 3. chief complaint: right knee pain 1 year 4. brief history: young/m/man, injured of right knee when playing football. Pain, swelling, restricted movement. giving way, locking, pain intermittently. otherwise unremarkable. stressed on social history. 5. PE finding full knee examination. parapatellar effusion, positive drawer test and Lachman test 6. diagnosis right ACL and meniscus tear 7. questions asked by lecture wat do know understand about giving way and locking mechanism of ACL tear Causes of locking origin and insertion of ACL,function and mechanism of action Bedside: more like a short case rather than a long case full knee examination: while performing examination, examiner asked about wat to test for origin and insertion of medial colleteral ligament? wat other things u wanna check: neurovascular examination wat is ur management for this patient? I would like to do x-ray knee and MRI knee. tell me wat u aspect to find in x-ray knee, MRI. (ring..........) last Monday Report
Sam Sim Yap Khoon Sim 1. lecturers who took u Prof Azhar, Prof CT Tan, Prof Cheah(external) 2. specialty Orthopedic 3. Come for follow up Chronic osteomyelitis of left humerus for 27 years.(ya, no mistakereally the upper limb) 4. brief history
A 34 years old Indian gentlemen, with the background history of chronic osteomyelitis for 27 years, no history of trauma, infection, immunocompromise that predispose to the chronic osteomyeliis. No loss of weight or loss of appetite and no history suggestive of malignancy. Since then, have multiple admissions to the hospital because of similar problem but never had sinus noted and no discharge. Other medical illness: skin fungal infection, low back pain(they are not interested in the low back pain), gastritis. 5. PE finding Multiple surgical scar noted at the left upper armwasting of muslelimb length discrepancy(learn how to measure upper limb!!!) 6. diagnosis Chronic myelitis 7. questions asked by lecturer What do you think the causes of the gastritis?...pathophysiology? Examine the patient. Muscle wasting and they want the limb length discrepancy!!why you think the causes of limb length discrepancy?? Show me what you check for chronic osteomyelitis?? Did you measure the forearm limb length??...and singnificant?? show range of movement: shoulder and wrist, pronation and supernation perform ulnar never examination and what muscle supply that action investigation??...basic all normal!!...after you say x-ray, they show you!!!....discribe management.not able to finish then ringgggggggggggggggg. last Tuesday Report
Ayu Anastacia lecturer: prof zuraida,prof gurdeep,external examiner specialty: psychiatric hx: bckground history of MDD,with suicidal attempt previously, and diagnosed with ADHD since 16 year old. younger brother had ADHD. pe last Tuesday Report
Angel Kwan 1. lecturers: Prof Eugene, Prof Aisyah, Prof Wan Azman 2. specialty: O&G 3. chief complaint: menorrhagia X 2months + partially controlled asthma
4. brief history: menorrhagia x 2 months (no anemic symp, no constitutional symp & no coagulopathy symp), asthma (partially controlled: nocturnal symp, activity limitation, acute reliever>3time/week, last attack 1 month ago.) 5. PE finding: abd examination (no hepatosplenomegaly, no pelvic mass also). Demonstrate how to palpate for pelvic mass. Show the margin of abdominal U/S coverage & pelvic organ situation in patient) 6. diagnosis: uterine fibroid + partially controlled asthma 7. questions asked by lecturer I. menorrhagia Q''s: a. what further P/E u want to do? (PR exam, VE & speculum for cervical mass) b. During speculum exam, what u want to do? (pap smear & endometrial sampling) c. What's the histopath result will showed? d. Definition of dysfunctional uterine bleeding. e. What other investigation want to do? (transabdominal U/S) f. what's the coverage of abdominal U/S? what U/S that show the uterus concisely? (not transvaginal U/S & not pelvic U/S. dunno what ans prof want) f. name 3 medications that can stop the bleeding in menorrhagia & how it function. II. Asthma Q's: a. GINA guideline 2006 b. complication of asthma. if PC with SOB & chest pain + reduced breath sound, what diagnosis? (pneumothorax) b. A&E setting: acute asthmatic attack, what you wanna do & medication want to give? type of respiratory failure. oxygen therapy in type 2 respi. failure c. ward setting: how you monitor the progression of pt. (RR, PR, BP, PEF, SpO2, respi exam for wheeze & accesory m. usage) d. Klinic kesihatan setting: what u want to do during follow up of pt. (compliance, inhaler technique, optimize medication, prophylaxis) e. the latest asthma medication in Google?? last Tuesday Report
Ayu Anastacia pe: was asked to show thyroid examination Q: patient on Zeldox. what is Zeldox and why on zeldox eventhough no psychotic features what is long term goal of the patient how to manage brother had ADHD. any relation btween of MDD and ADHD. patient went to daycare..what is the activity at daycare? patient had fine tremor..why? last Tuesday Report
Cherry Tee 1. lecturers: Prof. A.V.Chin(geriatric), Prof Fatimah Harun (Peads), external (gynae) 2. Specialty: medicine 3. chief complaint: headache for 3 days 4. brief history: 49/I/female, headache a/w vomiting, dizziness, blurring of vision, h/o Rheumatic Heart Disease at 21 y/o and had metallic valve replacement at 23 y/o. poast op on warfarin 4-5mg and INR maintained at 1.9-2.3. 5. PE finding: bruises over both arm craniotomy scar over right temporal region sternotomy scar metallic click tachypoea irregularly irregular weak pulse, normal rate increased JVP displaced apex beat Patient said got AR and MS Bibasal crep Ascites Hepatomegaly with liver span 12cm Sacral and bilateral LL oedema 6. diagnosis: intracranial haemorrhage secondary to over warfarinization 7. questions asked by lecturer (mainly conducted by Prof Chin What other drug can be used other than warfarin? Heparin and fondaparinux Differential dx Symptom of increased ICP? Headache, vomiting,dizziness, blurring vision Earliest sign of increase ICP? Cushing reflex (papilloedema is a late sign) Is the patient had heart failure? Yes evidenced by above sx What are the indication of warfarin in this patient? Prosthetic heart valve and AF What level of INR should be maintained in patient with prosthetic heart valve replacement? 3-4 What other prosthetic heart valve available? Bioprostheses valve Interpret CT scan. Subdural haemorrhage with midline shift bell rang: external examiner ask: " how you confirm this CT scan is your patient's?" is writen there.. last Tuesday Report
MBBS(Malaya) 06/11 Final Exam Data Store Ng Boon Keat 1. lecturers who took u UK external gynae (dr Anna Mary Lensden??) Prof Ong(surgery), Prof Zuraini(PCM) 2. specialty Gynae (UK external main examiner), Prof Ong only said (come in, and forever silent), Prof Zuraini(hi, and forever silent) 3. chief complaint Post menopausal pervaginal bleeding x 6 months. 4. brief history -P5 + 1(self abortion) -PV bleeding since 6 months ago, investigated in teluk intan 3 months ago, biopsy came back with the result of cervical CA... -history same as Wang Jie... except: -10-14 years of IHD with 2 PCI done, 10 years and 7 years ago. -Hpt 10-14 years. -partial compliance on ACS treatment -last f/u in IJN 3 months ago -husband died only 3-4 years ago wo... she said. -only risk factor for cervical CA is grandmultipara. 5. PE finding -sweat!!!! find nothing :-P except high BP, anaemia, and minimal wasting(which i forced to agree) -no mass palpable... omg... -kiv got liver enlargement 6. diagnosis Cervical CA... she want my provisional to be endometrial CA first before cervical CA. 7. questions asked by lecturer History: 1. Is there HPV vaccination during the era of patient? (i answer only recent years, not more than 20 years... she laugh, hahaha only these 3-4 years they really stress on vaccination... i said ok, sorry >.<) PE: 1. Show me the sign of physical examination: striae, anaemia, and tenderness(right iliac fossa to right flank tenderness.)
2. Demonstrate how you examine liver: eh, palpable liver to 3 fingers breath??? Swt at this moment... thinking mati lah.... but she did not drill... so, haha :-) 3. still no palpable mass wo... i think it is a pubic tubercle izzit?? dun noe... need to discuss with wang jie later or go to the ward to ask the patient. Mx: 1. How would you manage?(she really want things in systematic order... so... haha, i answer everything haphazardly and she appeared not very impressed, so the final answer is history, pe(abd), VE(speculum, then only Bimanual), then pap-smear, then colpo, then ultrasound, pipile, then only biopsy (==" swt) but i manage to answer all. ) 2. Do you know about the stage of disease? (i said i am not sure) 3. Do you patient know about her stage? (i said patient not know, apparently hmmm... the patient DID know about the diagnosis... should answer: it is unreliable from the mouth of the patient, especially if she is not so educated) 4. She said stage 2, what does stage 2 means ?( with prompting, get the answer correctly. ) 5. She want definitive management.( i answer TABHSO) 6. She ask TAHBSO got chop chop cervix bo? ( matilah... i dun know...) 7. She said what do you think? ( i answer radical hysterecromy... apparently the answer is Radical hysterectomy with clearance of lymph nodes... gg) 8. What is other mode of therapy aside from surgery? (i answer radiotherapy, yessss... everybody happy :-)) 9. What so bad about surgery on uterus and vagina?( i answer bladder injury and rectum injury.) 9. What is the complication of radiotherapy? i said cystitis(prof ong nodding head) 10. Since you mention about paliative... tell me how do you want to palliate the patient?? (i dun noe how to answer, and answer alot of cow shit and bull shit... so the moral lesson izzz: dun dig your own grave. The question asked really depend on what you said...) Ok, that's me :-) i guess i pass, not with flying colours, but at least i know i didnt die. last Tuesday Report
Siew Li 1. lecturers who took u ( Prof Mary , external, Dr Nuguelis ) 2. specialty ( paediatrics) 3. chief complaint- 23 months old Malay boy, diagnosed bronchial asthma 1 month + ago, currently asymptomatic, on Ventolin and Flixotide 4. brief history 23 months old Malay boy, initially presented with runny nose, cough and post tussive vomiting( green sputum), no fever for 1 week, a/w wheezing. Family member no URTI sx, no hx of foreign body ingestion, no fever. Turns blue during attach, increased rate of breathing, with intercostal recession, still can say mama, worst during morning and nightime. No personal atopy history. Uncle on paternal side had asthma. Both parent and only sister dun have. started on Ventolin and Flixotide, 2nd attack on 3 weeks ago. Same presentation. 5. PE finding - no respiratory distress: nasal flaring, looks pink, 100bpm, 24breaths/min - growth : wt btw 25 - 50th centiles, height 3rd centile - no eczema over NECK, FLEXOR - chest: increased AP diameter, hyperinflated lung, harrison's sulcus, hepatomegaly 2 FB. 6. diagnosis- poorly controlled asthma 7. questions asked by lecturer 1) what is the occupation of the father? ( sorry prof, i forgot to ask)...:( 2) what is the importance of the type of transportation particularly in this patient? ( during exacerbation, how fast can be sent to hospital?) 3) PE: - show me signs of respiratory distress, any growth failure( show growth chart), do chest examination, what is harrison sulcus? where to look for eczema in this patient? 4) how to u convince that he had asthma in the first presentation? 5) what test u want to do?( FBC, RFT, CXR) what r u looking for in CXR?( she wants foreign body). How the CXR looks like if there is foreign body? 6) how to manage chronic asthma?( patient education, father quit smoking, asthma action plan, wash bed sheet avoid dust mite, avoid precipitating factors) 7) let say patient only on Ventolin, what would u do in his follow up in clinic?( any indications of prophylaxis?) 8) if patient's mother said that she had learnt from internet that steroid has side effect, how would u tell the mother? what r the side effects of systemic steroids? 9) if patient came in with acute exacerbation, how would u assess the severity of the patient? That's all i think! All the best...... last Tuesday Report
TarMizi Yusoff From: Nurul RCMP 1. lecturers who took u- Prof Razif, Prof David Choon, Prof Sanjiv (observe most of time) 2. specialty-(Lovely?)Ortho 3. chief complaint-Numbness n weakness of arm n forearm 4. brief history- Apparently well until 7/12 ago post MVA motorcycle vs car, sustained a laceration at the left neck injury (by glass). N wound laceration on the head n hx of LOC n post traumatic amnesia? Since then she experienced numbness n weakness of arm n forearm. F/up in UMMC n Schedule for op next month.I messed up my hx, dunno what to ask more.So, please be prepare for BPI..huhu. 5. PE finding-Just show positive findings systematically..gulp... A lot of findings lorr.. Well-healed scar over the left lateral of the neck Deltoid muscle wasting, winging scapula, adduction,pronation and internal rotation of left arm with waiter's tip appearance? I was confused with Erb's n Klumpke's palsy..adoii What is the obstetric BPI- It's Erb's Palsy.ok...huhu Dryness of the skin of left arm with thenar n hypothenar muscle wasting Hypotonia Power of shoulder 0/5 Power of the elbow extension(C7) 2/5, elbow flexion(C5,C6) 0/5 Wrist flexion(C8) and wrist extension(C7) 5/5 Fingers flexion, extension, adduction and abduction(C8,T1) 5/5 Loss sensation over C5, reduced sensation over C6 and T1 Reflex-Normal but i think there is left reverse supinator? Tenderness over the sterniclavicular joint and supraspinatous area I didnt check the neck ROM n lower limb which i should.huhu=( No horner's syndrome I also check for cervical myelopathy sign as my DD I was wasting my time with taking the vitals which not significant at all? 6. diagnosis-BPI 7. questions asked by lecturer-What is your different dx- I give BPI.What is your other differential diagnosis? Cervical myelopathy (dt trauma?)? I said i think the patient is having upper nerve root injury?involvement of C5, C6 n T1? What is horner syndrome? How to check dryness of skin-anhydrosis?
