Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Respiratory Distress in Newborn
Caricato da
Chimot Ona MilanelloDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Respiratory Distress in Newborn
Caricato da
Chimot Ona MilanelloCopyright:
Formati disponibili
RESPIRATORY DISTRESS IN NEWBORN
B. VISHNU BHAT Prof. of Pediatrics JIPMER Pondicherry 605 006.
Address for communication B. Vishnu Bhat,
Prof. of Pediatrics, JIPMER, Pondicherry - 605 006. Email: drvishnubhat@yahoo.com
RESPIRATORY DISTRESS IN NEWBORN
Respiratory distress in a newborn is diagnosed when any two of the following findings are present for more than 2 hours after birth:Respiratory rate more than 60/ minute. Grunting Apnea Central cyanosis Accessory muscles of respiration working. The time duration of 2 hours is set so that transient adaptation to extrauterine life is not included. The incidence of respiratory distress may vary from 7 8 % among live births. The incidence varies from 30% among preterms, 20% among post-terms to 4% in term babies. CAUSES: The cause of distress may be within the respiratory system or outside. Pulmonary causes account for 80 85% cases of respiratory distress in a newborn. Table 1: CAUSES OF RESPIRATORY DISTRESS PULMONARY Transient tachypnea of newborn Hyaline membrane disease Meconium aspiration syndrome Pneumonia Pneumothorax Congenital lung cysts Diaphragmatic hernia Choanal atresia Laryngeal web/ polyp EXTRA-PULMONARY Cardiac failure Anaemia, Polycythemia Septicemia Metabolic disorders Renal failure, renal tubular acidosis Meningitis/ intracranial bleed Ascites
In a newborn, upper airway obstruction like blocked nostril or choanal atresia can cause severe respiratory distress since they are primarily nose-breathers. Severity of respiratory distress can be assessed using Downes score as shown in Table 2. Table 2: DOWNES SCORE SCORE PARAMETER 0 1 2 Respiratory rate < 60/ min 60-80 > 80 Cyanosis Nil While in room air At 40% oxygen Grunting Nil Audible with stethoscope Audible to naked ear Retractions Nil Minimal Marked Air entry Normal Reduced Almost absent A normal baby has 0 score while score 10 indicate severe distress resulting in impending death.
TRANSIENT TACHYPNEA OF NEWBORN: It is also known as Type II Respiratory Distress Syndrome or Wet Lung. It is the commonest cause of respiratory distress accounting for 40 45 % of cases. It occurs mostly among term and near term babies. The cause is increased lung fluid in the lungs. Generally 40 % of lung fluids get squeezed out during passage through birth canal and the remainder gets absorbed into venous channels and lymphatics. This may result from rapid delivery (precipitate or caesarian section) or poor respiratory effort resulting from perinatal asphyxia, respiratory depression from drugs and prematurity. The diagnosis is usually done by exclusion of other causes. Chest radiography may reveal increased bronchovascular markings, sometimes interlobar or subpleural effision. The condition is usually self-limiting and lasts for 12 24 hours. The baby needs intravenous fluids and supplemental oxygen. They may rarely require ventilatory support suggesting myocardial failure. HYALINE MEMBRANE DISEASE (Type I Respiratory distress syndrome): It is usually seen among preterm babies and rarely after 36 weeks of gestation. It is caused by decreased surfactant level in the lung. Surfactant reduces the alveolar surface tension and prevents collapse of alveoli during expiration. Alveolar collapse leads to poor oxygenation, hypercapnea and acidosis. The incidence is increased with decreasing maturity. It may occur among 80% of babies less than 28 weeks of gestation and in less than 5% after 36 weeks. Asphyxia, hypothermia, blood loss, Diabetes in the mother, male sex, caesarian section and erythroblastosis fetalis increase the incidence while intrauterine growth retardation, premature rupture rupture of membrane, heroin addiction in the mother and antenatal steroids decrease the occurrence of hyaline membrane disease. Predicting the risk for HMD: 1. Lecithin/ Sphingomyelin ratio (L/S ratio): If this ratio is less than 2, then there is increased risk. But in cases of diabetic mothers and erythroblastosis, a ratio of more than 3 should be taken for adequate lung maturity. 2. Shake test: One should take 1 ml of amniotic fluid or gastric aspirate of the baby and 1 ml of absolute alcohol in a test tube. Then the test tube is shaken for 15 seconds and allowed to stand for 15 minutes. The amount of air bubbles at the meniscus is noted and graded as follows:+ -- 1/3 of meniscus has bubbles ++ -- 2/3 of meniscus +++ -- one row along the circumference of meniscus has bubbles ++++ -- more than one row of bubbles The risk of hyaline membrane disease is minimal if the test is more than ++. Clinical Features:
The baby develops grunting, tachypnea, accessory muscles of respiration working and cyanosis, soon after birth or within 6 hours. The distress gradually worsens during the first 72 hours and then improves.
