Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Concept Map - TCC - Longterm Care
Caricato da
Stacy StrongDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Concept Map - TCC - Longterm Care
Caricato da
Stacy StrongCopyright:
Formati disponibili
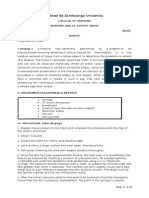
Associate Degree Nursing Program Concept MapStep 4 & 5 Problem #1: Chronic Pain General Goal: Pt will verbalize
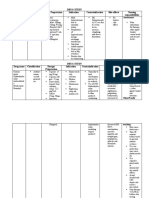
and demonstrate (non-verbal cues) relief and/or control of pain or discomfort Predicted Behavioral Outcome Objective(s): Pt will demonstrate comfort and willingness that will identify specific pain level that will allow her to perform ADLs, and pain will stay below the specific lever for remainder of cancer progression. Nursing Strategies Patient Responses 1. Assess the conditions associated with long-term Pt has - Stage l L heel pressure ulcer; Stage III R Heel pain Pressure Ulcer, Sacrococcygeal Stage l Pressure Ulcer, Bilateral knee arthroplasty, Symptoms of splenomegaly, Noeplastic Malignant Ovarian Cancer, Osteoarthritis 2. Evaluate current and past analgesic, opioid or other Pt is allergic to Codiene, PCN, Morphine, Percocet drug use 5/325; alleged reaction is unknown. Pt is prescribed Tylenol for pain and fever; when offered Tylenol for pain control pt declined for fear that it would react with her Coumadin treatment. 3. Evaluate pain behaviors Pt appears to be in severe pain, she is reluctant to her prescribed care. She exhibits facial grimacing, her body is tense and rigid, she winces to the touch and is guarded when attempts were made to assess her abdomen and lower extremities. 4. Assist client in minimizing effects of pain on PT/OT/ST and OT is ordered on a daily basis there is no interpersonal relationships and daily activities prescribed pain management other than Tylenol. Pt is resistant to therapy she cries out in pain and is guarded. In transfer from bed to wheelchair via Hoyer lift pt states, "I don't want that it hurts." PT was scheduled during breakfast. Pt was force to top eating to perform ROM exercise. 5. Watch for signs of depression with chronic pain; Pt is difficult to arouse. Nurse states, that she sleeps sleepiness, not eating, flat effect, statements of throughout the day if not performing ADL's and depression, or suicidal ideation exercises with therapy. Pt has flat facial expression and cries out when moved or manipulated. Summarize patient progress toward outcome objectives: Pt pain is not control and need further evaluation from her physician or pain management center. She needs further education based on the prescribed medication. PT/OT and ST needs to be scheduled around breakfast and lunch.
Problem #2: Disturbed Sensory Perception at Risk For Prone Health Behavior General Goal: Predicted Behavioral Outcome Objective(s): Pt will recognize and correct or compensate for sensory impairments by demonstrating an increasing interest/participation in self-care Nursing Strategies Patient Responses 1. Perform a physical and/or psychological Pt is difficult to arouse. Nurse states, that she sleeps assessment throughout the day if not performing ADL's and exercises with therapy. Pt has flat facial expression and cries out when moved or manipulated. Pt is guarded and reluctant to be assessed, asks "why and would prefer to left alone" Pt refuses to allow assessment of her abdomen and L lower extremity. 2. Explore the expression of emotion signifying Pt has flat facial effect, cries out when moved or impaired adjustment manipulated. Pt is guarded and reluctant to perform ADLs and Therapy. Pt's states, "I am unable to hear you and cannot understand you." And "I am not going to answer you." 3. Use therapeutic communication skills Discussed the reason for care and therapy, offered open communication and feedback. Expressed that I would like to help her remain comfortable and safe. 4. Assess the ability to speak, hear, interpret and Pt had decreased vision and hearing loss. She has respond to simple commands. corrective lenses and hearing aids. CNA stated that she refused to wear her hearing aids. Pt states that, "They block her hearing" 5. Observe for behavioral response and encourage Pt is encouraged to wear her hearing aids. Pt is the use of listening device reluctant and states that, "They block her hearing" When she wears her hearing aids communication improves. Summarize patient progress toward outcome objectives: Need to re-evaluate interventions and contributing factors such as pain. Continue to encourage self-care and positive reinforcement. Provide patient with option for care, such as time, days and interventions to help maintain pt autonomy and control over self.