Do u think the patient got sympathetic involvement?Yes? Stages of nerve injury?neuropraxia,axonotemesis,neurotemesis. Which one can recover? Do u think the patient will recover?No? Other than physiotx wat the patient can do? What is cervical myelopathy sign do u know of? Hoffman, 10 secs test, Reverse supinator, Lhermitte's, Finger escape. The patient can pass urine by herself?Yes U should examine the LL then...yes i know.. Ix-Nerve Conduction study.Can nerve conduction study detect wat is the prob.Yes. MRI-to see pseudomeningomyelocele?this is what i said..haha supposedly pseudomeningocele...What other thing to look for?spinal compression?Nerve root involvement-radiculopathy? I merapik2 dah waktu ni rase nak nangis.. Mx- how to determine when to do surgery?Give time for healing 6 months? Do nerve repair n transfer... I did my best with my obvious shaking hand.haha.Goodluck. last Tuesday Report Wen Mangteen ecturers who took u ( Prof Ong, Prof.Zuraini, UK external examiner) 2. specialty ( surgery) 3. chief complaint-65 year old, chinese geltleman. painless gross hematuria 4. brief history presented 8 years ago with painless gross hematuria, serial ix show bladder CA, neoadjuvant radiotherapy, surgery, adjuvant chemotherapy........ well until 1 yr later, recurrence. 5 yrs later hv ?pelvic abscess, I+D done then experience intermittent right hip pain...... admitted this time bcz gross hematuria, painless. 5. PE finding -pale, nt cachexic, on CBD, left nephrostomy tube... hematuria. abdomen, midline laparaotmy scar, laparoscopic scar, right iliac fossa scar( for I+D), no hernia. no abdomen findings..... 6. diagnosis- recurrence bladder carcinoma 7. questions asked by lecturer 1) what is the differential dx? recurrence, trauma, stone, UTI, prostate CA, BPH......... 2) what is the IX? 3) lets say is unilateral hypronephrosis, where will be the level of obstruction? 4) contrast or non-contrast CT? 5) show me the antegrade pyelogram and ask wat is this. wat u see, why? 6) wat will you do if u see a growth in bladder during cystoscopy? 7) wat will you do to make pt feel better? i think is all i can remember...... good luck
last Tuesday Report
Ka Kiat Chin 1. lecturers prof Sajar (PCM), prof Lucy (Paeds), prof Mary (external) 2. PCM 3. Chief complaint came for exam 4. History 44/m/gentleman, dx with epilepsy for 14 years. no previous admission in ppum, follow in ruka. last attack on oct 2010 due to stop taking drug for a week. GTC during sleeping, on phenytoin no complications. no other medical illness. still driving 5. PE no finding. asked to show the signs of focal lesion (increased ICP) : papiloedema, unequal pupils, visual field (HH and bitemporal hemianopia), diplopia (LR6). Phenytoin SE: signs of anaemia, gum hypertrophy. bp 140/100 6. diagnosis - epilepsy 7. questions: wat psychological illness associated with chronic disease? investigations when patient follow up in clinic long term management? advice to family members when seizures happen? advice on smoking? (prof lucy) driving issues? will u diagnose him hpt on single reading? last Tuesday Report
Ong Yen-Yeung 1)Lecturer: Prof CT Lim, A/P Sofiah, Prof Azad 2)Specialty : Paediatrics loalways....as predicted...haiz 3) Brief history:20y/o Malay "gentleman"(he looks like 10-12 only), known case of Beta thalassaemia major diagnosed 19 years ago, on monthly transfusion, S/c desferrioxamine,no active chief complaint.Strong family history of B-thal.
Was diagnosed when he presented with pallor,lethargy(no jaundice) during 7 months old.Hospitalized 5 days, transfused. Last trasfused 2 weeks ago. Pre-transfused HB:5g/dL.Post-trasfused level: don't know. Each time transfused 3-4 Pack red cell... Currently a bit of lethargy. But no other symptoms of anaemia. Not compliance to s/c desferrioxamine.Why?Lazy. Financial problem.Not experiencing any side effects. Serum ferritin level??last visit was told HIGH but doesn't know the value. Last ECHO and ECG:according to him normal. Infectiive screening negative.LFT, TFT, LH&FSH all donno. No biopsy done before. No changes of voices yet. Noticed himself shorter than his peer. No hypothyroid symptoms.No signs of cardiac failure. Not on vitamin C! Offered splenectomy due to increasing tranfusion but defaulted many years ago due to financial constraint... Family HX: both FAMA are carriers.Father DM,HPT. Eldest sister also B-thal major requiring monthly transfusion,on s/c desf. Youngest brother carrier. Social: Not working,not studying(said due to illness). Below average student. Failed all his SPM subjects.Hobbies: amazingly stilll can play sepak takraw, football post transfusion.stayed at PJ.Come with Bus. Mother is the only breadwinner. Father not working(ill).smokes 2 stick/day. no high risk behaviour. 4)PE:look darker, no frontal bossing, maxillary prominent. short stature: height: 146cm corresponding to 50% of 12 year old....(Prof CT Lim expect me to plot on growth chart leh...even though he is 20 years old!so plot on 18 y/o and extrapolate la...)below 3rd centile! palmar pallor, scleral jaundice, conjunctiva pallor, tongue also pale. Hepatomegaly(13.5cm=7-8FB)...(show how to measure: tell all the 5 stars of liver:size, tenderness, pulsatility, consistency-firm, surface, border) Here i did a stupid mistake:what i thought was spleen was actually the left lobe of liver...DIE... His spleen was pushed to the very lateral site...+splenomegaly... I checked the s/c injection site at the right tigh but forget to present Tanner staging: P0 no pubic hair at all,G0..balls not big gua. Fasting plasma glucose:4.7mmol/L. Urine:dark-colourred, a bit reddish...small volume... Here I did the urine dipstick...(very kelam kabut without wearing gloves...and did not manage to present but able to describe the urine la) 5)Diagnosis: beta-thalassaemia major, complicated with hypopituitarism(?) with non-compliancy to s/c desf.
6)Goreng time -What do you think about the complexion of patient(darker lo)what is it called?start with "H"(haemachromatosis?not sure) -Why did the patient do ECHO? -Patient's pre-transfusion level: 5g/L, are u happy with that? -So what is the normal pre-transfusion level that we want... -What is hypertransfusion and what is the level....Why hypertransfuse the patient? -If he is presented to you when he was 7 months old, how do you diagnose? FBC-anaemia, hypochrom microcytic anaemia PBF-look for what.. what is the differential diagnosis pertaining to this kind of picture? -Do you know how to differentiate it?(yeah...MCV/RBC...dont know what name, but the cut off point is 15) no need to calculate la... -what else-i said ady serum electrophoresis but he want: HB electrophoresis -Look for what? -what else:baseline serum iron, ferritin, LFT.... RING RING~~
last Tuesday Report
Yeo Siang Yew 1. lecturers who took u: Prof wan arrifin, Prof saw aik, external-dr chann 2. specialty- paeds... 3. chief complaint: 3 years old malay girl was admitted due to unresolved nephrotic sysdrome since last week.. (second admission) 4. brief history : Problem 1: 1st admission- noted to have facial puffiness and periobital swelling progressively worsening, and more severe in the morning. no history of URTI, urnation and bowel openings were normal. admited to ward for management and discharged two weeks later. after 2nd admission: after 1 week post discharge, noted still having ascites and was referred from paediatric clinic. first day of admision, urine dipstick still Trace, but O trace on 2nd day of admission. Currently, the swelling was resolved, no periobital, abdomen and ankle swelling. No SOB. Problems 2: Missed 18th months' vaccine, DPT, Polio. 5. PE finding: no significant findings. NO SWELLING!!!Lung clear, cvs normal, no organomegaly, no ascites.
6. diagnosis: Steroid sensitive NS currently on remission 7. questions asked by lecturer 1. Miss immunisation, how will you do? 2. How many type of vaccine?in this case, will you gv now? (hint: immunesuppressed due to NS or on Steroid) - live, attenuated, died 3.other differentials in a child with swelling? 4. Pathophysiology of swelling - from anatomical parts to ascites!! 5. what are the structures involve in leaking? 6. criteria for NS, value, - as he asked other test that you want do in this patient 7. Steroid complications,signs, symptoms in this child which can happend 8. bed side urine dipstick result 9. what is the status of this child now? 10. course of NS last Tuesday Report
Jas Jamaludin got the same pt as Hooi Min~ 1. lecturers who took u : Prof Saw Aik (ortho), Prof Wan Arrifin (pead), external examiner 2. specialty: sport ortho(pt come for exam purposes) 3. chief complaint: right knee pain 1 year 4. brief history: 24/m/man, injured of right knee when playing football.same like Hooi Min + lots of social history !! impaired his daily activity, lots of MC & emergency leave~ 5. PE finding full knee examination + demonstrate extension lag.. 6. diagnosis right ACL and meniscus tear 7. questions asked by lecture almost the same like Hooi Min ~ + describe OA changes in Xray and patient possible xray finding. + definition & causes of giving way~ + last questn b4 bells ring, what are u going to do next?? he wanted to hear ACL reconstruction surgery.. gud luck !! last Tuesday Report
Rosdi Pon Please present your long case following this format. 1. lecturers who took u Prof thambi, prof philip phoi, prof nik sherina 2. specialty surgery 3. chief complaint currently no active complaint 4. brief history 62 y/o chinese gentleman, with history of colorectal carcinoma diagnosed on 2006. first p/w bloatedness and fresh pr bleed. non smoker occasional drinker no fhx of crc 5. PE finding a lot of scar. got i chemopot. midline scar appendicectomy scar, scar from previous stoma, scar from previous hernia examination 6. diagnosis colorectal carcinoma (sigmoid ca) 7. questions asked by lecturer how to check for ascites? staging for crc? where commonly metastases? how? screening for other family members? follow up what to look for? metachronous tumour, is it common? last Tuesday Report
Bebola Ketam 1. lecturers who took u : Prof Azlina (ortho), Prof Cheah ( External pead), Prof KJ Goh 2. specialty: ortho 3. chief complaint: left proximal large swelling of forearm 4. brief history: 53/m/man, presented with 4/12 hx of progressive swelling,
occupational affect and constituitional sx. 5. PE finding examination of the swelling, differentiate where the swelling could be 6.differential diagnosis: list all cause and discuss how to differentiate them: benign, malignant, bone,muscle, soft tissue, joint, infection. 7. questions asked by lecture questio pertaining to exlude secondary mets of other cancer, investigation, what biopsy,interpret XRAY, tingtong. thats all i had. final diagnosis could be sarcoma; on xray it does not involve bone or joint. i felt like being question by 2 ortho examiner, prof Cheah loves to asked question regardless of case specialty. last Tuesday Report
MBBS(Malaya) 06/11 Final Exam Data Store Please present your long case following this format. 1. lecturers who took u: Prof CK Liam [coordinator], Prof Jessie [sweet], Prof Soffiyah [smile always] and Dr. External 2. specialty - Medical [Respi, ID, Neuro] 3. chief complaint - Fever for 2 weeks and numbness / weakness left both limbs. Hx of Hpt, IHD and chronic smoker. [arghhh... not reach any Ix or Mx] 4. brief history Fever - 2 weeks: high grade, progressive n constant, not relieved by pcm. Numbness/weakness - 40 minits, drenching of sweat, slured speech. Multiple probs with IHD, TIA.. Discharge well for 2 days and coming back due to progressive fever. 5. PE finding - UMNL [hypereflexia and hypertonia], elicit d reflex... Bilateral coarse crepitation with normal vocal resonance and vocal fremitus. There was maculopapular rash seen due to allergic to antibiotics. 6. diagnosis - Transient Ischaemic Attack - Drug Rashes - Pneumonia with PUO 7. questions asked by lecturer... - Infective endocarditis: presentation and how to diagnose? - Acute Coronary Syndrome: PTCA [asked during Past Medical Hx]
- Elicit hyperreflexia - Classified the rashes, differential of rashes with pruritus. - PUO: causes... Arghhh... not reach investigation... stuck in history of PUO and PE of rashes... arghhhh.... - MHR last Tuesday Report
Ngui Ling Xiu 1. lecturers who took u: prof nik sherina, prof philip, prof (i guess fr surgery dept coz always saw him walking around surgery dept, indian guy, thin tall, curly hair, middle age, dunno who) 2. specialty: PCM 3. chief complaint: recruited for exam by mohazmi 4. brief history: uncontrolled DM, HPT, hyperlipidaemia, BPH. Polio at age of 5, complication OKU, present all then summarize, they are quite patient i think. 5. PE finding: Bedside examination of UL inspection, right side, wasting of thenar muscle, foream muscle wasting, median nerve affected, examine ulnar and radial normal. Then examine UL motor, patient compensated the elbow extension by shoulder pushing forward. Then lower limb inspection, wasting of left lower limb, objective measuring the circumference, then check the vibration ( prof philip ask how to check if patient REALLY feel the vibration??? coz u touch the pt oso noe, but he said i m not saying that the patient will tell lies, later ans will be comparing with chest, the ques sounds interesting but answer he want weird). Fundoscopy silver wiring, pt eyes dilated to pupil size 9mm. Others bedside examination i do urine examination all they did not ask. 6. diagnosis: explain about the findings, poliomyelitis, ant horn cell then lower motor neuron 7. questions asked by lecturer Ask about investigation.... reason Then ask about some issues like lisinopril caution b4 giving, renal artery stenosis, rule out u/s, renal bruits. Management if patient still uncontrolled DM, how to start insulin, prebed, dosage. Pt with family hx of colorectal ca, pt came what will you tell him, later prof ask how to screen him easily, fecal occult blood. The side effect of the drugs, metformin, gliclazide, lisinopril. Last ques if pt cannot tolerate lisinopril, present with cough, what will you do, change ACE to ARB, then prof philip ask what is ARB??? suddenly thought block, then all of them hinting, the surgery prof who was silent for whole day suddenly so excited n hinting also. Finally, bell rang and oh i remember, angiotensin receptor blocker, haha... I heard prof sherina said to prof philip ya, we all experience this
too, haha. She was so kind;)Thanks GOD for giving me health, cooperative patient, and nice examiners! last Tuesday Report
Ct Gan 1. lecturers who took u-Dr F....(O&G, external), Prof Pan (Ortho, external), Prof MTKoh (Paeds) 2. specialty-O&G 3. chief complaint-for exam purpose 4. brief history -34/M/G4P3, at 18 weeks POG, completely well throughout the pregnancy, come for exam. 1st pregnancy: gastroschisis, left leg auto-amputated, emergency LSCS. next 2 children SVD at term at UMMC.otherwise normal, no family history of anomaly. amniocentesis done during 1st pregnancy: normal. 5. PE finding-gravid uterus + centrally located pelvic mass 6. diagnosis-fibroid in pregnancy 7. questions asked by lecturer-why refer to tertiary centre for delivery of 2nd & 3rd children? (previous anomaly, previous scar) PE: do an abdominal examination discuss abt PPH (def, classification,...) if let say pt got cervical laceration, what wil b ur acute Mx? last Tuesday Report
Cheng Joo Qing 1 prof raman(paeds surgery), prof khoo( PCM), prof mary ann(external) 2 surgery 3 left facial swelling 4 left facial swelling, increasing in size, multiple negative biopseis..CT abdomen, found renal mass, for nephrectomy 2morow 5 left facial swelling,10X8cm, nonmobile, smooth surface, firm..no LN, no other positive findings 6 RCC wit mandible mets?( examiner lead me to dis dx, at first i said LN, pf raman asked: do u think LN will be so large???) 7 where does RCC mets chemotherapy for RCC, trial in UMMC-i dunno tx for this pt-radical nephrec, chemo for lung mets, radiotherapy for bone mets tumor marker for RCC-i dunno, pf raman ask do u think troponin will be high, i said yes interpret CT scan
frm prof mary: prognosis for dis patient frm prof khoo:wat did hospice do last Tuesday Report
Huang Bao Xian 1. lecturers who took u- Prof Wan Ariffin, Prof Kamarulzaman, Ext (Respi), all of them are very gentleman! 2. specialty-Paeds 3. chief complaint- fever, cough, SOB and noisy breathing 4. brief history- elaboration on chief complaint, patient also had CTEV, prolonged NNJ 5. PE finding- hyperinflated chest, prolonged exp phase, rhonchi, fine insp crep... 6. diagnosis- Acute bronchiolitis 7. questions asked by lecturer - what do u think is the cause of the prolonged NNJ? - what is ur provisional diagnosis? - ur diffrential? why u think is not asthma? - tell me sth abt CTEV? -why patient had to change cast regularly? - what is the grade of CTEV? - what is the operation about? - how do u differentiate a pathological liver from liver ptosis? - common places for eczema. - what investigation u would like to do? - do u think u will do these investigations? - what u can see in CXR? - what u will see in renal profile? what is SIADH? - what is the prognosis of pt? - what u will tell the parents if u said the prognosis is good? - what vaccine? - what is the most common aetilogical factor? - when is the common season? - other aetiological agent? - among all these agents, which one cause most morbidity to patient? - how type 1 repiratory failure become type 2? - how u manage type 2 RF? - what is the site u take ABG? last Tuesday Report
Kevin Ng Rong Xiang Prof Nortina and 2 external Medicine Lupus nephritis No chief complaint history started 1989 and presented with multiple joint pain and body swelling got 10 relapses, every relapse must ask very detail and they will ask one by one and ask about your opinion for each relapse and you cannot skip the relapse history. need detail investigation too. PE: moon face and bilateral leg edema Diag: not asked Question: opinion abt every relapse like what do you think this relapse is? what is the triggering factor? what is nephrotic syndrome? should renal biosy done? can patient pregnant? why not? advice for patient? steroid issue like complications? actually all questions very patchy and no proper answering due to time constraint. after i present history already 20minutes cos long history. no physical examination, no investigation, no management, no nothing.