Diagnosis: Respiratory distress in a preterm baby with L/S ratio < 2 or positive Shake test suggests Hyaline membrane disease. Chest radiography initially shows fine reticulogranular pattern with air bronchogram followed by opalescence and complete white out lung fields. Lung biopsy if done shows hyaline membrane, which is made up of eosinophilic material. Hyaline membrane will not be present if the baby dies too early in the disease. Treatment: The baby needs intravenous fluids because of respiratory distress. Temperature control in order to prevent hypothermia and maintenance of acid base balance are important. Supplemental oxygen through head box or nasopharyngeal catheter is effective in mild cases. The severe cases will require ventilatory support. Artificial surfactant can be given intratracheally both prophylactically as well as therapeutically. The cost is prohibitive. Since one cannot differentiate conclusively hyaline membrane disease from infective
bronchopneumonia, antibiotics are given if the child is sick after collecting samples for bacterial culture. The survival is directly proportional to the maturity of the baby. The survival may be 50% with supportive care alone and > 90% with surfactant therapy and ventilatory support. MECONIUM ASPIRATION SYNDROME (MAS): Meconium consists of bile, intestinal secretion, amniotic fluid and exfoliated epithelial cells. About 10 12 % of fetuses may pass meconium before delivery. Meconium aspiration syndrome develops in 1 2% of deliveries or 10% of thick meconium stained liquor cases. Only 25% of meconium aspiration will result in aspiration syndrome. If meconium is seen below the vocal cords, baby has barrel shaped chest and respiratory distress, meconium aspiration is present. Chest radiography shows coarse nodular opacities, hyperinflation, air leak and sometimes consolidation or collapse. The commonest cause for respiratory distress is blocking of the airways by the meconium particles and hence develops immediately after birth. Sometimes chemical pneumonitis, secondary infection or air leak may result in respiratory distress. When distress develops after 24 hours, it suggests infection or air leak.
Treatment: The babys nutrition, temperature and hydration should be maintained through intravenous fluids and warming devices. Correction of acidosis will result in improvement by increased pulmonary circulation. Acidosis results in pulmonary vasoconstriction and
increase in pulmonary pressure. Supplemental oxygen by head box or ventilatory support may be needed for maintaining oxygenation. Since there is air loculation and emphyseme in this condition, the baby should be maintained with low end expiratory pressure. Surfactant has been tried by some with improved survival. Antibiotics are initiated if there is evidence of infection like foul smelling liquor, prolonged rupture of membranes, positive septic screening tests. Persistent pulmonary hypertension is difficult to manage. Hyperventilation and alkali therapy will help in improving pulmonary ciruculation. If they do not work, then Tolazoline or Nitric oxide may be tried. If they also fail in improving oxygenation, then Extra corporeal membrane oxygenation (ECMO) is the treatment. Complications: Blocking of airways leading to apnea, collapse of lung, air leak, consolidation, hypoxic brain damage and Persistent pulmonary hypertension are the complications. Mortality may vary from 15 20%. APNEA OF PREMATURITY: It is the cessation of respiration for more than 15 seconds or less than that with cyanosis and / or bradycardia. It is classified as follows:1. Central or idiopathic 2. Peripheral or obstructive 3. Mixed (commonest type). It can also be classified as primary and secondary. Primary apnea is the idiopathic apnea of prematurity due to immaturity of the respiratory center. Primary apnea most often manifests on the second or third day. When a newborn develops apnea after 3 days one should always look for an underlying cause. Secondary apnea results from underlying cause like sepsis, intracranial bleed, temperature instability, metabolic abnormality, anaemia, convulsion etc. When apnea is a manifestation of convulsion, there is
tachycardia unlike other causes. Apnea when prolonged can result in hypoxia and brain damage. Hence it is essential to identify and treat apnea. Treatment: Idiopathic apnea of prematurity can be prevented by Aminophylline/ Theophylline in a dose of 5-6 mg/kg/day to maintain a blood level of 10 12 g/dl. Other drug that is effective is Caffeine citrate. Doxapram although effective is not used because of side effects. If
apnea is persisting and recurrent, then Continuous Positive Airway Pressure(CPAP) or Intermittent Positive Pressure Ventilation (IPPV) may be needed. In cases of secondary apnea, the primary cause should be identified and treated.