Problem #3: Ineffective Peripheral Tissue Perfusion At Risk For Infection General Goal: Pt will remain free of infection Predicted Behavioral Outcome Objective(s): The client will demonstrate progressive healing of tissue, as evi-denced by the Granulating and epithelizing wounds with low to moderate amounts of exudates with approximated edges. Wounds will be kept clean and dry. Wound will be monitored for signs of infection, oral temperature will remain between 96.8 - 99.9 F (37 - 37.7C) daily Nursing Strategies Patient Responses 1. Note the current condition that can effect Pt. is insulin dependent diabetic, Hypertension, CHF, perfusion to all body systems ovarian cancer, immobility and pressure ulcers 2. Assess the skin texture, presence of edema, Pts skin is dry and fragile; slight tenting present; peripheral pulses and cap refill. Peripheral pulses are palpable and cap refill <3 sec bilaterally pedialas. Slight non-pitting edema bilateral lower extremities. Pt has a stage l pressure ulcer R-heel and sacrococcygeal area and stage ll pressure ulcer L heel 3. Observe wound for Redness, swelling, increased R-heel -Intact skin, nonblanchable erythema, painful to pain, or purulent drainage touch, soft, and warm. Sacrococcygeal area - Intact skin; nonblanchable erythema, painful to touch, soft, and warm. L -heel - superficial nonblanchable blackened tissues, 6 cm, painful to touch. 4. Monitor vitals signs - temp, pulse, respiration, BP - 168/80; Radial Pulse - 91; RR - 20; Temp - Pt auscultate lungs for crackles or rhonchi refused. Lung fields, clear breath sounds on auscultation 5. Monitor white blood count (WBC). Lab draw -1/21/13 WBC's were elevated at 17.8. 6. Administer antibiotic medication as prescribed Pt is prescribed flagyl TID at 0800, 1400 and 2000 and Levaquin daily at 0800 as an anti-infective; flagyl and levaquin given at 0800 this shift Summarize patient progress toward outcome objectives: OT states, that the pressure ulcers are responding to current antibiotic treatment and therapies. Pt exhibits reluctance to therapy related to pain. Reassess pain management therapy.
Problem #4: Impaired Physical Mobility / Self-Care Deficit At Risk For Falls General Goal: Maintain or increase strength and function of affected and/or compensatory body part Predicted Behavioral Outcome Objective(s): Pt will demonstrate understanding of situation and individual treatment regimen and safety as evidence by comfort and willingness to participate in self-care. Nursing Strategies Patient Responses 1. Determine extent of immobility Pt is immobile due to pressure ulcers on bilateral heels. She is bed and wheel chair bound; Hoyer lift prescribed for transfer. 2. Assess the degree of pain Pts is flat facial effect, body is rigid with limited movement while at rest. Pt grimaces and cries out; she is guarded and tense during physical assessment, OT , ST and PT. 3. Assess pt perception of activity and exercise needs Pt is reluctant to participate in prescribed therapy. She exhibits no-verbal signs of discomfort, such as facial grimacing, guarded, winces to touch. 4. Determine presence of complications R/T Pt has bilateral clear breath sounds on auscultation, immobility capillary refill is <3 sec bilaterally upper and lower extremities, exhibits bilateral slight non-pitting edema in her ankles; bilateral heel pressure ulcers and nonverbal indications of pain. 5. Reposition q2h Pt is reposition and comfort assessment provided Q2h 6. Support affected body parts or joints using pillow, Pt is positioned with air boots bilaterally to prevent rolls, foot support or shoes. pressure on heels while in bed. Summarize patient progress toward outcome objectives: OT, PT and ST are order daily to prevent further complications. Pt joints remain without contracture, passive ROM, grip strength equal and but weak; Fine motor skills are limited; Able to eat and drink with no assistance; needs assistance with repositioning Pt is reluctant to care due to her pain level. Reassess pain management. Adapted from Schuster, P.M. (2002) Concept Mapping: A Critical Thinking Approach to Care Planning. Used with permission. (Rev 12/11)