last Tuesday Report
Lee Chui Yee 1. lecturers who took u - prof choy lang(med), prof kamarul(ortho), prof wan arrifin(paed) 2. specialty-medicine 3. chief complaint-scleroderma and eisenmenger's syndrome 4. brief history -scleroderma x 30years -lung fibrosis on LTOT -Raynaud's phenomenon -skin rash -renal impairment -esophageal dysmotility -vsd with eisenmenger's syndrome
-hpt -allergy to chicken, prawn and cyclophosphamide 5. PE finding -everything abt scleroderma - grade 4 murmur at LSE 6. diagnosis: eisenmenger, pulm hpt, scleroderma 7. questions asked by lecturer -wat is the complication of LTOT? -wat is viagra? how does it work? wat is the 2nd mediator? -wat r the other treatment of pulmonary hpt? -in vsd, if pt hav loud S2, wat does it mean? eisenmenger same case with Miss Karti... last Tuesday Report
Shyful Nizam 1. lect : prof MTK, prof pan, prof XXX 2. specialty onco orthopedic 3. c/o: right knee swelling 6 moths. 4. summary: mr xXx/ 55/ gentlemen / presented with progressively increase in size of distal knee associated with pain and numbness. 5.o/e: there was a swelling at the site lateral and proximal aspect of leg, with size 7x7 cm , round in shape, and erythema skin noted over the swelling. on further inspection, there was distended vein over the dorsal aspect of the right foot and associated pitting oedema and shiny skin on the right leg up to the knee level. on palpation : non tender and warm. firm in consistency, smooth in surface, ill define margin and non mobile. otherwise there ware no fluctuation, translucency. on knee examination: reduce range of motion, from 0-60 degree. reduce sensation over the lump. 6 . my impression: malignant bony tumor. eg most likely chondrosarcoma, bcos older age. and osteosarcoma in children. 7.question: - from the history what did u think, malignant or benign. bone or tumor? -which one come first pain or swelling, what is the significant?
- does his problem effect his work? what he think about his problem. how does he cope the situation or the problem? -describe the swelling? -why there is erythema over the swelling? - what is the diff redness in malignant and acute infection? -what example of bone infection and what is there clinical feature? -what is the diff between osteomylaitis and malignant bone tumor? - what structure may involve- common paroneal nerve. -what is the clinical feature of common paroneal nerve palsy? -can u demonstrate common peroneal nerve palsy? -which one is significant dorsiflexion of ankle of plantarflexion? why? -what other system do u want to look, why? - how can lession in bone met to lung? -where is the lymphatic drainage from the swelling spread to? - from all the finding what is u diagnosis? - describe the xray- well define hypodense lesion over the fibula, osteolytic, thining of the bone, proximal bone expansion, and pathological fracture. -from the xray, malignant or benign? - what further investigation? - management? teeeettttt.....tq last Tuesday Report
Ikha Zulaikha specialty: medicine (b-thal) lecturer: prof wan azman, prof aisyah, prof eugene. chief complaint: nil HOPI: -22/m/male dx B-thal major since 2 yrs old. receive blood transfusion every months. no transfusion complication. pre hb is usually 7-8. post hb 13-14g/dl. every months will have have anaemic symptom such as reduced effort tolerance and SOB 2-3 days before go for the next blood trasfusion. have one allergic reaction post-transfusion when he was 12 years old. -family hx of consaginous marriage and father+mother both are carrier (only know their status after he was dx to have b-thal). All sibling were screened. 2nd brother also carrier. youngest brother affected. -take iron chelating agent: desferioxamine (10 hours, 4-5 times per week, 4 bottle per day) since 10 y/o and desferiopone (7 tablets per day)since last yr. no complication of iron chelating agent. he was compliant to the treatment. -complication from iron overload- poor growth - hypogonadism (small testis, penis, no axillary hair, sparse pubic hair): receive IM testosterone monthly - hypothyroidism: no symptom, accidentally dx during
routine follow up and check the hormone level. on thyroxine. Lastly, social history: was feeling inferior toward friends coz shorter, no moustache or beard. feel burden towards family, not perform well in academic. never get teased by friend. smoking, no alcohol.prof really particular bout it. -got teased by friend? friend know or not? wat is his feeling? wat is his family feeling. p/e -check abdomen. he has splenomegaly. prof ask how to differentiate spleen and kidney? enlarged inferomedially, cannot get upper border, not ballotable, moves with reps, got splenic notch and splenic rub on auscultation. -prof asked bout testis and penis and pubic and axillary hair. patient had no axillary hair, sparse pubic hair, small testis and short penis length. -how to check for pallor? conjunctiva. -comment on the face- thalasemic facies: maxillary hyperplasia, frontal bossing, gum hypertrophy. question: 1)sign and symptom of hypothyroid- constipation, cold dry hand, slowness in motion, 2)how to dx hypothyroid: thyroid function test-low T4 and TSH. 3)management of b-thalasemia- i ans: - regular blood transfusion- need to take pre and post hb level, ensure received the correct leucodepleted blood, monitor the patient during transfusion if got any complication, give lasix afraid of volume overload. - iron chelating agent when serum ferritin >1000 and monitor the complication. types of chelating agent- DFP, DFX -need to monitor complication of iron overload. then prof ask how to monitor: LH,FSH and testosteron level for hypogonadism, TFT for hypothyroidism, FBS or OGTT for DM, echo for cardiomypathy, liver fuction test for liver cirrhosis. and monitor growth for effect of low growth hormone. -splenectomy if patient has hyperslpenism. then prof ask, how to know? i ans splenomegaly and thrombocytopenia. as well as low Hb.. actually 3 cell line will be low. -discuss the percentage of his offspring can get thal. then, prof gives a scenario : if he get married with normal female, what percentage of affected pregnancy and carrier?? if married with carrier, what is d percentage of affected pregnancy and carrier?- need to calculate using mandelian law. -lastly, prof ask, how do u want to help the patient. do u want to refer to any grup. I ans THALASEMIA CLUB, but all laughed! prof wan said, not club, its THALASEMIA SUPPORT GROUP. then prof ask, how it can help d pt? - pt
can discuss with other thalasemic patient and the group can help him to deal with thalasemia .. prof aisyah Q: wat is the urine look like (pt had a urine sample)? i said tea color urine. but actually not.she prompt me and i ans due to iron overload, iron was passed in d urine. but i still dunno d color of d urine. i heard prof aisyah said red sumting... not sure wat. mayb red-bronze colour due to iron overload.
last Tuesday Report
Chai Jia-Ning 1. lecturers who took u: Prof Chan Lee Lee [Paediatric department], Prof Woo [O&G] and one more forgot already.. XD 2. specialty - Paediatric [Respiratory] 3. chief complaint - 8 year old malay girl. Here for exam. Underlying Bronchial Asthma (BA) 4. brief history Diagnosed at 6 year old during a BA attack. Defaulted follow up and treatment. 6 march 2011, hospital admission due to an acute attack with shortness of breath, lethargy, talking in phrases, fever, cough, vomiting. Discharged with oral prednisolone, MDI ventolin, MDI serotide. + eczema + allergy rhinitis + allergy conjunctivitis No known food or drug allergy. Father smoker, mother BA & allergy to seafood. Brother no atopy. School performance excellent, but not good in sports (shortness of breath, chest tightness) 5. PE finding - growth normal. Vital sign stable. Harrison sulcus, loss of liver dullness. Chest clear. abdominal skin & lower limb + eczema. 6. diagnosis - BA 7. questions asked by lecturer (all by Prof Chan) - Occupation of parents? (sorry I didn't ask) - How do you diagnose BA? (clinically) (Prof nodded) - During her first presentation, how would you come to the diagnosis of BA? (long history of noctunal cough, atopy march, family history of atopy, clinically marked improvement with nebulizer bla bla) - Development milestone, she is 8 year old now, how do you assess? (whether she
did well in school, physically active/ active in sport) (Prof nodded) - What is BA? (reversible obstructive airway disease) - [Bring to bedside] What physical signs you want to look for in this patient with history of 2 years BA? (Growth, harrison sulcus, chest wall deformities, signs of eczema, signs cushing syndrome) - What type of chest wall deformities you would expect in this patient? (Barrel chest because of air trapping) - Clinically how would you know whether there is any air trapping? (percussion, showed examiner. hepatic ptosis) - What causes Harrison sulcus? (chest wall indentation at insertion of diaphragm, due to underlying chronic lung disease) - Why growth is very important in this patient? What would you look for? (stunted growth, as frequent exacerbation will cause poor lung function) (Prof nodded) - [back to room] What investigation would you do during her first attack back in 2009? Reasons. (FBC and CXR, not further more Prof needed. Offered lung function test, she disagreed) - Why a CXR at first attack is important? (to ruled out other conditions that can mimic asthma) - What condition mimics BA at age of 6? (pneumonia. Prof prompted:" other conditions that will give generalized wheezing and shortness of breath") (foreign body, mediastinal mass, bilateral lyphadenopathy that compressed on air way) - Where will the foreign body usuallty lodge? at what level? (bronchus, at right anatomy as right bronchus is more vertical compared to left.) - After acute management, how would you manage this patient? Who should be started on preventive treatment? - How do you assess the severity of attack? - How do you assess control of disease? (answer of last 3 questions can be found in GINA guidelines, so dry) last Tuesday Report
Heah Sooches Please present your long case following this format. 1. lecturers who took u: MT Koh (paed), Prof Pan (ortho)-external and Prof Singh(o and G)-External: 2. Specialty: Alreally mention 3. chief complaint: Coming for Routine f/U at Paed clinic 4. brief history : 14 yo Chinese boy with the history of type 1 Dm. HE was apparently well until 2 years ago he presented with polyuria, polydipsia ,polyphagia, nocturia and lethargy. He had a good control of his DM. Never admit due to hypoglycaemia attack..Actually, he had no much of problems and no complications. His is a GOOD HISTORIAN and he had come for exam b4.. Ur history muz had a complete with the How he was diagnose, where and
when..Advice given by dr...Medication he took(INSULIN) muz mention everything who inject, when and where he inject, compliance..any complication d2 to the dz.. Social history vry imp..Muz hv( His teacher and student noe about?? And muz ask travel history) 5. PE finding..No much..Juz he had lipohypertrophy at the inject site( Bilateral lateral aspect of UL) 6. diagnosis 7. questions asked by lecturer. -other history u need to ask according Hyperphagia? (he want to noe izit the pt put on many weight or not? -Travel history-why imp..(Miss the meal and injection...More imp is how he store the insulin) -PE, what u want to check..(Height, weight, fundoscopy, hepatomegaly, testis, sensation,vibration, hyporeflexia and pulse and dont forget Urine DIpstick) -What u look for by fundoscopy( describe about preproliferative, proliferative and maculopathy) -what the reflex u think he ll get( Hyporeflexia)...Show me how u do test the reflex.. -inteprete the result of urine dipstick - when every time he come to clinic for f/L..What laboratory test u want to do? (FBS, HbA1c..Tell me the level he need to achieve-(I said previously is 6.5% but now bcome 7% dt more of them ll tend to get hypoglycaemia).THANKS to SHAREN coz telling the ans to me B4 that..HAHA -Liver fx test..What liver enzyme u want to look for ( ALT, AST, ALP and 1 more ..i forget liao but prof MT KOH start with G so finally I said GGT) RingSSSSSSSSS..Yeah can relieve liao..prof MT koh like ok saja but i x sure he ll b silet killer again boh..So..Muz pray Hard..Hopefully can PASSSS...hehe Bender Fry Same case with Sairy. 1. lecturers who took u Prof Cheah (Paeds External), Prof KJ Goh (Medicine), Prof Azlina (Ortho) 2. specialty Paeds 3. 17 year old boy (appeared like 10 years old), no chief complaint,well 4. brief history Thin, short and low body weight till now Birth - Failure to thrive without reason being identified, under follow up at private hospital. Born via SVD at term with 2.73kg, no significant perinatal history 3 months old - Pneumonia, 6 days of hospitalization, no complication. 8 years old - Multiple episodes of abdominal pain after eating oily food,