INFECTIVE BRONCHOPNEUMONIA: Pneumonia may be observed among 0.5% of live births and 10% of low birth weight and sick newborns. The infection may be acquired before, during or after delivery. Transplacental infections are usually caused by viruses like Cytomegalovirus and Rubella virus. It may also result from Listeria or Treponema pallidum. The baby may get infected from the maternal genital tract during delivery. Premature rupture of membranes, prematurity, birth asphyxia and invasive procedures increase the risk for infection. The organism responsible for intranatal infection may be Streptococcus, Escherichia coli, Klebsiella, Enterobacter, Chlamydia, Herpes and Varicella viruses. Postnatal infections are usually caused by bacteria like Klebsiella, Coagulase negative staphylococci, Pseudomonas, Acinetobacter. Sometimes Chlamydia and fungi may also cause infection. Clinical Features: The baby may have grunting, retractions, tachypnea or apnea. There could also be temperature instability, reduced activity and other features suggestive of systemic infection. Investigations:Laboratory tests can be done for diagnosing sepsis and pulmonary involvement. Blood cell count, Band cell count, micro-ESR, C-Reactive Protein and blood culture are helpful in diagnosing sepsis. Blood culture and lung aspirate culture may be helpful in identifying the etiological agent. When intrauterine infection is suspected, gastric aspirate and tracheal aspirate at birth are helpful. Chest radiography will reveal the extent of
pulmonary involvement. Blood gas analysis will indicate severity of pulmonary disease and the need for ventilatory support. Treatment: It includes general supportive care and specific against infection. The nutrition, hydration and temperature are to be maintained. Oxygenation is maintained by supplemental oxygen by hood or mechanical ventilation. Antibiotics are to be selected based on the type of organism prevalent in the neonatal unit and later modified based on sensitivity pattern of the bacteria identified. A combination of third generation cephalosporin with aminoglycoside may be the initial combination of choice. Other modes of therapy involve granulocyte transfusion, immunoglobulin therapy and administration of GM CSF (Colony stimulating factor).
Key messages 1. Respiratory distress is an important cause of neonatal morbidity and mortality. 2. Transient tachypnea of newborn (TTN) is the commonest cause but it should be diagnosed after excluding other causes. 3. More than 80-85% of the cases the etiology can be identified in the respiratory system. 4. Chest radiography and septic screen are must in all cases of persisting respiratory distress. 5. Ventilatory support and good nursing care can improve the outcome. Reference 1. Kumar A, Bhat BV. Respiratory distress in newborn. Ind J Mat&Chld Hlth 1996, 7:8-10. 2. Kumar A, Bhat BV. Epidemiology of respiratory distress in newborn. Ind J Pediatric 1996, 63:93-98 3. Shuba S, Bhat BV. Meconium aspiration - current concepts. Quality care in Pediatric 1997,2:10-17. 4. Field DJ, Milner AD, Hopkins IE, Madeley RJ. Changing pattern in neonatal respiratory distress. Pediatr pulmonol 1987, 3: 231-235. 5. Hjalmarson O. Epidemiology of neonatal disorders of respiration. Ind J Technol assess Hlth care. 1991, 7:9-15.