Potrebbero piacerti anche
- Pediatric EmergenciesDocumento79 paginePediatric Emergenciesأحمد سعد الديوه جيNessuna valutazione finora
- GROUP 3 - CASE STUDY - TraumaDocumento5 pagineGROUP 3 - CASE STUDY - TraumaDinarkram Rabreca EculNessuna valutazione finora
- StrokeDocumento1 paginaStrokeMariel Febreo MerlanNessuna valutazione finora
- Neurology Lectures 1 5 DR - Rabo 2Documento20 pagineNeurology Lectures 1 5 DR - Rabo 2Miguel Cuevas DolotNessuna valutazione finora
- Third Molar Surgical Difficulty Scales: Systematic Review and Preoperative Assessment FormDocumento9 pagineThird Molar Surgical Difficulty Scales: Systematic Review and Preoperative Assessment FormdaruNessuna valutazione finora
- Case Analysis On Respiratory DisordersDocumento5 pagineCase Analysis On Respiratory DisordersAaron ConstantinoNessuna valutazione finora
- Unit 2 HEALTH MAPEH 10Documento5 pagineUnit 2 HEALTH MAPEH 10Aj AntonioNessuna valutazione finora
- Ethical Issues in Geriatrics A Guide For CliniciansDocumento9 pagineEthical Issues in Geriatrics A Guide For CliniciansThanc FishNessuna valutazione finora
- Discharge PlanDocumento5 pagineDischarge PlanrraksNessuna valutazione finora
- The Child With Hematologic DisordersDocumento149 pagineThe Child With Hematologic DisordersNics FranciscoNessuna valutazione finora
- PM PFC MatrixDocumento4 paginePM PFC MatrixFamed residentsNessuna valutazione finora
- Bowel ObstructionDocumento6 pagineBowel ObstructionKryza Dale Bunado BaticanNessuna valutazione finora
- 1 A Synopsis of IVT in The PhilippinesDocumento17 pagine1 A Synopsis of IVT in The PhilippinesPrince Rener Velasco PeraNessuna valutazione finora
- ConceptMap AMLDocumento1 paginaConceptMap AMLnursing concept mapsNessuna valutazione finora
- Concept Map FinalDocumento1 paginaConcept Map Finalapi-383763177Nessuna valutazione finora
- Pituitary Adenoma Concept MapDocumento1 paginaPituitary Adenoma Concept Mapnursing concept mapsNessuna valutazione finora
- Lung Cancer ScreeningDocumento17 pagineLung Cancer ScreeningNguyen Minh DucNessuna valutazione finora
- Ateneo de Zamboanga University: College of Nursing Nursing Skills Output (Nso) Week Biopsy I. DescritptionDocumento4 pagineAteneo de Zamboanga University: College of Nursing Nursing Skills Output (Nso) Week Biopsy I. DescritptionHaifi HunNessuna valutazione finora
- Concept For Abdominal BloatingDocumento1 paginaConcept For Abdominal BloatingChiomaDabrinze-AmosNwankwoNessuna valutazione finora
- GBS Nursing MangementDocumento21 pagineGBS Nursing MangementJoseph Namita SunnyNessuna valutazione finora
- Concept Map For EndocarditisDocumento3 pagineConcept Map For EndocarditisSavanna ChambersNessuna valutazione finora
- Cancer Concept MapDocumento1 paginaCancer Concept MapNICOLE ALLYSA M. BALBERANNessuna valutazione finora
- Crizotinib Improves ProgressionDocumento3 pagineCrizotinib Improves ProgressionIsabella RoselliniNessuna valutazione finora
- Acute Concept Map 2 FinalDocumento1 paginaAcute Concept Map 2 FinalCynthia LeonNessuna valutazione finora
- Burns Pathophysiology 2Documento1 paginaBurns Pathophysiology 2Monique Ann DanoyNessuna valutazione finora
- Understanding Traumatic Brain InjuryDocumento43 pagineUnderstanding Traumatic Brain InjurySilvanaPutriNessuna valutazione finora
- Concept MapDocumento3 pagineConcept Mapphelenaphie menodiado panlilioNessuna valutazione finora
- Concept Map 1Documento2 pagineConcept Map 1yfortilus100% (1)