steatorrhoea. Referred to UMMC for sweat test, positive. U/S of abdomen, CXR (scarring), and liver biopsy (liver cirrhosis) done. 9 years old - Dark and foul smelling stools for 2 days. An episode of haematemesis with multiple huge blood clot. Hospitalised for OGDS and rubber banding. 10 years old - Started to have thick yellowish green sputum produced every morning, no fever. 15 years old - Easy bruising and epistaxis. Currently under f/up at UMMC, everyday on Vit. A,D,E,K, Pancreatin (Creon) 17 tabs, nebuliser, chest physio, and acapella. Antibiotic tuning was done annually and oesophageal banding was done once in 2 years. No PMH, PSH, FHx of CF or liver cirrhosis. 5. PE finding (only positive findings) Anthropometric chart - both height and weight are far below 3rd centile General appearance-thin Finger clubbing, leuconychia, absence of moustache, beard, axillary hair,pubic hair Distended abdomen, flat umbilicus, spenomegaly (10cm below costal margin). 6. diagnosis Cystic fibrosis with liver cirrhosis and malabsorption for 9 years 7. questions asked by lecturer (Prof Cheah keeps leading me to the answer he wants, I am like a fish chasing the bait.. T.T) History - what other aspect u shud consider other than academic performance? sport PE - Show me how u do nutritional assessment. Does he look like a 17 year old boy? No,why? Do you plot the growth chart? What do expect his height if he is normal? Back to room - During the follow up, what will you do to assess his condition? By symptoms(steatorrhoea), weight, LFT. - Tell me the features of decompensated liver failure. Do u think he is having decompendated liver failure? No,why? - Why he has oesophageal varices? What other parts of body u can find portosystemic shunts? How will u treat portosystemic shunts? - Other than pancreatic insufficiency and malabsorption in CF, what other features u know? What is bronchiectasis? Tell me how u diagnose. What will you do to investigate? Why u think the sputum is yellowish green? What will u do for the sputum? What organism u expect to discover? Tell me the features of pseudomonas lung infection in CF patient,something like that..I responded it by showing SHOCK expression,zzZZ.. - This treatment is not used in Malaysia, if the bronchiectasis persists, what is the final treatment for the pt? Lung transplantation gua... P/S: I was in denial when getting this patient..but trying hard to get it through..hope examiners will be considerate after seeing my petrified face and stupor. Was damn embarrassed and amusing as I accidentally spoke "plancental
insufficiency" instead of "pancreatic insufficiency",huhu.. Good luck everyone! ^^ last Tuesday Report
Wei Cheng Please present your long case following this format. 1. lecturers who took u 2 external + 1 i dono, same with rongxiang 2. specialty: psy 3. chief complaint: nil, 55 year old, unemployed, known case of psyciatric illness > 30yr 4. brief history: recurrent manic episodes requiring admission, last admission was 2 years ago (but she tol the other malay that was 3 weeks ago...=.=''...i think i screwed up), downward drift 5. PE finding: cogwheel rigidity (i demo using elbow flexion; examiner said wrong...she said correct one should be using wrist...=.='' 6. diagnosis: bipolar/ schizo?. screwed with hx.pt tol all hx abt manic episodes, but she is taking antipsychotic, no psychotic feature elicited excepted for nonbizzare grandiosity..=.='' 7. questions asked by lecturer -insight -dd, y?y bipolar instead of schizo? -management -SE of lithium. therapeautic range -if this is the 1st episode, wat other dd wil u consider? she wan substance (i answered hallucinogen such as ketamine, she wan amphetamine) -PE: - examine for SE of medication (on typical antipsychotic) - how to check for bradykinesia - causes of cogwheel rigidity? wat's the correct method to elicit it? - wat other SE to look for -gv 1 specific SE of atypical antipsychotic
was chase out 5 min b4 bell rang, seriusly bad prognosis....=.= last Tuesday Report
Zahratulhuda Khairulezuan 1. lecturers: Prof Nur Aishah, Prof Chan Lee Lee, Dr. Ho (all the profs and dr are nice =)) 2. speciality: surgery 3. c/o: per rectal bleeding for 1 day 1 year ago 4. HPC: 62 years old indian gentleman. started to have constipation for 1 week. then passed out pencil shaped stool. then did not have bowel opening for 2 days. the subsequent day he had per rectal bleeding. 4 drops of dark red blood. no mucus and no clots. assoc with abdominal discomfort, tenesmus. no LOA, no LOW, no abd pain. he was diagnosed with colorectal Ca after colonoscopy. defunctioning colostomy was done. MRI was also done to stage the dss. it has metastasize to the lung but no lung symptoms. neoaduvant therapy was done to shruken the tumor. he underwent radio, chemo xeloda (chemo pill). then after 5 months abdomino perineal resection was done. he end up with permanent end colostomy. no chemo or radio done after surgery. 2 months after that came back for discharge at anus (anus dah stitch coz APR kan). drain was inserted then OK. family history of colorectal ca. he also had mild depression 5. O/E: No signs at periphery. on abdominal inspection there was midline scar from laparotomy. a transverse scar at right upper quadrant from previous defunctioning colostomy. there was stoma bag at the lower left quadrant. describe the stoma la (there was solid faeces inside so of course colon la). also had incisional hernia at the transverse scar. 6. dx: colorectal carcinoma mets to lungs (duke D) 7. discussion was mostly about colorectal carcinoma and incisional hernia kt patient on bedside la. -show the incisional hernia (suruh patient cough la) -what's important (determine hernia strangulated or not) -how to determine that (they ask to find the neck of the hernia). so ask patient to tense the abdominal muscle by flexing the neck. then ask patient to cough. then rasa the neck. if small neck most likely to strangulate and need to arrange for surgery. tp patient ni wide neck. so no urgent surgery needed. then showed them the anus and say it was healing well since there is healthy granulation tissue and no discharge. then dlm bilik:
-on f/up in clinic what u want to do. find symptoms and signs of recurrent colon ca, complications of surgery. then do CEA to monitor for recurrence. -can patient have normal CEA although have colon ca? ans: can. therefore CEA is not use for diagnosis. it is use to monitor progression and recurrence. -on f/up i will look for depression also -then CLL asked, how you manage the depression i said if severe refer psychiatrist (then diorg laugh la). they asked me to manage. then i said since he has mild depression and he is embarassed to go out, he is wearing cloths kan so org x nampak the stoma bag. then to manage the smell, asked him to clean the stoma bag before going out anywhere. -then tanya staging (duke D coz dh mets to lung) -then prof asked MRI was done in this patient, is it usual? i said no. usually CT thorax, abdomen, pelvis. -so why MRI was done? i ans: MRI is good for soft tissue. it was probably to assess local invasion for eg. to the bladder (they agreed) -what other way to assess local invasion: transrectal ultrasound -how does it help the surgeon: assess depth of invasion and local invasion (i'm not sure this one) -do you think he has familial syndrome that predisposed him for the colorectal ca ans: no coz he got the ca at old age and so did his sister. usually in familial syndrome the age of getting colon ca is younger. -what familial syndrome can predispose to colorectal ca (yg ni ans wrongly...huhu) polyposis synd (FAP and Peutz Jeghers) HNPCC (Lynch syndrome) good luck!~ =)
last Tuesday Report
Chai Pin Ang Chai Pin 1. lecturers who took u Prof Sofiah (O&G), Prof CK Liam(Med), Prof Jesse(Paed) and another observer (O&G i think)
2. specialty: GYnae 3. chief complaint: Anaemic symptoms with menorrhagia and dysmenorrhoea (from ward 10) 4. brief history 47/I/Lady, Para 2, with underlying DM and asthma, present with menorrhagia and dysmenenorrhoea a/w abdominal mass for 1 yr, got typical anaemic symptoms. previous menses was 3-4 days but since one year ago increased to 12-14 days each cycle.10-12 fully soaked pads and a/w blood clots. Dysmenorrhoea confined to lower abdomen and the back, related to menstrual cycle, affect her sleep, relieved by analgesia she was admitted twice last month due to anaemia and was transfused 5-7 units of blood. current admission was scheduled for an operation. No bleeding tendencies or medication taken. 2 uneventful SVD children and no previous operation done. 5. PE finding Vital signs stable. Pallor on the nailbed and conjunctiva. no tachycardia or SOB. INspection: abdominal distended mainly at the lower abdomen, no scars, got linea nigra and stria ALBICANS (was struggling to come out tiz word after hinting by Prof) Palpation: Tenderness. Mass is 27cm frm symphysis pubis, clinically 26 weeks of gravid uterus size. the mass is round, well margin, smooth surface, can get above it. Percussion and auscultation: din manage to present (no abnormal finding) 6. diagnosis: uterine fibroid 7. questions asked by lecturer a. in the room: so wat other medical problems that may cause bleeding in this patient? (bleeding tendencies, hypothyroidism), any medication that can cause bleeding? (anticoagulants.... i cant answer it even the Q was easy) b. Bedside: presence of pallor clinically, so estimated Hb in this patient? c. how to differentiate uterine mass and ovarian mass? (i ans uterine mass centrally located, can get above and prof ask: can get below it or not? i said yes... haiz...) then they ask me to check on patient again, did stupid at that time..Prof Jesse come and guide me to palpate correctly...=.=lll. The answer shd be cant get below in uterine mass, because it connect to cervix.... d. investigations: FBC (Hb low...) Prof Liam: so wat type of anaemia in tis patient? (guess wrong again, everyone is shock again..) should be microcystic hypochromic anemia because tis is chronic blood loss for 1 year. e. next: wat is your expectation of the platelet count? (i dono...) f. other investigations? they wan straight to the point of diagnostic Ix--> ultrasound, endometrial sampling
g. differential diagnosis: uterine fibroid.... (i said TRO CA in the beginning..they don wan tat answer...haiz) h. DEFINITIVE management: hysterectomy last Tuesday Report
Gan Kar Wei 1. lecturers who took u Prof Mary (external), Prof Raman, Prof Khoo 2. specialty Obs 3. chief complaint No 4. brief history 31 y/o G4P2+1, 36 wk+3 days of gestation, 2 previous LSCS K/c/o pregestational diabetes mellitus and currently on insulin treatment admitted into UMMC last week dt poor controlled diabetes No other maternal and fetus complications 5. PE finding singleton pregnancy, longitudinal lie, cephalic presentation.... when i said estimated birth weight, they laughed.. i said probability of macrosomia prof asked hw to assess fetal well being if couldnt appreciate heart sound by using peanut ( ask mother about fetal movement and laptone ) she also asked whether amniotic fluid is high? ( No, fetal part is easily palpable) 7. questions asked by lecturer Hw to monitor this pt? what do u want to look for in ultrasound? 1 more question related to CTG but forgot liao complications a/w LSCS in mother and fetus.. mother- i said poor wound healing, anaesthesia...... she led me to DVT... then hw to prevent DVT fetus- i said TTN then she wanted RDS... what is RDS? Hw LSCS cause RDS? hw to prevent RDS in this pt? prof said why dont delliver at 39 weeks to decrease the risk of RDS wo.. post partum management of this patient... good luck everyone.. last Tuesday Report
Deeyana Mohd Hud Please present your long case following this format. 1. lecturers who took u External examiner ( Caucasian), I forgot the name~main examiner external examiner,
Prof Nortina (neurology) observer 2. specialty Surgery 3. chief complaint 61 year old, malay, single came in with right iliac fossa pain. 4. brief history 8 months ago, she presented with right iliac fossa pain for 1 day, the pain was severe, acute, and colicky. No change in bowel habit and urination. No nausea, vomiting and fever. She experienced loss of appetite and loss of weight 10 kg for the past 6 months. She underwent surgery as she suspected to have acute appendicits and was found out to be perforated right colon cancer ( ascending colon?). She then had Ct scan and PET scan done, and was told the cancer has spread to the liver. She underwent chemo and radiotherapy. A few months ago. she started to experience bilateral lower limb weakness, unable to walk and need to use the wheelchair. No bowel or urinary incontinence. Later, 20 days ago, she experienced with one day history of central abdominal pain, with severe vomiting, passing very hard stool for 1 week. Since that, she was on total parenteral nutrition in the ward. She has family history of colorectal cancer, where her elder sister was diagnosed to have colon cancer at the age of 66 years old. She is single, live alone in 1st floor flat house with no lift. She was able to take care od herself, but sometime she required help from other family members. 5. PE finding cachexic looking with TPN. positive finding was hepatomegaly 8 cm below the right costal margin...i forgot to look for incisional hernia~ 6. diagnosis Examiner didnt ask~Colon cancer mets to liver and (spine?) 7. questions asked by lecturer what the usual presentation of acute appendicitis? pls describe about colicky pain? what type of operation she had?why? right hemicolectomy~ show me on this pic ( he drew the colon) until which part the colon was resected. why patient wears diapers? where the TPN was administered? how u want to manage this patient? he showed me the CT scan- show me the normal finding plus there was multiple liver mets. if there is only single lobe affected what u want to do? the staging of colon cancer- i told Duke's criteria...A, B,C, and D. he said Dukes until C only as it based on histopathalogy, so cant comment on dukes D which is distant mets. can patient allow to go home: he said no. tell me about the prognosis of this patient. if she and her sister had colon cancer at 40 years old, what do u think?- HNPCC, FAP, etc. what the risk factor of colon CA-my answer including ulcerative collitis. when do u think people with UC will have colon ca?- the answer is 20-25 years. what the screening programme available in msia-breast and cervical cancer. any screening programme for colon Ca in msia?