Potrebbero piacerti anche
- (Treatments That Work) Gail Steketee, Randy O. Frost - Compulsive Hoarding and Acquiring - Therapist Guide-Oxford University Press (2006)Documento237 pagine(Treatments That Work) Gail Steketee, Randy O. Frost - Compulsive Hoarding and Acquiring - Therapist Guide-Oxford University Press (2006)mdmonzurh1100% (2)
- Ecg in Emergency Medicine and Acute Care-2005Documento420 pagineEcg in Emergency Medicine and Acute Care-2005Ioana Nicoleta Dinu91% (22)
- ADHD Parent Questionnaire PDFDocumento4 pagineADHD Parent Questionnaire PDFklichtNessuna valutazione finora
- Pyloric StenosisDocumento23 paginePyloric StenosisRama ItachiNessuna valutazione finora
- Spirit Releasement Protocol ListDocumento4 pagineSpirit Releasement Protocol ListKristen Hammer100% (5)
- Syllabus ElectrotherapyDocumento4 pagineSyllabus ElectrotherapySYED ALI HUSSAINNessuna valutazione finora
- Peter Pan Syndrome Is A DeepDocumento3 paginePeter Pan Syndrome Is A DeeptucklertNessuna valutazione finora
- The Kessler Psychological Distress Scale (K10)Documento2 pagineThe Kessler Psychological Distress Scale (K10)octavianNessuna valutazione finora
- Meno Pause&HRTsDocumento27 pagineMeno Pause&HRTsMajed AlhuzaliNessuna valutazione finora
- Fracture in ChildernDocumento56 pagineFracture in ChildernVicky Jessica EffendiNessuna valutazione finora
- Hospital and Its OrganizationDocumento16 pagineHospital and Its Organizationprathusha78% (9)
- Keehbauch Menopause HRT 4.2.16 SCDocumento55 pagineKeehbauch Menopause HRT 4.2.16 SCMuhammad AzkaNessuna valutazione finora
- Bleeding During PregnancyDocumento8 pagineBleeding During Pregnancyfernandezrachelle44Nessuna valutazione finora
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesDa EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNessuna valutazione finora
- Congenital Pulmonary Airway MalformationDocumento5 pagineCongenital Pulmonary Airway MalformationKiagusRoyNessuna valutazione finora
- Salpingitis: Sumber: 1. Dorland 2. Williams Gynecology 3. Better Health Channel Fact Sheet - SalpingitisDocumento6 pagineSalpingitis: Sumber: 1. Dorland 2. Williams Gynecology 3. Better Health Channel Fact Sheet - Salpingitisearthbend_tophNessuna valutazione finora
- Drug Study For Mini Case PRESDocumento11 pagineDrug Study For Mini Case PRESKevin AliasasNessuna valutazione finora
- Lotus BirthDocumento4 pagineLotus BirthindahNessuna valutazione finora
- Necrotizing Enterocolitis (NEC) : Intensive Care Nursery House Staff ManualDocumento3 pagineNecrotizing Enterocolitis (NEC) : Intensive Care Nursery House Staff ManualJovvitaNessuna valutazione finora
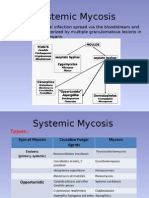
- MycosisDocumento5 pagineMycosisMaiWahidGaberNessuna valutazione finora
- Anorectal Anatomy & Surgical ManagementDocumento164 pagineAnorectal Anatomy & Surgical Managementsgod34Nessuna valutazione finora
- Complete Atrioventricular Canal (CAVC)Documento4 pagineComplete Atrioventricular Canal (CAVC)vivid1980Nessuna valutazione finora
- Anal Rectal MalformationsDocumento64 pagineAnal Rectal Malformationsdevtario100% (1)
- Submitted By: Diana M. Resultay A301/Group-3B Submitted To: Ms. ReyesDocumento9 pagineSubmitted By: Diana M. Resultay A301/Group-3B Submitted To: Ms. ReyesDiannetotz MoralesNessuna valutazione finora
- Respiratory Distress in Newborn FinalDocumento22 pagineRespiratory Distress in Newborn FinalajayganeshjNessuna valutazione finora
- Cholecystitis Cholelithiasis PresentationDocumento21 pagineCholecystitis Cholelithiasis PresentationPrincess Meinny JeanNessuna valutazione finora
- Respiratory Distress in NewbornDocumento32 pagineRespiratory Distress in NewbornCharu KalraNessuna valutazione finora
- Public Health CareDocumento20 paginePublic Health CareGuru KandhanNessuna valutazione finora
- Kidney Anatomy: NephronDocumento3 pagineKidney Anatomy: NephronNeil AlviarNessuna valutazione finora