- Ineffective Peripheral Tissue Profusion Care PlanDocumento1 paginaIneffective Peripheral Tissue Profusion Care Planstacie4roher4smithNessuna valutazione finora
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Interevention Rationale EvaluationDocumento1 paginaNovilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNessuna valutazione finora
- Week 7 - Rheumatoid ArthritisDocumento1 paginaWeek 7 - Rheumatoid ArthritisTuTitNessuna valutazione finora
- Concept MapDocumento1 paginaConcept Mapapi-252910411Nessuna valutazione finora
- Module D Pain AssessmentDocumento12 pagineModule D Pain Assessmentmwhite8051100% (1)
- Deficient Fluid Volume: Assessment Nursing DiagnosisDocumento7 pagineDeficient Fluid Volume: Assessment Nursing DiagnosisJasonlee BaluyotNessuna valutazione finora
- Concept Map Meningitis TheoryDocumento3 pagineConcept Map Meningitis TheoryMia AuliaNessuna valutazione finora
- CKD + HPN Concept Map DRAFTDocumento1 paginaCKD + HPN Concept Map DRAFTInah Floresta BesasNessuna valutazione finora
- Physical RestraintsDocumento4 paginePhysical RestraintsSathya PalanisamyNessuna valutazione finora
- Nursing Care Plan For Subarachnoid HemorrhagicDocumento2 pagineNursing Care Plan For Subarachnoid HemorrhagicAshram Smart100% (1)
- Cushings SyndromeDocumento51 pagineCushings SyndromeTina TalmadgeNessuna valutazione finora
- PoliomyelitisDocumento4 paginePoliomyelitisGerard Adad Misa100% (1)
- Head InjuryDocumento2 pagineHead InjuryPheiyi WongNessuna valutazione finora
- NCP DIarrheaDocumento8 pagineNCP DIarrheakamini ChoudharyNessuna valutazione finora
- Classification of Burns Based On Depth CharacteristicsDocumento2 pagineClassification of Burns Based On Depth CharacteristicsmexelleNessuna valutazione finora
- Hip FractureDocumento3 pagineHip Fracturenursing concept mapsNessuna valutazione finora
- Case Scenarios: Scenario 1Documento2 pagineCase Scenarios: Scenario 1Kym RonquilloNessuna valutazione finora
- Concept MapDocumento6 pagineConcept Mapapi-499028250Nessuna valutazione finora
- A. A Sudden Change in How Brain Cells Send Electrical Signals To One AnotherDocumento70 pagineA. A Sudden Change in How Brain Cells Send Electrical Signals To One AnotherMwansaay Twain HolyNessuna valutazione finora
- Inv A Sion Pha Se: Bill Julius Samuel G. Alferez BSN IiiDocumento1 paginaInv A Sion Pha Se: Bill Julius Samuel G. Alferez BSN IiiRudelsa Agcolicol LangamanNessuna valutazione finora
- Oxytocin (Pitocin) : Slide 1Documento16 pagineOxytocin (Pitocin) : Slide 1Kalesha JonesNessuna valutazione finora
- Assignmen 1 AnswersDocumento3 pagineAssignmen 1 AnswersAlasl BobyNessuna valutazione finora
- BiopsyDocumento4 pagineBiopsyanirbanmanna88320Nessuna valutazione finora
- NCP DisturbedDocumento2 pagineNCP DisturbedTrixie Anne GamotinNessuna valutazione finora
- Pathophysiology of PsoriasisDocumento2 paginePathophysiology of PsoriasisKim LegastoNessuna valutazione finora
- Check ListDocumento11 pagineCheck ListtetarwalNessuna valutazione finora
- Nursing Care Plan For HEMOTHORAX PNEUMOTHORAXDocumento8 pagineNursing Care Plan For HEMOTHORAX PNEUMOTHORAXHistory TechNessuna valutazione finora
- Bacterial Pneumonia PharmacologyDocumento70 pagineBacterial Pneumonia PharmacologyMarc Imhotep Cray, M.D.Nessuna valutazione finora
- SBAR ToolDocumento2 pagineSBAR Toolpragya_devkota0% (1)
- This Study Resource Was Shared Via: HypoparathyroidismDocumento1 paginaThis Study Resource Was Shared Via: HypoparathyroidismDeo FactuarNessuna valutazione finora
- Kaposi's SarcomaDocumento6 pagineKaposi's SarcomaveremkovichNessuna valutazione finora
- Or Technique Scrubbing, Gowning and Arranging Instruments: 1. Define The Following Terms: Peri - Operative NursingDocumento35 pagineOr Technique Scrubbing, Gowning and Arranging Instruments: 1. Define The Following Terms: Peri - Operative NursingHoney MacabuhayNessuna valutazione finora