what tool we can use for screening purpose: i answered colonoscopy ( no idea actually),but he told me flexible sigmoidoscopy. how can u decrease the prevelance of colon ca in the public? there were a few question i couldn't remember. I have been asked all the way by the Caucasian external examiner~~he seem to hear about figure and percentage~ the last question was what the psychosocial support in this patient...huhu .he asked me to leave b4 the bell rang..good or bad sign? for the rest of u....gud luck!! last Tuesday Report
Zurah Hamid B thal major adult. prof wan azman, prof aisyah and prof eugene. my case and questions = ikha. plus pathophysiology of heart failure in thal and a case scenario, if patient come in with URTI, how do u manage this patient start with ix. ok guys. Goodluck. last Tuesday Report
Farhana Nur 2 internal examiners (not sure who they are) + 2 external examiners (All of them are nice & tak garang) SLE 38 y/o/C/lady known case of sle for 22 years.no active chief complain.frequent relapses (more than 10 times) with kidney involvement. typical sle symptoms during first presentation.currently on oral pred, azathioprine, omeprazole and calcium supplement.other medication had been given previously include cyclophosphamide (stop becos she plan to conceive at that time, rituximab (costly drug and had experience febrile neutropenia during this episode),iv methylprednisolone).history of failed intrauterine insemination once,currently still has no offspring. she also has complication of steroid toxicity (cuhsingoid appearance,easy bruising,peptic ulcer disease,bilateral cataracts,fungus infection once but resolved already). PE: most signs of cushing syndrome (just mention the positive findings in the room-not being asked to examine the patient..huhu)
Ques asked : 1.How to diagnose SLE.mention all features for SLE 2.Managemnt of sle. what is the drug that normally give to sle patient but not in this patient? hydroxychloroquine. Should we consider giving her this drug?what should we check b4 start her on this drug? liver function test,renal function test, eye examination since this drug can cause central scotoma. 3.Supposely if this patient come with mood symptoms such as mania or depression.What r ur differential diagnosis? cerebral lupus,steroid induce or depression due to long term unresolved disease. 4.What are the approach for proximal myopathy?what are the differential diagnosis other than cushing syndrome. what investigation u wanna do? 5.All side effects of steroid toxicity.....how steroid can cause infection? 6.What is autoimmune disease? 7.discuss about antiphospholipid syndrome and little bit issue of sle in pregnancy. 8.Since this patient also has kidney stone-been asked about type of stone and management of kidney stone) 9. Features and complications of nephrotic syndrome 10.Suddenly caucasian examiner who sleep all the way of presentation wake up and suddenly ask approch of hyperparathyroidism... 11. caucasion examiner: what are the name of radioistope scan of hyperparathyroid gland? sestamibi scan. 12.What r the mneumonic for hypercalcaemia? more or less these are the questions that been asked by examiners.All the best & hopefully all of us will pass this exam~ last Tuesday Report
Arina Anhar 1. lecturers who took u : Prof Hussain (main) Prof David Choon & Prof April 2. specialty : PSY 3. chief complaint : no chief complain came for exam 4. brief history : 54y/o / Malay/ Men, diagnose with schizo ~30 yrs ago at time of diagnosis : auditory hallucination -comanding, delusion only hv thought broadcasting, no negative symptoms, disorganise speech, disorganise behaviour (start to have symptoms in form 5 - drop in school performance) had been admitted only once due to aggressive behaviour currently no active symptoms working in care cafe no DM HPT IHD METABOLIC SYND 5. PE finding MSE - tak pegi bed side pun just present to him
present the general aprreance, speech, mood affect, thought process/content then he ask about thought blockng, word salad, looseness of assoiaciations then he ask about insight 6. diagnosis i say schizophrenia then he ask for differentials then he asked what diagnosis is most likely in pt with this hx, then he change asking if early onset,high achievers ---> he wants bipolar 7. questions asked by lecturer pt hv a bit of wt gain : so he ask why is it important importance of negative symptoms issue on drug compliance -pt not compliance currently on depot injection, change medication 2 times previously prof : "u mention about hx of smoking, did u asses if patient want to quit smoking" how would u manage *bell ring* ok name 1 drug u would give to pt he basically ask more on the hx, he dissect like one by one and he notice which hx yang tertinggal huhuhuuuu~ last Tuesday Report
MBBS(Malaya) 06/11 Final Exam Data Store sheilaizrin 1. lecturers who took u: prof boey (paeds, main examiner), prof chee(cardio medicine), prof mary ann(external O&G) 2. specialty: PAEDIATRICS 3. chief complaint: 2y/o girl. fever and 1 episode of seizure 4. brief history: fever 1 day, seizure 1 time 5 min. other normal. 5. PE finding: normal. DA normal 6. diagnosis: simple febrile seizure 7. questions asked by lecturer: differentials, how would you exclude. bedside: child's asleep so present findings. what would you look for, how to do kernigs and brudzinki's. what would you look for before ensure mother that this is simple febrile fit. back in room: what investigation. take consent for lumbar puncture. what would you look for in lumbar puncture. how would you advise mother for another seizure. management of status epilepticus. last Tuesday Report
Zahidah Zakaria 1.ortho ext examinar, prof ong, prof ida 2.speciality: ortho paed 3.case osteogenesis imperfecta 8 year old malay girl....diagnosed with OI since in utero at 20 weeks POA.. had multiple fracture, multiple operation for intramedullary rod insertion.. electively admitted for intramedullary replacement at left knee... 4. PE explained LL deformity, cubitus varus, blue sclera, translucent teeth 5.question asked: -are u agree with the diagnosis? why do u said it is OI? -how to manage a child who come with multiple fracture - interpret xray - definitive management for IO- intramedullary rod insertion -prognosis i think got some more question, but forgot already...hehe... last Tuesday Report
Aiwoon Goh i get breast lump. 64 year old chinese women. with post thyriodectomy due to goiter, post nephrectomy due to rcc. pe- exam the breast. full set. after that look for sign of metastase, liver, cns,bone pain, pleural effusion,consolidation. and thyroid eye examination. how will u investigate this patient, triple assessment. intepret mammogram. malignancy change-microcalcification. management-if it is malignant, mascetomy. TNM staging. if femur pain, wat u suspect? how u investigate, plan x-ray, bone scan. last Tuesday Report
Lim Chin Hwan 1. lecturers prof Chee (Medicine), prof Mary (external), prof Boey (Paeds) 2. Gyne 3. Chief complaint
came for exam 4. History 49/I/F, divorcee, c/o menorrhagia and dysmenorrhea for 8 years. Details of menorrhagia and dysmenorhea, pressure symptoms, back pain, diagnosed uterine fibroid 5 years back, last yr Pap smear abnormal, arrange for TAHBSO next month. Interesting sexual history and psychiatric history. *promiscuity, more than 10 partners, few episodes of PID, 1 surgery for vulva abscess, deep dyspareunia, PCB etc. *depressed, stop working, hopeless, prev break down, suicidal attempt after divorce then live a messy life, promiscuity then..spend a lot of time exploring each symptoms and PSY history coz i was afraid got PSY lecture, pt like really fullfill somatization, lots of problems, u name it, she got it...haha...PMHx alot also, migraine, HPT, gastritis, multiple admissions also in the past either gyne or medical prob...lot of it din manage to present oso...SHx very interesting oso, but good to explore, examiner like to hear oso...she go pee2 for 10min, OMG, next time dun let ur pt go pee2 after taking history...haha... 5. PE report vitals, BP high, not tachyc bt tachypnea (pt was anxious as I m a guy, she initially refuse to let me clerk, haha..) she was really in pain, not letting me to touch her tummy, even when auscultate lung and heart she oso c/o pain.. but i manage to get tat fibroid like 20 wk size..VE pt refuse..examiner oni ask to show pallor, signs of anemia, demonstrate on abdo examination and wat else to look for in particular to my pt.. 6. diagnosis - Uterine fibroid w suspicious cervical CA, plan for TAHBSO next month. 7. questions: -let say she is 40 y/o come to ur clinic, after hx and PE, u diagnose got fibroid, wat next thing u would do? VE n bimanual -how would u differentiate btw uterine and ovarian mass? act after say PA n VE hw to differentiate, she say u cant actually, it very difficult to differentiate btw d 2.. -then how? TAS and TVS -let say she still want to conceive n dun wan TAHBSO, wat other option? HIFU, UAE, myomectomy which i say out last as i thought she say pt dun wan surgery.. -wat are the complications rate btw all these? sorry i dunno -How would u counsel her b4 TAHBSO? -wat HRT u will give? ERT -again ask TAHBSO Cx rate? oh...i geleng my head n she ans act 10% then she smile to me...ngam2 ring....then they all smile and say u may go out now.. last Tuesday Report
Karen Koey HueyLing
Karen KHL 1. lecturers who took u: prof honey (paeds, main examiner), prof Rokiah Ismail, ?? external specialty: PAEDIATRICS 3. chief complaint: 5 months old, prolonged jaundice from birth 4. brief history: prolonged jaundice, pale stool, tea colored urine, Stage 4 VUR, biliary atresia negative 5. PE finding: Hepatospleenomegaly. 4cm liver, 6cm spleen. DA normal 6. diagnosis: prolonged jaundice secondary to UTI? TORCHES? NEonatal hepatitis 7. questions asked by lecturer: - normal value of bilirubin - differentials - Define TORCHES - What is HIDA? findings in biliary atresia bedside: child's asleep so present findings. abdomen examination. what syndrome present with obstructive jaundice pisture ( I know is Alagille, but don't dare to answer cos forgot the features!) back in room: - what can ultrasound show? - what is findings of liver in biliary atresia then Prof Rokiah's turn. ( Let us back to basic) - What is the histopathology of liver in this case? - cirrhosis? What type of pathology u expect ( she wants MACRO/ MICRO) -what advice will you give to the parents. last Tuesday Report
Mohd Taufiq 1. Lecturers: Prof X (external), Prof Siti (O&G), Prof Yip (Surgery), Dr Zaharuddin 2. Specialty: Medicine 3. Chief Complaint: Productive cough 5 years ago 4. Brief history: 59 y/o Malay lady, housewife, history of childhood asthma, c/o
productive cough, fever, a/w SOB and wheezing. Initially under Hosp Seremban f/up. In 2007, went to private hosp, investigations were done n diagnosis was made.. condition remain stable however in 2009 another exacerbation occur, went to UMMC, CT scan n CXR was performed and diagnosis was given. Since then she is under UMMC f/up every 4 months. Last year, she had 4 admissions to hosptal due to exacerbation. This time, came in for cyclical antibiotic.. PM hx- dyslipidaemia Drug hx-MDI Ventrolin and Seretide, statin n a/b 5. PE finding: Pf. X notice i did not hand rub( before n after seeing pt). He said u(me) should hand rub..... iv fortum???, no clubbing, no tremor, no cyanosis, lymph node (xcheck), trachea xdeviated (but in CXR trachea deviated, inspiratory coarse crepitation and occasional ronchi (from middle to lower zone), i mentioned present of pleural effusion (actually no pleural effusion), bcoz i think present stony dull. 6. Diagnosis: Bronchiectasis (pt told me), when presenting hx, i did mentioned a diagnosis had been made, Prof X ask me " do u know the diagnosis? I anwred " yes, bronchiectasis, pt told me" Pf. X " it's an medical term, does pt really told u?" yes, pt really told me".. They are not asking about differential 7. Questions asked by lecturer: Pf. X a) what the diagnosis? (already mentioned above) b) this pt require a/b for rest of life,, why?? c) what do u do if u see pt came to the hosp? d) what investigation u would do? He give me cxr Ring lesion.. What is it imply? e) what cause bronchiectasis? I mentioned a1 antitrypsin def, then he ask what is a1at def? f) how would u manage her? (actually he asked a lot of questions, but can remember all) He finished... Bell not rang yet He asked prof yip n pro siti, anything they want to ask Prof Yip continued a) let say, pt go for operation for perforated peptic ulcer, what is ur concern? b) what assesment do u do before surgery? Lung function( spirometry) c) what parameter u look in spirometry? (FEV1 and FVC) last Tuesday Report
Shafiq Papik 1. lecturers who took u: Dr yeaw* an external surgeon, the main examiner, Prof Cheah *external paeds and Prof Philip Poi
2. specialty: Surgery 3. chief complaint: 49 y/o lady presented with painless lump on the right breast for 4 months. 4. brief history: post menopausal for 5 years. no other medical illness. lump noted in november. one painless lump, hard in consistency, no discharge, no skin changes, no other lumps noted. the only main breadwinner in the family. the only risk factor, age and oral contraceptive pill, depot progestogen. Past surgical hx; bilateral tubal ligation. 5. PE finding: painless lump noted on the upper quadrant. at midline with dilated vein. skin dimpling noted. lump is not attached to skin or muscles. mobile, hard in consistency, edge is well defined, size 2 x 3 cm. no lymphadenopathy. 6. diagnosis: breast Ca 7. questions asked by lecturer: differentials; throw out everything including benign breast disease, fat necrosis, duct ectasia. If see this first in the clinic, what would you do? take a proper history. do the triple assessment. explain about triple assessment. indications of choosing core biopsy than fine needle aspiration cytology. staging of the disease ( TNM staging). indications of mammogram and ultrasound. explain the mammogram ( no clacification noted on the right upper quadrant of the breast). then how would u treat this patient. ( I screwed the qestion alot!). surgery; lumpectomy, mastectomy, and breast conservative surgery. indications. (yet I quote too many from Burkitt which happen the external surgeon did not read it -_________)..chemotherapy. Tamoxifen the estrogen receptor blocker pun ditanya. then how to screen women nowadays if I were happen to be the deputy DG one day. I answered breast lump? NO. Family history? NO!!!! ring ring. I begged him to answer the question; mammogram for certain age. (please read this in the newspaper today)... Short cases pulak :D last Tuesday Report
Chew Kee Seang 1. Prof Philip Poi, Prof Cheach (UKM neonatologist) , another external 2. specialty: medicine 3. chief complaint: exam 4. brief history History of recurrent MI for2 times in 3 months period, presented last year. Now
having CCF symptoms orthopnoea, leg swelling, reduced effort tolerance. I start off presenting a symptoms history on MI last year and how he progressed to CCF with the typical symptoms. Accessed the ADL. 15 years ago diagnosed DM, presented with 3P and weight loss. poorly controlled, changed to basal bolus insulin after MI, good control. Multiple episodes of hypoglycemia. Many complication of DM: recurrent abscess on skin, frothy urine with proteinuria, bilateral cataract but no retinopathy, bilateral numbness up to mid shin, no diabetic foot ulcer before as he was educated on foot examination, no unilateral body weakness, no bilateral leg pain on exertion. on metformin hypertension 5 years diagnosed after screening. has multiple episodes of postural hypotension. hyperchol 4 years. Spine TB 8 years ago, presented with sudden onset severe back pain asso numbness of LL and shooting pain. then had multiple spine surgeries and bed bound for 1 year. subsequently recover, regain full function but still have residual pain BPH 1 year. on xatral (alfuzosin) and symptoms were relieved. fracture right tibia 20 years ago with ORIF and treated. mild deformity. strong family history od DM hpt chol. brother died at 54 due to MI, father died at 74 due to MI. mother got stroke. drug history a long list.... metformin, insulinatard and actrapid, perindopril, lasix, spironolactone, bisoprolol, plavix, aspirin, vactarel, xatral. no allery NO smoke, no alcohol, married, sedentery lifestyle, diet: high fat high salt. thats all. 5. PE finding: raised JVP (must show prof philip), displaced apex, loud P2. typical DM leg changes (diabetic dermopathy, atrophy skin, shiny, loss of hair, no dorsalis pedis pulse, no ulcer. sensation lost up to mid shin. SLR SST positive at 30 degrees. 6. diagnosis CCF secondary to MI. with..... 7. questions asked by lecturer (prof philip) why patient has recurrent MI? what is so special about atherosclerosis in THIS patient? do u think surgery better? how to access pre op fitness? what is lung function test? RINGgg........
(prof cheah) what is the management of MI? like that la......kin jiong lo, really not enough time to clerk. last Tuesday Report
Hadi Anuar 1. lecturers who took u : Prof Rokiah Ismail (main) Prof Hani & External Examiner 2. specialty : Medicine 3. chief complaint : no active chief complain came for exam 4. brief history : 33 y.o Chinese man presented to UMMC 14 years ago (1997) with high fever & progressive bilateral leg swelling. Referred to GP multiple times, treated with Ab and PCM but fever kept coming back. Developed progressive bilateral leg swelling over 3 days, referred to Assunta Hospital. Multiple ix done, diagnosed to have SLE. Switched to UMMC due to logistics. Started on high dose oral prednisolone since then. Not compliance to meds due to acne, proximal myopathy. Relapse nephrotic in 1998, renal biopsy done -> GN 2nd to lupus nephritis. remained normotensive. started on cyclophosphamide for 1 year. didnt develop s/e. again not compliance, relapsed 2nd time in 1999. remained asymptomatic till 2008 where he developed AVN of left femur 2nd to steroid in 2008, left hip arthroscopy done to repair with bone graft. other symptoms of SLE during 1998-1999: alopecia, malar rash, photosensitivity,mild arthralgia. others were not present. 5. PE finding stretch mark due to previous ascites, scar on left flank due to arthroscopy. not cushingoid. protein 3+. 6. diagnosis SLE with lupus nephritis. 7. questions asked by lecturer epidemiology of SLE in Malaysia, ethnic group, ratio female:male common presentation of SLE - in comparison to this patient? why do u think his presentation is unusual? Side effects of prolonged use of steroid? does he has features of cushing's? would you send him to ophthalmologist (cataract)? how would you monitor this patient on daycare basis (BP, proteinuria, glucosuria)? how would you persuade him to be compliant?