- Fluid Volume BalanceDocumento73 pagineFluid Volume BalanceSalman HabeebNessuna valutazione finora
- Chest PhysiotherpypptDocumento32 pagineChest PhysiotherpypptVillain DevilNessuna valutazione finora
- Anatomy of KidneyDocumento3 pagineAnatomy of KidneyjibbyNessuna valutazione finora
- Pa Tho PhysiologyDocumento4 paginePa Tho Physiologyimagine28Nessuna valutazione finora
- Approach To Respiratory Distress in NewbornDocumento79 pagineApproach To Respiratory Distress in NewbornNikhil100% (1)
- Electrolyte Imbalance in ElderlyDocumento70 pagineElectrolyte Imbalance in ElderlyPrasannakumar P CNessuna valutazione finora
- Esophageal Atresia and Tracheoesophageal FistulaDocumento28 pagineEsophageal Atresia and Tracheoesophageal FistulaarifNessuna valutazione finora
- Effects of Preterm Birth On Bonding, A Study at KATH MBUDocumento29 pagineEffects of Preterm Birth On Bonding, A Study at KATH MBUguardy100% (1)
- Report EmpyemaDocumento32 pagineReport EmpyemaMylah CruzNessuna valutazione finora
- Fetal, Transition and Neonatal Circulation: Divya Mishra Dept of PediatricsDocumento37 pagineFetal, Transition and Neonatal Circulation: Divya Mishra Dept of PediatricsMathan KarthikNessuna valutazione finora
- Respiratory DiseasesDocumento58 pagineRespiratory DiseasesSarahNessuna valutazione finora
- Tracheo-Oesophageal FistulaDocumento23 pagineTracheo-Oesophageal FistulaAhmad KhanNessuna valutazione finora
- Prematurity: DR - Azhar Hamza AlsaqyDocumento18 paginePrematurity: DR - Azhar Hamza AlsaqyChro MANessuna valutazione finora
- ProstatitisDocumento21 pagineProstatitisHamzeAbdiMuosaNessuna valutazione finora
- Care of Child Having Bladder Exstrophy and EpispadiasDocumento3 pagineCare of Child Having Bladder Exstrophy and EpispadiasGarima ChaudharyNessuna valutazione finora
- Medscape Status EpilepticusDocumento10 pagineMedscape Status EpilepticusEllen Siska SusantiNessuna valutazione finora
- Patterns of Nursing Care Delivery in IndiaDocumento22 paginePatterns of Nursing Care Delivery in IndiaBinu JoshvaNessuna valutazione finora
- Endometri Osis: Par Khmermedical StudyDocumento18 pagineEndometri Osis: Par Khmermedical StudyLeang KarichakNessuna valutazione finora
- Amniotic Fluid & Its AbnormalitiesDocumento29 pagineAmniotic Fluid & Its AbnormalitiesSTAR Plus SerialsNessuna valutazione finora
- Pyloric StenosisDocumento2 paginePyloric Stenosisgeorgeloto12Nessuna valutazione finora
- Mal RotationDocumento13 pagineMal RotationkavyarkrnagarNessuna valutazione finora
- Rational Blood Transfusion in Infant and ChildrenDocumento37 pagineRational Blood Transfusion in Infant and ChildrenBayu KurniawanNessuna valutazione finora
- Airway Management, Ventilation, and Oxygen TherapyDocumento56 pagineAirway Management, Ventilation, and Oxygen TherapybrentupdegraffNessuna valutazione finora
- Hydranencephaly ManagementDocumento20 pagineHydranencephaly ManagementJohn Christopher LucesNessuna valutazione finora
- Anatomo-Physiological Peculiarities of The Respiratory System. Percussion of The Lungs.Documento40 pagineAnatomo-Physiological Peculiarities of The Respiratory System. Percussion of The Lungs.Hetvi PatelNessuna valutazione finora
- Suppurative Lung Diseases: DR Faisal Moidunny Mammu Department of PaediatricsDocumento39 pagineSuppurative Lung Diseases: DR Faisal Moidunny Mammu Department of PaediatricsFaisal MoidunnyNessuna valutazione finora
- Obstetric EmergenciesDocumento11 pagineObstetric EmergenciesAaronMaroonFiveNessuna valutazione finora
- Respiratory Distress Syndrome: Islamic University Nursing CollegeDocumento21 pagineRespiratory Distress Syndrome: Islamic University Nursing Collegeyaumil agisnaNessuna valutazione finora
- Akut AbdomenDocumento69 pagineAkut AbdomenFawzia Haznah Nurul ImaniNessuna valutazione finora
- Duodenal ObstructionDocumento53 pagineDuodenal ObstructionBoby ChandraNessuna valutazione finora