- Drug Study Drug Name Classificatio N Dosage/ Prepatarion Indication Contraindication Side Effects Nursing ResponsibilitiesDocumento4 pagineDrug Study Drug Name Classificatio N Dosage/ Prepatarion Indication Contraindication Side Effects Nursing ResponsibilitiesTheresa AbrilloNessuna valutazione finora
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDa EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNessuna valutazione finora
- Report AyendeDocumento13 pagineReport AyendeAbubakar RabiuNessuna valutazione finora
- DWIHN Access To HealthcareDocumento1 paginaDWIHN Access To HealthcareWXYZ-TV Channel 7 DetroitNessuna valutazione finora
- Comminuted Fractures in Dogs - Symptoms, Causes, Diagnosis, Treatment, Recovery, Management, CostDocumento7 pagineComminuted Fractures in Dogs - Symptoms, Causes, Diagnosis, Treatment, Recovery, Management, Costclips and chipsNessuna valutazione finora
- Pregestational ConditionsDocumento66 paginePregestational ConditionsEsvinch EsvinchNessuna valutazione finora
- Addiction - Substance AbuseDocumento30 pagineAddiction - Substance AbusemidoNessuna valutazione finora
- Preconception Health in The Well WomanDocumento9 paginePreconception Health in The Well WomanI Tech Services KamranNessuna valutazione finora
- CV RUGS Format TZMTJ 18022014Documento6 pagineCV RUGS Format TZMTJ 18022014Nor LiyanaNessuna valutazione finora
- AVILA, Decision Making For Tooth Extraction or ConservationDocumento17 pagineAVILA, Decision Making For Tooth Extraction or ConservationKathe LeyvaNessuna valutazione finora
- A Call To Reexamine Quality of Life Through Relationship-Based FeedingDocumento7 pagineA Call To Reexamine Quality of Life Through Relationship-Based FeedingLauraNessuna valutazione finora
- The Managed Care LandscapeDocumento30 pagineThe Managed Care LandscapeJohnNessuna valutazione finora
- Nursing Informatics: Master of Arts in NursingDocumento3 pagineNursing Informatics: Master of Arts in NursingMaica LectanaNessuna valutazione finora
- Julia Harwood Promoted To Senior Vice President of Clinical Operations For New York Cancer & Blood SpecialistsDocumento3 pagineJulia Harwood Promoted To Senior Vice President of Clinical Operations For New York Cancer & Blood SpecialistsPR.comNessuna valutazione finora
- Fields of NursingDocumento8 pagineFields of NursingOmie TumanguilNessuna valutazione finora
- Add Risk Min MeasDocumento12 pagineAdd Risk Min MeasVladimir KostovskiNessuna valutazione finora
- Career ReportDocumento7 pagineCareer ReportRyan KillNessuna valutazione finora
- Pressure Ulcers Project - EditedDocumento6 paginePressure Ulcers Project - EditedZeera MohamadNessuna valutazione finora
- Vacant Seats For Transfer - Admissions 2022Documento4 pagineVacant Seats For Transfer - Admissions 2022Shahroz RindNessuna valutazione finora
- The International Research Congress On Integrative Medicine and Health 2014Documento159 pagineThe International Research Congress On Integrative Medicine and Health 2014Sergio Jesús Huapaya GálvezNessuna valutazione finora
- FKIK DikonversiDocumento119 pagineFKIK DikonversiIera TajudinNessuna valutazione finora
- DM MCHDocumento2 pagineDM MCHBhalodiya NirajNessuna valutazione finora
- Pharmacy Act - 1948Documento49 paginePharmacy Act - 1948Manu GargNessuna valutazione finora
- Update Journal Reading Stase BedahDocumento24 pagineUpdate Journal Reading Stase BedahadnajaniNessuna valutazione finora
- What Need Know About Wild OreganoDocumento21 pagineWhat Need Know About Wild OreganoMatt PintoNessuna valutazione finora
- Dr. Noel Casumpang vs. Cortejo G.R. No. 171127, March 11, 2015Documento29 pagineDr. Noel Casumpang vs. Cortejo G.R. No. 171127, March 11, 2015FD BalitaNessuna valutazione finora
- Hospital List in SADocumento26 pagineHospital List in SASudhakar KuppireddyNessuna valutazione finora