Prognosis of this patient? (RF) what is the normal function of kidneys? (erythropoietin, hemostasis, toxic excretion, blood pressure) how would you advice him?(ESRF-->hemodialysis, needs fistula) if ur in remote area and this patient presents with severe acidosis? (peritoneal dialysis) how do you perform peritoneal dialysis? what fluid do u use? Role of renal transplant in this patient? (no point transplant, develop antibody) bedside: show me ur positive findings. how do u elicit prox myopathy? does he has any features of cushing's? last Tuesday Report
Teo Hock Gin Please present your long case following this format. 1. lecturers who took u: main examiner prof pan (external), prog ong, prof ida 2. specialty: orthopaedics (OI) 3. chief complaint:OI diagnosed in pregnancy, multiple fracture, electively admitted for op tomorrow 4. brief history Diagnosed in pregnancy by ultrasound, multiple implant, blue sclerae dental abnormality, aug 2010 fracture for left tibia with implant failure..No other medical problem 5. PE finding multiple deformity and deformities, blue sclerae, short stature, dental abnormality.. Decsribe the abnormality, show how to check for hyperelasticity.. 6. diagnosis OI type III 7. questions asked by lecturer All questions asked by external examiner... Do u agree with the diagnosis of OI? How to classify OI What do u think the OI type for ur patient? What is the treatment for OI? what is the action of pamidronate? Interpret x ray?previous fracture...describe... is it union? Second Xray? with nail inside? what is the nail? i dunno ...check online i think is self expanding nail. This patient had nail inside and fracture, what do u think had happened? fracture of the nail...will u using the same nail for replacement?.... This patient had fracture at birth treated by casting, do u agree with the treatment? when u want to start internal fixation?...
What is the complication of the nail? i answered growth plate injury reduced growth...actually is increased growth(from internet) last Tuesday Report
Peng Loon Cheah Same as kee seang's case lo.. 1. lecturers who took u: Prof Philip Poi, Prof Cheah Fook Zhoe (External UKM), Dr. Wong (not sure from where.. um?) 2. specialty: Medicine 3. chief complaint: Came for exam. Last admission 8 months ago with chest pain. (MI) 4. brief history: - Last year two episodes of typical MI symtoms, done angioplasty and discharged with aspirin and clopidogrel. Had acute pulmonary edema, some ascites, no leg edema. Dunno got CCF or not, but i clerked as MI. - 18 year history of DM with complications - 4 year history of hpt - 8 year history of TB spine - BPH on Xatral - previous distal tibia fracture 5. PE finding Same as kee seang's oso lo.. I found JVP oni 3 cm (which is wrong lo >.<) 6. diagnosis Myocardial Infarction with all those chronic probs lo.. Not asked for diagnosis also. 7. questions asked by lecturer a) What important physical findings u found? Me: BP normal. Checked for postural hypotension. (Yay he's happy :P) b) What is considered significant for postural hypo? (>20mmHg systolic) c) I said JVP only 3 cm.. not raised.. he said sure? Ok.. straight to see patient. d) Show to elicit JVP. First try still point to the 3cm point, then he ask to look again then found a higher point lo.. e) How you confirm its a JVP? What is normal JVP? Me: Not palpable and slightly enhanced by hepatojug reflux. (Prof: What slightly? Either got or dun have..... of cos say got lo) f) What else in CVS? (This one really SWT) Me: Apex not displaced Prof: Where's the apex? I pointed lo below the nipple 5th ICS, then i said okla.. displaced 1 cm) Then prof go feel high up in the axilla (above the nipple line weyh) then ask me
feel.. i can't feel oso finally he put one finger there ask me feel. So finally i felt. Then prof said.. hmm interesting.. this patient has two apex beats.. (hopefully that means i'm not screwed la..) g) What are the causes of displaced apex beat? What is definition of apex beat? h) What bruit would u expect to hear? Me: Carotid bruit? U mean murmur ah? (Prof: Of cos la.. aren't murmurs bruits?) Me: ok.. mitral regurg due to dilatation i) Show the loss of hair on the shin, peripheral neuropathy. j) What else u look for in the legs? (already covered ulcers, fungal infections in web spaces.. dunno what else d) His answer is callouses h) Did u feel dorsalis pedis pulses? OOPS FORGOT OMG.. then feel in front of him.. left leg got, right leg absent. Posterior tibial present. Tell me how diabetes causes peripheral neuropathy. (Dunno.. can guess? he said ok.. so i said hyperglycaemia causing myelin and schwann cell damage.. he said yea.. but HOW? I said due to osmolarity imbalances.. then he said i'm going further off track.. nvm d) i) Did u check urine? Yup.. got trace protein oni.. the rest normal. OK back to room j) He has trace protein, so what's a better way to quantify it? Me: 24 hour urine? (what else?), uFEME (talking nonsense d.. wrong oso of cos), microalbuminnuria (YES YES all nodding head) k) How u test for microalbuminuria? Me: ERR.. order oni lo.. (all laugh..sarcastically say just tick in the form oni right? then prof philip say actually is dipstick oni) l) Does he have hypoglycaemic attacks? (OMGGG forgot to ask again.. sorry prof. Prof: say sorry to patient, not me) m) Ok.. he actually has morning hypoglycaemia. How u want to manage? Me: Err.. assess the prev. night management. maybe ask him to take snacks before sleeping. Prof: Anything else? (I dun dare to lower insulin.. scared cannot and its a serious mistake then straight fail.. so just stone there lo..) So u mean u only give snacks and dun do anything else? Me: Erm.. yeah i think so.. and monitor lo.. Prof: U give him insulin and he got morning hypo u still dun wan change ah?? (SO strong hint d so i say YAYAYA WANT TO LOWER INSULIN) =.=" n) Ok.. so he has proteinuria, what medication u wanna give? (ACE-I) o) Why? (Proven to reduce proteinuria and progression to renal failure gua) p) Why ACEI can reduce proteinuria? (Dunno.. stone few seconds..) q) What are the side effects of ACEI? (transient rise in creatinine and CI in bilat renal artery stenosis) r) Ok.. Why got transient rise in creatinine? (Dunno.. just studies show oni.. stone there again) Prof: Its related to afferent and efferent vessels. Me: Err.. maybe reduce blood flow to afferent vessels? Prof: A- or E- fferent? ( I said A-fferent).. Then he said ok nvm.. u can go now.. (wrong lo i guess) last Wednesday Report
Yip Hing Wa Main Examiners: External (russia), plus Prof CT Lim and Prof Azmi (both of them silent only) Specialty: Surgery C/O: 63 year old Chinese man intermittent painless per rectal bleeding HOPI: Dec 2010, 1st episode of per rectal bleed stained on toilet paper, otherwise no abd pain, tenesmus, fever or altered bowel habit. Stool stained with stale blood and mucus with more loose consistency. No anemic, constitutional, metastatic symptoms at all. No risk factor other than ex smoker for 30 packyear. Stop 8 years ago (forget to ask why). Went to private clinic, DRE notice some mass, arranged for colonoscopy 2 weeks later. Colonoscopy showed rectal mass and sigmoid polyps. Biopsy done rectal polyps and benign sigmoid tumour. Refer to UMMC for management. Just had surgery done 3 weeks ago and plan for chemo in April. PMH: generalized psoriasis for 20 years, first presented with skin lesion in left forearm and spread diffusely. Biopsy confirmed psoriasis on treatment (medication alternate day I think is MTX) now got left knee pain (I ignore it). No DM, HPT, IHD, Asthma (thank god) No PSH other than colonic surgery. Allergy to sambal (swt=.=) No family history, social half than examiner ask stop d. Question: Differential diagnosis (colorectal ca, diverticular dz, angiodysplasia, polyps, IBD) What is character of stool repeat and he ask difference with malena.. Then difference of bleeding in colorectal ca with diverticular dz (dunno goreng different site different color. He said ok nevermind.) What is angiodysplasia? Then go to patient. Show abdomen examination multiple scars, 4 laparascopic scars with 1 transverse LIF scar, tenderness and mass like thing at scar site. I said got mass. He ask do u want to consider is induration as a result of surgery? YES YES YES!! Showed how to palpate for liver. Why important to know liver size? Back to room and disaster started: Investigation: - FBC, LFT, CEA, CT TAP Why CEA? Function? Why CT TAP? I said staging. What do u mean and please elaborate. (as opposed by Prof A must precise =.=) Showed CT scan and point me the abnormalities. (no one rescue me. Luckily tembak correct) Where the tumour will spread to? (not iliac, not inguinal and not left supraclavicular, he wants spread radially to mesentery) What operation the patient has. (anterior resection) Tell me about ant resection. How many types. (tembak high and low. he said 3
types) How long is the rectum? (tembak 10cm. ans: 15cm :( What is the difference between each anterior resection. ( I said sphincter involvement. Ans: that is APR. Nvm) Do you heard mesorectal excision? (yaya coz the tumour will 1st spread to there and blah) Why patient had so many laparascopic scar? For operation lo. Whats the difference between laparatomy and laparoscopy? Which 1 cheaper? I said laparascopy cheaper coz less hospital stay then answer the other way although stay longer coz expertise needed. =.= Patient what stage? I said stage 3. Tell me staging. I said TNM and Dukes. He ask about dukes. Apparently rectal ca only up to Dukes C. wrong again. Then prognosis each stage. I said stage I 80%, II 60-70% and III 20%. He said III less than 5%. Swt =.= What complications from the surgery? I said all. the end he prompted me to say anastomosis leakage. How u prevent DVT? I said early mobilization and anticoagulant (forgot TED stockings.) what is the dose for DVT? (depends which type of heparin. Examiners: so?? bell rang!! i tembak 1mg/kg at the end he wants low dose only) Good luck everyone in short case exam!!! last Wednesday Report
Teh Cheah Hooi Prof Apri(main examiner)l, Prof David Choon, Prof Hussein Specialty: Surgery History: Right painless breast lump for the past one year. Increased in size with some skin changes~~ bla bla bla! all the lump history as we clerk as usual. Nothing else significant. no constitutional symptoms, no signs and symptoms suggestive metastsis. No risk factors. Went to seek traditional medication. Prof david choon asked: do u know what the traditional medicine she took? he means for Malay 6traditional medicine? i'm not sure?! then brought by the son to UMMC here for further management. Patient was not sure who's the Dr in-charge, what investigation she had undergone?? She just said she was admitted to there and was given IV drip?? WHAT?? Is it Neoadj chemo? But I forgot to ask if the any hair loss after this drip? Not sure with this since patient was not sure. She kept denying she had undergone any procedure even though she had 2 scars on both breasts. Then i jz carried on with the rest of the history. Other than that, jz hypertension for the past one year, good controlled with no complication! P/E: as usual all the lump examination. Otherwise not much significant except
for the traced proteinuria. Prof didnt ask me to present P/E also, straight away go there and did short case. Breast lump examination! Elicit the signs if there are metastasis, lung for pleural eff, bone pain(path frac). Jaundice, brain.. As we walked along to see patient, what diff u want to consider if she is a young patient-2 5 year old?! I forgot others d?! Questions: Diagnosis based on the history and P/E Why u said breast cancer?! Analyse the history and give the supportive points. What investigation u want to do if the patient initially present to the clinic. The triple test. What is triple test? Whats diff btw FNAC and tru-cut biopsy. Which one better and what's the complications. Mammogram is better, why? Whats the common place the tumour metastasis? if the tumour mets to other place, what u expect to find in the history and P/E. if mets to bone which blood iX u want to do, ALP level! Other than that, what imaging u wants to do? Staging of the patient. T3N0M0. What surgery is preferred? Wide local excision? Mastectomy? Radiotheraphy, chemotherapy? Elaborate all the management. Do u read the journal?(asked by Prof david choon)? Erm.. hehe.. no la.. jz update from the internet lo. How u want to treat this if the patient refuse to go for surgery,chemo, radio? How how how? I said keep on following up the patient and tell her to go for surgery since its still a preferred management. But, if the patient still refused?! RING then Prof April said, do u know Estrogen receptor!? Oh ya, I said tamoxifen and aromatase inhibitor, bla bla bla.. Some of the Qs could not remember d, this is what I could get. Good luck everyone =) last Wednesday Report
Chai Chau Chung 1. lecturers who took u Prof david choon (ortho) , prof hussain (psy), prof april (surgery) 2. specialty ortho 3. chief complaint low back pain for 6 yrs 4. brief history fall down 20 yrs ago, low back pain started 6 yrs ago with bilateral shooting pain on both legs, now come in for further management, prefer not to do surgery.Pt active in sport. Got previous adjustment disorder and came to ummc psy clinic. Got previous alcohol drinking problems. Got bronchitis and hypertension. 5. PE finding Demonstrate spine examination and lower limb examination to examiners.Name
and show the dermatomes and myotomes. Right antalgic gait. Straight leg raising test negative. All other ortho findings negative. 6. diagnosis Prolapsed intervertebral disc 7. questions asked by lecturer Other ortho system that u want to check that can lead to back pain? The ans is hip examination. what is the initial movement loss in hip OA? The answer is hip rotation. OA changes in spine. (bla, bla, bla...) Expected x-ray findings of patient. Investigations to be done. Interpret X-ray and MRI. MRI showed 'black disc'. Show and name all the structures in MRI film. (psoas muscle, dura, bla bla bla). Patient dun want to do surgery, what should u do? How to advice him to do surgery.How to give counseling before surgery bla bla bla. Success rate of spine surgery? When can patient recover? When can pt start to go back to work? After finish answering, the bell rang already. last Wednesday Report