- Cryptomenorrhea - WikipediaDocumento6 pagineCryptomenorrhea - WikipediaScience & TechnologyNessuna valutazione finora
- Anaemia in PregnancyDocumento28 pagineAnaemia in PregnancyUsman G. HingoroNessuna valutazione finora
- NEPHROSISDocumento31 pagineNEPHROSISvinnu kalyanNessuna valutazione finora
- Assignment ON Observation ChecklistDocumento7 pagineAssignment ON Observation ChecklistParbati samantaNessuna valutazione finora
- Diabetes Mellitus Type 1Documento12 pagineDiabetes Mellitus Type 1Burhan RiazNessuna valutazione finora
- Neonatal InfectionDocumento56 pagineNeonatal InfectionGanesha Gamma 2017Nessuna valutazione finora
- Approach To Upper Gastrointestinal Bleeding in Children PDFDocumento13 pagineApproach To Upper Gastrointestinal Bleeding in Children PDFandreita1741Nessuna valutazione finora
- Partograph EditedDocumento54 paginePartograph EditedNathaniel PulidoNessuna valutazione finora
- 5 GOPT Physical Physiological ChangesDocumento40 pagine5 GOPT Physical Physiological ChangesDaniJaralNessuna valutazione finora
- 5 Bleeding Disorders PPT EditedDocumento87 pagine5 Bleeding Disorders PPT EditedFrances Isabella OlasimanNessuna valutazione finora
- FMRI Obs Icu & HduDocumento13 pagineFMRI Obs Icu & HduApoorv JainNessuna valutazione finora
- TN Fahrudin Vulnus ExcoriatumDocumento10 pagineTN Fahrudin Vulnus Excoriatummonyet65Nessuna valutazione finora
- A Comparative Study of Nutritional Status of Children Aged 11-14 Years of Low and High Economical Background, SuratDocumento4 pagineA Comparative Study of Nutritional Status of Children Aged 11-14 Years of Low and High Economical Background, SuratEditor IJTSRDNessuna valutazione finora
- Muscle Function TestingDocumento2 pagineMuscle Function TestingAnonymous OAEuN9NE1sNessuna valutazione finora
- CL12Documento598 pagineCL12preeti dNessuna valutazione finora
- Kitchen Chemistry: A Scoping Review of The Diversionary Use of Pharmaceuticals For Non-Medicinal Use and Home Production of Drug SolutionsDocumento10 pagineKitchen Chemistry: A Scoping Review of The Diversionary Use of Pharmaceuticals For Non-Medicinal Use and Home Production of Drug SolutionsAntonioNessuna valutazione finora
- Poundmaker's Lodge Treatment Centres Press ReleaseDocumento1 paginaPoundmaker's Lodge Treatment Centres Press ReleaseCTV News EdmontonNessuna valutazione finora
- 2023 Vein AnatomyDocumento6 pagine2023 Vein AnatomyKarenNessuna valutazione finora
- Sample Pipe Jacking Engineer ResumeDocumento9 pagineSample Pipe Jacking Engineer ResumeGeorge VNessuna valutazione finora
- Wound Care DescriptionDocumento4 pagineWound Care DescriptionRodriguez, Joyce Ann G.Nessuna valutazione finora
- ASD Interventions Theories, Age Range and SettingsDocumento4 pagineASD Interventions Theories, Age Range and SettingstracycwNessuna valutazione finora
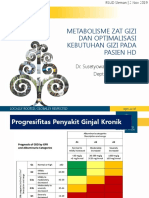
- Seminar HD-RSUD Sleman 2019Documento36 pagineSeminar HD-RSUD Sleman 2019herkamaya100% (1)
- Respiration Course ObjectivesDocumento8 pagineRespiration Course Objectivesjoshy220996Nessuna valutazione finora
- Prevention of Crown and Root Caries in AdultsDocumento19 paginePrevention of Crown and Root Caries in AdultsnataliaNessuna valutazione finora
- Lactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonDocumento15 pagineLactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonArrianne AcopNessuna valutazione finora
- Makalah Bahasa InggrisDocumento7 pagineMakalah Bahasa InggrisRima Novianti100% (1)
- ILS 2014 Final Year Revision LectureDocumento54 pagineILS 2014 Final Year Revision LectureokaberntrNessuna valutazione finora
- JONES Criteria: Rheumatic FeverDocumento5 pagineJONES Criteria: Rheumatic FeverChristopher GarrettNessuna valutazione finora
- New Cystic Fibrosis Diagnosis FinalDocumento26 pagineNew Cystic Fibrosis Diagnosis FinalSuman DeshmukhNessuna valutazione finora
- HIV Policy MemoDocumento3 pagineHIV Policy MemoZhihong XuNessuna valutazione finora