Kejal Udani from kejal : BTW, my lecturers were : Prof CK Liam, Prof Jessie Bruyne, dr sofea, and an observer who asked a lot of questions... long case : indian lady with fibroid, pesented with a fall in bathrom ?anaemia ?? underlying asthma, and Diabetes Qs : d(X), why, how can u treat? when is HIFU better over myomectomy? i guess when its ONE large one.. side effects of UAE? post emboisation syndrome...not sure wat exactly.. why fobroid sudenly painful ? - degeneration? ischeamic necrosis? how to optimise b4 opt ? Lung function test, ecg, echo, insulin sliding scle if need wat type of anaemia ? IDA why ? storage depleted.. ix : serum ferrittin she appeared pale, guess her HB ? i dunno, just said 8g/L which medications : COC, tranexamic acid and NSAIDS on Wednesday Report
Ebner Yoon 1. lecturers who took u prof philip poi, prof cheah (UKM PAED) and perak prof 2. specialty paed 3. chief complaint periorbital swelling
4. brief history short history 2 days hx of periorbital swelling with abd and leg swelling, no scrotal swelling 5. PE finding. super well n playful boy.... outpt actually, currently in remission without proteinuria 6. diagnosis nephrotic syn on Thursday Report
Felicia Lau Prof Rokiah Ismail(med), Prof HAny(paed), external (none of my examiners from o n g, good news?? or nt???) Hopefully Obs: Placenta praevia type 4 43 year old, malay lady, referred from puspawi hospital d/t placenta praevia no active complaint previous lscs PE: SFH 37cm, correspond to date Oblique lie inverted nipple on right side Is LSCS predispose to pp?? Risk of elderly gravida How to screen for down syndrome during pregnancy?? dun wan chorionic villus sampling-invasive, blood test-alpha fetoprotein, beta hcg, estradiol ultrasound- nuchal fold thickness main on counselling- risk of operation to her. counsel in front of examiners patient dun wan op, any other alternative?? wat is the significance of inverted nipple? since when?? y u wan 2 knw?? tat all i can recall^^ on Thursday Report
Siti Khalimah 1. lecturers who took u : DR KL NG(leading) PROF ADEEBA(a bit of interruption) & DR NG(observer, consoling) 2. specialty : Surgery 3. chief complaint : Breast lump x3/52
4. brief history : 65 Malay housewife,menopause, known of DM, HPT, hyperlipid. Present with painless, immobile breast lump not changing in size since discovery.No nipple/skin changes. No discharge. Had mild prickling pain of the breast, fever (--> lead to discussion on breast abscess) LOA, no LOW. Risk factor: OCP 2years, female, elderly. No fhx of cancer. 5. PE finding : Symmetry breasts, breast non tender, no nipple retraction/discharge, no peau d'orange,no tethering, bruised overlying lump and site of FNAC. Lump --> superior medial quadrant of left breast, hard, not fix to deep muscle, fix to skin, painless, smooth surface, regular margin, size 5x5cm. 6. diagnosis : Breast cancer, breast abscess (?fever?pain) 7. questions asked by lecturer differential diagnosis investigations (triple assessment) other investigations? what to do if FNAC result return as ductal ca?--> inform patient (breaking bad news) do CT scan for staging, surgery on Thursday Report
Nor Haslinda Zainuddi 1. lecturers who took u : Prof Khoo (PCM), Prof Raman (paeds surg), Prof Mary? ( external ONG) 2. specialty: PCM 3. chief complaint: - No c/o la, come for exam...huhu.. history of dm n hpt for 16 years and dyslipidaemia for 8 years. 4. brief history - DM control not so good even compliance to medication. HPT reading is good. LDL and HDL not in normal range. educated person( an addmath teacher) and very nice. diet not really control n exercise less. ho other DM cx like IHD or diabetic nephropathy. previous eye check up shows peripheral hemorrange. dis pt got ED and on viagra. 5. PE finding - All normal except presence of skin lesion in DM and I'm not sure about the skin lesion so better know in and out bout DM k. 6. diagnosis -DM n HPT with dyslipidaemia with no symptoms of hyperglycaemia. 7. questions asked by lecturer
-Diet for diabetic patient. -How do u manage pt with HBA1c > 8? -Target HBA1c for dis pt? -Bedside: perform peripheral neuropathy examination and palpate pulses. -Ix for dis pt -side effect ARB and when u cannot use ARB? on Thursday Report
Ngam Pei Ing 1. prof siti Z (onG), prof yip (surg), prof Chim? (externa-medicine), A/P Zahar (observer but keep on giving opinion by non-verbal cues) specialty: Obs (GDM with ITP) History: no current chief complaint. but with GDM after OGTT not controlled by normal diet... on insulin monitoring. patient has ITP on predisolone. PE: normal singleton pregnancy... with feature of cushingnoid. wat to check? thyroid. why? breast. why? fundus. why? wat else?.... er.... wat about BP? yes... is important esp GDM will hv PIH as well... ok... how to check? on erect position. how to check? on supine position. how to check? Diagnosis: 1. GDM 2. ITP 3. Cushingnoid sx Questions 1. why tis pt need to do OGTT 2. wat is OGTT 3. Wat u shd advice to pt 4. wat diet hx... bla bla bla... 5. any snacks in btw? 6. wat is the normal calorie in pregnant women? wat about GDM? 7. as gestation age increase? wat is the trend of calorie u would expect? 8. wat is diabetic diet? give in details... how many calories 9. cx of GDM u would worry about 10. how u mx this patient then? 11. when can she delivered? 12 why? 13 how about her ITP? wat to worry about? 14 wat is her platelet now? 15 wat to advice to ITP patient when she is going to deliver? 16 wat the min plt level for ITP pt to deliver BB? on Thursday Report
Norazwa Ramli 1.Prof siti(o&g),prof yip(surg), prof ?(external med) 2.specialty:medicine 3.History: no current complain. background hx of mitral stenosis n valvular replacement done twice.1st on 1986 (bioprotheses),2005 (metal valve).last adm last month (feb2011) due to AF with heart failure.currently NYHA classification is stage 2 to 3.no other co morbit. on warfarin(anticoagulation), digoxin(rate control),atenolol(B-blocker), lasix(diuretic), sloking(K+ supplement). 4.PE:AF+tachycardic(100bpm) ---> not well control AF cardiomegaly + pedal oedema up to shin --->not complete recovery of HF no pleura effusion,no hepatomegaly,no raise in JVP 5.Diagnosis:AF in HF 6.Question: a.what happen during the 1st adm?what is the probable diagnosis? b.what happen on 2nd adm? c.why u say her NYHA classifation is 2 to 3?tell all the stage in NYHA d.do u think her heart prob is well control? e.what could be the valve abnormality for the valve replacement? f.what type of valve she had been replace with? g.why she was on warfarin?desired INR?how frequent to check the INR? wat u advise u should tel the patient?what precaution u should tale on her. h.explain why she was given the current medication.what other drug u can give to control the heart rate? i.how to treat HF in acute state? ji.if she come to u now what do u want to do? k.interprate ECG l.echo show her ejection fraction is low, what do u want to give her to improve her ejection fraction? Leong Yan Ning 1. Prof Ong Teng Aik (Surgery), Prof Ida (Medicine), Prof Poh (External, not sure which specialty) 2.Surgery -Breast 3. 64/C/ lady, c/o: left breast lump x 1 yr (electively admitted for surgery 2moro) 4. HOPI: progressively enlarge over 1 yr, hard, painless, no discharge & skin
changes, no LOW/LOA, no family hx of breast or ovarian ca, no previous breast lump PMH: THyroidectomy 20 yrs ago (i thk is MNG tat cause SOB & hyperthyroidism), Right renal cell carcinoma 5 yrs ago with radical nephrectomy, HPT, Hyperlipidemia, Hyperuricemia. 5. Breast: A lump in left upper outer quadrant, oval shaped, 5x6cm, hard, mobile, no skin changes or axillary lymph nodes involvement. No signs of mets. Abd: a well healed right subcostal scar measured 22cm Neck: a tyroidectomy scar, no lump felt. 6. Left breast carcinoma Diff dx: fibroadenosis, fibroadenoma (usually not at dis age), lipoma... 7. Mainly asked by Prof Ong :) Provisional & differential dx Perform breast exam on pt n present findings Name the right nephrectomy scar ( subcostal or Kocher scar aft he leads me, haha), what type of appraoch did d surgeon use in dis nephrectomy (Prf Ong gav me 2 choices: retroperitoneal or transperitoneal? transperitoneal appraoch since d scar is subcostal:>) What eye signs in hyperthyroidism pt n perform on pt (exophthalmos, lid retraction, lid lag, extraocular muscle weakness (diplopia in H pattern), another medical term of extraocular muscle weakness (Prof Ida dun wan opthalmoplegia) What you wana do aft P/E? (triple assessment: mammography & biopsy) Interprete mammogram of dis pt (CC & MLO view) What do u thk? (an opacity wif irregular margin, no microcalcification, no retracted nipple, no lymph node in an old age lady --> Breast carcinoma) Which stage is dis pt in nw ?(T3N0Mx) What u wana do next? (Biopsy- FNAC) What do u expect 2 c? (high NC ratio, mitotic changes, check for estrogen or progesterone receptor on cell) How would u prepare dis pt if u r a HO in ward? ( FBC for Hb level, cross match, LFT for preparation of chemo, RP (Dt previous right nephrectomy 2 look for renal impairment), ECG ( dt HPT, risk of MI), CXR ( baseline for anest, mets 2 lung n ribcage) External den ask: what alse u wana 2 do pertaining 2 d mets in dis case? is CXR sensitive? ( I said i would like 2 do CT thorax as well, since it picks up smaller lung lesion n mets) Den he asked hw sensitive it is? Do u noe hw small d lesion can a CT picks up? (I said i m not sure. I remb in radiological class was ard 0.51cm, but u all nid 2 double check) Which place breast ca tends 2 spread as well? (I said bone esp thoracic spine n ribcage) he den asked which site else? (I answered long boe n pelvis as well, i forgot what was his response) What test u would like 2 do 2 look for mets in dis case? (Bone scan--look for high absorption area) How would u manage her aft confirming it is breast ca? ( mastectomy dt large size lump although pt's size is C cup--can't do breast conservation surgery in lump >3cm, >4cm in large breast) Would u like 2 do axillary LN clearance as well? ( Do sentinel node biopsy, if d 1st node tat receives lymphatic drainage frm breast is infiltrated, do axillary LN
clearance straightaway) What r d complications of axillary LN clearance? (lymphadema n cutaneous nerve injury-numbness) How would u decide d level of axillary LN clearance? base on which muscle? (Pect. minor, level 1: lateral 2 pect minor, level 2: beneath pect. minor, level 3: medial 2 pect. minor) Does d prognosis in dis pt good? Hw would u predict it? (I said overall quite good, Prognostic factors in breast ca: axillary LN involvement, lump size, age (yonger age more aggresive), ER, PR & HER2 positive (better response 2 tx)) Bell rang & times up!! on Friday Report
Nur Nadiatul Asyikin 1.Lecturers who took u: Prof Yip (surgery main), prof siti zawiyah ( OnG) , Prof Chan (external,same with azwa n Ngam) 2. Specialty-Surgery 3. chief complaint & 4. brief history : 52 yo malay gentlemen , a chronic alcoholic drinker, currently has no active compliant, one week back, he has hx of fever for 2 days associated with epigastric pain for 6 hour b4 admission. epigastric pain, no radiation, no relieving Assoc w pain ( mild only) + chills but no rigors ,sob, tea colour urine, x realise jaundice, no pale stool 2 years back- hx of gallstone , ERCP done-stenting risk for hepatitis/liver disease-chronic alcoholic 5. PE finding: On examination: forget to calculate BMI!!..at first thought he had ascites but its actually his fat. (aiyoo~ ZZZzz) the only positive sign is palmar erythema. No positive Murphy sign.. (prof yip reconfirm back with him bcoz, previously he said theres pain.. but this time he denies n all the profs laugh) 6. Diagnosis- Ascending cholangitis (AC)secondary to gallstone 7. questions asked by lecturer 1)Dx 2)what are the stigmata of chronic liver disease ( at bed site) 3) what can u see from inspectionnothing except his obese 4)why do u say AC- charcoat triad 5) what is the other classification of AC Raynaud pentad (hypotension + alter mental status) 6) what MX at emergency- Resus, (prof say ok not much to resus.. then? )
Ultrasound, interprate U/S, this is us of mr amirudin,taken on...written there CBD dilated.no presence of stone How do you know its dilated?--> the measurement is 1.63mm (written there with * on top), So whats the normal CBD? 0.5mm 7) now , what else u like to do? Blood ix,so inteprate n summarize the finding, increase wbc n bilirubin n liver enzyme n blood glucose How many percentage of increase conjugated bilirubin does it considered as significant.. 75% Why does liver enzyme derrange? Bcause AC , what liver enzyme indicate obstruction? GGT n ALP. How do you know liver enzyme deranggement is due to AC not liver disease ..albumin normal,coagulation normal. Blood glucose high. So? Patient need to be screen for DM.. what to do.. i answer OGTT but actually they want me to answer fasting blood glucose 8)patient had stent, why do you think he had AC? Stent dislodge (ptn told me) , stricture, block from residual stone...then cannot think anymore..prof answer impaction due to slough/mucus plug 9) why patient can have infection in choledocholithiasis, im thinking of complex mechanism but prof only want me to answer ascending bacterial infection .. 10) what common organism, dunno why i answer s.aureus (with confidence but of coz salah), then i answer anerobes, E.coli and klebsiella ( gut organism), so antibiotic? Metronidazole and cephalosporin 11) what else do you like to do in this patient, i answer ERCP ( now prof siti says, patient had ERCP done already.. what else..)owh, colecycstectomy... prof yip want me to answer cholecycstectomy n exploration of the bile duct to prevent recurrent.. 12)other mx? Follow up n give antibiotic (if havent completed ) P/s:Hope we all pass..Did mess up here n there. Lecturer will help ya.. Good Luck juniors~ Same case with cindy.. that all that i remember~ if theres anything else just add ok.. ^_^ on Friday Report
Chuan Chun Lim Lec: Prof Phillip (Med), Prof Nik(PCM), Prof Thambi (Paeds Surgery) All questions by Prof Phillip Main Problem: TIA and polycythaemia,5 years ago Currently no C/O. Came for exam purpose. HPT 5 years. When i presented my hx, Prof Phillip asked 1. What CT scan findings of the brain you expect to see if patient come into A&E? 2. Why the Doc changed Aspirin to ticlopidine in polycythaemia? Zzz Then Prof said it was a high tech question. I only figured it out be4 i sleep... 3. For Aspirin, how many percent of patient will have GI problems?
PE (they mainly want to see the skills) Show power, reflex, clonus, visual field. Only have hyperreflexia. Others they want to see the skills. Discussion 1. Tell me about polycythameia? How many type? 2. Show me the FBC result, interpret. All cell line raised. 3. What is this condition called? I became thought block. Zzz myelo.....dysplasia. No!! then i said myelo.......proliferative d/o. They accepted the answer. 4. What is hydroxyurea? Anti-metabolite...... 5. What is perindopril? ACE-I....... 6. What is ticlopidine? Antiplatelet...... Patient came to your clinic. How would you check for polycythamia? Conjunctival plethora. What else? I keep talking hand, bla bla all rubbish then they said cyanosis. Why polycythamia patient will have cyanosis? I keep talking rubbish again until i said hypervicosity, blood stasis, and then only they let me go. Zzz,, serious thought block when they throwed me the Q !! really screwed up!!!! on Friday Report
Kamariah Ahmat 1. lecturers who took u - prof ida, prof ong, external 2. specialty- medicine 3. chief complaint - 63/malay gentleman c/o left sided weakness 4. brief history - background history of hpt for 20 years, dm for 10 years and asthma presented with a c/o left sided weakness..sudden onset on 2006..admitted for 20 days..non-compliance to medication 5. PE finding - left hemiplegia- flexion contrature, grade 4/5, hypertonia, hyperreflexia, upgoing plantar, sensory intact 6. diagnosis - left sided stroke 7. questions asked by lecturer a) question related histry - why patient not compliance to medication b) why this patient have flexion contracture c) imagine u're a doctor in-charge at ane, patient presented like that, what do you want to do n why? d) what is the severity of his stroke?..i'm not sure what she want e) what d difference with anterior and posterior artery circulation stroke presentation? f) she want me to describe ct scan...but bell ringgggg...
on Sunday Report
Potrebbero piacerti anche
- Long Case PaedDocumento21 pagineLong Case Paedwhee182Nessuna valutazione finora
- Gallbladder Ca, Colon Ca, ParathyroidectomyDocumento25 pagineGallbladder Ca, Colon Ca, Parathyroidectomywhee182Nessuna valutazione finora
- O&G Long Case Exam QuestionDocumento21 pagineO&G Long Case Exam Questionwhee182Nessuna valutazione finora
- Medicine Long CaseDocumento26 pagineMedicine Long Casewhee182Nessuna valutazione finora
- Family Medicine - General Practice MEQ 2006Documento6 pagineFamily Medicine - General Practice MEQ 2006jermie22100% (1)
- !the H Book For 5th Year OSCE - Part 1Documento147 pagine!the H Book For 5th Year OSCE - Part 1farzzana100% (1)
- OSCE Melb11Nov06Documento7 pagineOSCE Melb11Nov06janaka1022Nessuna valutazione finora
- PRO III 2012 Long Case (Surgical)Documento39 paginePRO III 2012 Long Case (Surgical)vijayaNessuna valutazione finora
- ONG OSCE History and Counselling - Chris BrethertonDocumento13 pagineONG OSCE History and Counselling - Chris Brethertonddewoolkar100% (3)
- Gynaecology History Taking GuideDocumento7 pagineGynaecology History Taking GuideJahangir AlamNessuna valutazione finora
- Gi Long CaseDocumento8 pagineGi Long CaseNadia SalwaniNessuna valutazione finora
- Case Write UpDocumento8 pagineCase Write Upaladawi930100% (1)
- Ten-Minute History-Taking and Physical Examination Station ExampleDocumento2 pagineTen-Minute History-Taking and Physical Examination Station ExampleMin MawNessuna valutazione finora
- 14 - Toronto Notes 2011 - GynecologyDocumento52 pagine14 - Toronto Notes 2011 - GynecologyZiyad100% (4)
- History TakingDocumento19 pagineHistory TakingAlice Verran100% (1)
- R 5th Year OSCE - Part 2Documento230 pagineR 5th Year OSCE - Part 2Leon RajanthiranNessuna valutazione finora
- UMMP Guidelines For ExaminationDocumento28 pagineUMMP Guidelines For ExaminationayuniNessuna valutazione finora
- MBBS2014 SurgeryCaseAnalysisDocumento194 pagineMBBS2014 SurgeryCaseAnalysisDaniel LimNessuna valutazione finora
- !THe H Book For 5th Year OSCE - Part 1 PDFDocumento147 pagine!THe H Book For 5th Year OSCE - Part 1 PDFMalvinder Singh DhillonNessuna valutazione finora
- Endocrine Long CaseDocumento8 pagineEndocrine Long CaseNadia SalwaniNessuna valutazione finora
- Long Case Parkinson's DiseaseDocumento4 pagineLong Case Parkinson's DiseaseNadia SalwaniNessuna valutazione finora
- OSPE EXAM OF OBSTETRICS AND GYNAECOLOGY (AFMG 2017/2018Documento43 pagineOSPE EXAM OF OBSTETRICS AND GYNAECOLOGY (AFMG 2017/2018Nabilah Mohammad KhalisNessuna valutazione finora
- Cwu 1 OrthoDocumento14 pagineCwu 1 OrthoHakimah K. Suhaimi100% (1)
- A Brief Sample Content of The " PACING THE PACES Tips For Passing MRCP and Final MBBS"Documento24 pagineA Brief Sample Content of The " PACING THE PACES Tips For Passing MRCP and Final MBBS"Woan Torng100% (2)
- O&g Osce BookletDocumento3 pagineO&g Osce BookletJohn TangNessuna valutazione finora
- Practice OSCE - Breaking Bad NewsDocumento1 paginaPractice OSCE - Breaking Bad NewssilverangelkickinNessuna valutazione finora
- Managing Multiple Trauma InjuriesDocumento9 pagineManaging Multiple Trauma InjuriesMia MusNessuna valutazione finora
- Year 6 Clerkship - Welcome & Curriculum Class 2020 (Revised 25.04.2019)Documento190 pagineYear 6 Clerkship - Welcome & Curriculum Class 2020 (Revised 25.04.2019)Ali SemajNessuna valutazione finora
- OSCE Marksheet 1Documento7 pagineOSCE Marksheet 1Elias PetrouNessuna valutazione finora
- Pediatric OSCE A Guide For Medical StudentsDocumento9 paginePediatric OSCE A Guide For Medical Studentsjoey92leeNessuna valutazione finora
- Case Write UpsDocumento4 pagineCase Write UpsMuhammad AzmanNessuna valutazione finora
- PRO 2012 Short Case (Surgical) CompilationDocumento24 paginePRO 2012 Short Case (Surgical) CompilationvijayaNessuna valutazione finora
- Pediatric Case Write-UpDocumento10 paginePediatric Case Write-UpZul Hisyam Fikri100% (1)
- Fmge Plan For June 2021Documento4 pagineFmge Plan For June 2021Integrated LearningNessuna valutazione finora
- OSCE Guide, University of Queensland School of MedicineDocumento86 pagineOSCE Guide, University of Queensland School of MedicineDarren Pang100% (2)
- Gyne Case COCDocumento37 pagineGyne Case COCLian BaylosisNessuna valutazione finora
- Long Cases in General Surgery: 2nd EditionDocumento259 pagineLong Cases in General Surgery: 2nd EditionDiornald Mogi100% (1)
- Hands:, Tablets, Wheelchair, WarfarinDocumento16 pagineHands:, Tablets, Wheelchair, WarfarinRhythm VasudevaNessuna valutazione finora
- UMS Medical Short Cases Records 1st EditionDocumento36 pagineUMS Medical Short Cases Records 1st EditionHendraDarmawan67% (3)
- Ospe For Revision ClassDocumento128 pagineOspe For Revision ClassHaseeb Sadi100% (3)
- Osce Book 3rdDocumento39 pagineOsce Book 3rdأحمد الكندي100% (1)
- PPIs Improve ENT Symptoms in GERD PatientsDocumento5 paginePPIs Improve ENT Symptoms in GERD PatientsHadia YaqubNessuna valutazione finora
- Accident and Emergency Posting Case Write UpDocumento8 pagineAccident and Emergency Posting Case Write UpAmbhi Gana0% (1)
- Ospe Bank PDFDocumento318 pagineOspe Bank PDFMed StudentNessuna valutazione finora
- OSCE Qs Internal MedicineDocumento29 pagineOSCE Qs Internal MedicineRancesh FamoNessuna valutazione finora
- HX TakingDocumento37 pagineHX TakingAya SalahNessuna valutazione finora
- OSCE Exam: Breast Lump Differential DiagnosisDocumento9 pagineOSCE Exam: Breast Lump Differential Diagnosismahmoud alhelal100% (1)
- Pediatric History - Dr. P. LopezDocumento15 paginePediatric History - Dr. P. LopezPipoy AmyNessuna valutazione finora
- 25.09.2012 Final Year OSPEDocumento21 pagine25.09.2012 Final Year OSPEsohebbasharat75% (4)
- Clerking An o & G CaseDocumento57 pagineClerking An o & G CaseAlan Na100% (2)
- Self Assessment Review of Pediatrics Preview PDFDocumento6 pagineSelf Assessment Review of Pediatrics Preview PDFMonowara Hussain0% (2)
- CLINICAL HISTORY AND DIFFERENTIAL DIAGNOSIS AT YOUR FINGERTIPSDa EverandCLINICAL HISTORY AND DIFFERENTIAL DIAGNOSIS AT YOUR FINGERTIPSNessuna valutazione finora
- A Brief Introduction to the Multi-Specialty Recruitment Assessment (MSRA)Da EverandA Brief Introduction to the Multi-Specialty Recruitment Assessment (MSRA)Valutazione: 5 su 5 stelle5/5 (1)
- Practical Gastroenterology and Hepatology Board Review ToolkitDa EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultNessuna valutazione finora
- CSA Revision Notes for the MRCGP, second editionDa EverandCSA Revision Notes for the MRCGP, second editionValutazione: 4.5 su 5 stelle4.5/5 (3)
- Motor Skills Inventory: Motor Development Clinic Cal Poly University, PomonaDocumento8 pagineMotor Skills Inventory: Motor Development Clinic Cal Poly University, Pomonawhee182Nessuna valutazione finora
- BurnsDocumento36 pagineBurnswhee182Nessuna valutazione finora
- Math D5 P1Documento23 pagineMath D5 P1whee182Nessuna valutazione finora
- Kumpulan J Kumpulan K: No Feet Have Two FeetsDocumento27 pagineKumpulan J Kumpulan K: No Feet Have Two Feetswhee182Nessuna valutazione finora
- Trial Percubaan UPSR Johor Matematik Kertas 1Documento17 pagineTrial Percubaan UPSR Johor Matematik Kertas 1whee182Nessuna valutazione finora
- SAINS A Percubaan UPSR 2014 - Bangsar Pudu - Sains - Bahagian ADocumento23 pagineSAINS A Percubaan UPSR 2014 - Bangsar Pudu - Sains - Bahagian Awhee182Nessuna valutazione finora
- Paper 2 Sains-UpsrDocumento13 paginePaper 2 Sains-Upsrwhee182Nessuna valutazione finora
- Trial Percubaan UPSR Johor Matematik Kertas 1Documento17 pagineTrial Percubaan UPSR Johor Matematik Kertas 1whee182Nessuna valutazione finora
- SAINS A Percubaan UPSR 2014 - Bangsar Pudu - Sains - Bahagian ADocumento23 pagineSAINS A Percubaan UPSR 2014 - Bangsar Pudu - Sains - Bahagian Awhee182Nessuna valutazione finora
- Kumpulan J Kumpulan K: No Feet Have Two FeetsDocumento27 pagineKumpulan J Kumpulan K: No Feet Have Two Feetswhee182Nessuna valutazione finora
- Long Case PCMDocumento10 pagineLong Case PCMwhee182Nessuna valutazione finora
- Standard Form Math Chapter ExercisesDocumento4 pagineStandard Form Math Chapter Exerciseswhee182Nessuna valutazione finora
- Introduction To Physics 1 PDFDocumento27 pagineIntroduction To Physics 1 PDFjgd2080Nessuna valutazione finora
- Criminal Incident Report FF-560-302Documento3 pagineCriminal Incident Report FF-560-302David100% (1)
- Lesson 2 The Culture Challenge in International Business ModuleDocumento10 pagineLesson 2 The Culture Challenge in International Business ModuleKuya ANessuna valutazione finora
- A Mother's Hidden Past and Guidance of Her ChildDocumento14 pagineA Mother's Hidden Past and Guidance of Her ChildNick Chock0% (1)
- Inglesudemy 1Documento647 pagineInglesudemy 1acamilongoNessuna valutazione finora
- المرشد العلاجي لالتهاب الانف التحسسيDocumento43 pagineالمرشد العلاجي لالتهاب الانف التحسسيyasinoNessuna valutazione finora
- Forces, Movement, Shape and Momentum 2 MS2Documento8 pagineForces, Movement, Shape and Momentum 2 MS2Jimmy QuintonNessuna valutazione finora
- CFA Level 2 NotesDocumento21 pagineCFA Level 2 NotesFarhan Tariq100% (2)
- Componentes de Ingles Pregunta 2Documento14 pagineComponentes de Ingles Pregunta 2Andres Salazar RoviraNessuna valutazione finora
- Supply Chain of MilkDocumento6 pagineSupply Chain of MilkFahad TatlaNessuna valutazione finora
- Full Download Ebook PDF Psychology 8e 8th Edition by Lester M Sdorow PDFDocumento41 pagineFull Download Ebook PDF Psychology 8e 8th Edition by Lester M Sdorow PDFandrew.wilson391100% (28)
- Physical Chemical Changes Lesson 2 ReflectionDocumento2 paginePhysical Chemical Changes Lesson 2 Reflectionapi-360585476Nessuna valutazione finora
- Sale of Goods (Sales of Goods Act 1957)Documento5 pagineSale of Goods (Sales of Goods Act 1957)Yee Zhi XuanNessuna valutazione finora
- CHAPTER VI CREATING BRAND EQUITY - Manansala - RolynDocumento16 pagineCHAPTER VI CREATING BRAND EQUITY - Manansala - RolynROLYNNessuna valutazione finora
- Flipbook Threshold DE PDFDocumento80 pagineFlipbook Threshold DE PDFRegulator0Nessuna valutazione finora
- Assignment 1 MCTE 3313 Sem 1 2018 2019Documento3 pagineAssignment 1 MCTE 3313 Sem 1 2018 2019Nurmi Elisya RosliNessuna valutazione finora
- An Introduction To Cancer Biology: When Good Cells Go BadDocumento68 pagineAn Introduction To Cancer Biology: When Good Cells Go BadSavitaNessuna valutazione finora
- Modeling CO2 Capture via Chemical Absorption Processes Literature ReviewDocumento21 pagineModeling CO2 Capture via Chemical Absorption Processes Literature ReviewRene QuisNessuna valutazione finora
- Letter From Julius Eckman To Solomon Nunes Carvalho, San Francisco 1855 (Transcription of Original Manuscript)Documento3 pagineLetter From Julius Eckman To Solomon Nunes Carvalho, San Francisco 1855 (Transcription of Original Manuscript)magnesmuseumNessuna valutazione finora
- The Paradigmatic Crisis in Chinese Studies: Paradoxes in Social and Economic HistoryDocumento44 pagineThe Paradigmatic Crisis in Chinese Studies: Paradoxes in Social and Economic HistoryYadanarHninNessuna valutazione finora
- Tinkle July 2019Documento176 pagineTinkle July 2019Ad85% (13)
- Jenitri 5Documento7 pagineJenitri 5Zaenal MubaroqNessuna valutazione finora
- The Lost Colony Journal ProjectDocumento2 pagineThe Lost Colony Journal Projectapi-224131798Nessuna valutazione finora
- Team Assignment 1 - Composing An Informational EmailDocumento1 paginaTeam Assignment 1 - Composing An Informational EmailHuỳnh Hồ Diễm NgọcNessuna valutazione finora
- RELATIONSHIP BETWEEN CENTRIPETAL FORCE, FREQUENCY, RADIUS AND MASSDocumento14 pagineRELATIONSHIP BETWEEN CENTRIPETAL FORCE, FREQUENCY, RADIUS AND MASSKenneth NyuNessuna valutazione finora
- Kirkham Last Supper and Passover HaggadahDocumento16 pagineKirkham Last Supper and Passover HaggadahChristopher MendezNessuna valutazione finora
- Introduction To Measurements and Error Analysis: ObjectivesDocumento17 pagineIntroduction To Measurements and Error Analysis: ObjectivesDeep PrajapatiNessuna valutazione finora
- Affidavit of Non Tenancy Rosalina LiaoDocumento2 pagineAffidavit of Non Tenancy Rosalina LiaoEppie SeverinoNessuna valutazione finora
- SILENT INVASION SAVE PAKISTAN CULTUREDocumento2 pagineSILENT INVASION SAVE PAKISTAN CULTUREMaira AleemNessuna valutazione finora
- Artifact - Autobiography Assignment Educ5004Documento6 pagineArtifact - Autobiography Assignment Educ5004api-246369228Nessuna valutazione finora
- 18PYB101J ManualDocumento38 pagine18PYB101J ManualRohit SinghNessuna valutazione finora