Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Clinical Aspects of Tonsillar Tuberculosis
Caricato da
Weleh Weleh WatiCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Clinical Aspects of Tonsillar Tuberculosis
Caricato da
Weleh Weleh WatiCopyright:
Formati disponibili
TONSILLAR TUBERCULOSIS
CLINICAL ASPECTS OF TONSILLAR TUBERCULOSIS
Somchai Srirompotong, Kwanchanok Yimtae and Supaporn Srirompotong Department of Otolaryngology, Faculty of Medicine, Srinagarind Hospital, Khon Kaen University, Khon Kaen, Thailand
Abstract. A clinical analysis of 6 patients with pathologically confirmed tonsillar tuberculosis was carried out retrospectively. The subjects comprised three men and three women, ranging in age from 20 to 74 years. All of the patients presented with a sore throat and 5 had lymphadenopathy. Ulcerations, masses and white patches characterized the tonsillar lesions; the pathological findings included caseous granuloma with positive acid-fast bacilli (AFB) in 5 patients and chronic granulomatous inflammation with negative AFB in one patient. Four of the six patients had pulmonary tuberculosis. The three patients who received complete treatment responded well. The presenting symptoms and abnormal tonsillar findings associated with tonsillar tuberculosis are similar to those of malignant tumors and therefore it is difficult to differentiate the two pathologies; moreover, tonsillar tuberculosis often occurs with pulmonary tuberculosis and AIDS and therefore, a chest X-ray and HIV-screening are recommended for all patients with tonsillar tuberculosis.
INTRODUCTION Prior to the introduction of chemotherapy, 6.5% of all tonsils removed from asymptomatic patients were infected with tubercles (Thompson, 1919). The tonsils were usually infected with Mycobacterium bovis because the patients drank infected cows milk. With the advent of effective antituberculosis therapy and the pasteurization of cows milk, a considerable reduction in the worldwide prevalence of tuberculosis was achieved (Anim and Dawlatty, 1991) and related tonsillar tuberculosis became rare (Williams and Douglas, 1995). For example, Rohwedder (1974) documented only 16 cases of tuberculosis of the upper respiratory tract among 843 cases of pulmonary tuberculosis. Similarly, isolated pharyngeal lesions affecting the nasopharynx or palatine tonsils, without accompanying pulmonary disease, is infrequent (Cleary and Batsakis, 1995; Selimoglu et al, 1995). The purpose of our
Correspondence: Somchai Srirompotong, Department of Otolaryngology, Faculty of Medicine, Srinagarind Hospital, Khon Kaen University, Khon Kaen 40002, Thailand. Tel: 66-43-348396; Fax: 66-43-243336 Email:srirompotong@yahoo.com Vol 33 No. 1 March 2002
study was to present the clinical manifestations of tonsillar tuberculosis.
MATERIAL AND METHODS We reviewed the pathological database records at Srinagarind Hospital, Faculty of Medicine, Khon Kaen University, Thailand, of patients with tonsillar tuberculosis seen between January 1991 and December 2000. Data were retrieved on age, presenting symptoms, characteristic lesions of the tonsils, histological findings, HIV infection, response to therapy and evidence of concomitant tuberculosis infection of other organs. Of the 7 cases fitting our criterion, one was excluded because the records were incomplete.
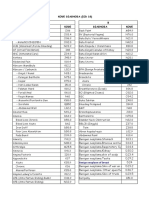
RESULTS The clinical features of the six patients (3 men and 3 women) are shown in Table 1. Age averaged 41.6 years, ranging from 20 to 74 years. The presenting symptoms included: sore throat (6/6), cervical lymphadenopathy (5/ 6), constitutional symptoms of malaise, fever, and/or weight loss (2/6) and cough (1/6).
147
SOUTHEAST ASIAN J TROP MED PUBLIC HEALTH
Table 1 Tonsillar tuberculosis : clinical features.
Case Age/sex Clinical features Sore throat c. node Duration (months) 2 Tonsillar appearance Mass Chest X-ray Tonsillar biopsy Caseous Granulomatous AFB +ve Caseous Granulomatous AFB +ve Caseous Granulomatous AFB +ve
20/M
Active tuberculosis sputum AFB -ve Not done
35/F
Sore throat cough c. node, fever Sore throat
White patch
74/M
12
Ulceration
Active tuberculosis sputum AFB -ve
37/F
Sore throat fever c. node Sore throat c. node
Ulceration
Active Caseous tuberculosis Granulomatous sputum AFB +ve AFB +ve Active tuberculosis sputum AFB -ve Not done Caseous Granulomatous AFB +ve Chronic Granulomatous AFB -ve
20/M
Ulceration
64/F
Sore throat c. node
Mass
c. node = cervical node enlargement
Four of the five patients with cervical lymphadenopathy had multiple bilateral lymph node enlargement; only one patient had isolated posterior cervical lymphadenopathy. The nodes were mostly of the middle cervical group (in 4 patients) and the posterior cervical group (in 2 patients). The various tonsillar findings included: ulceration (3 of 6 patients), masses (2/6) and white patches (1/6). The histological findings were described as caseous granulomatous lesions with positive acid-fast bacilli (AFB) in 5 patients and chronic granulomatous inflammation with negative AFB in one patient. Chest X-rays provided clear evidence of pulmonary tuberculosis, although, only 4 of the 6 patients had X-rays. Sputum AFB was positive in only one of those with a positive
148
chest X-ray. One patient had negative sputum AFB despite having miliary infiltration of the right upper lung with minimal pleural effusion. This patient had tonsillar masses and ulceration of the nasopharynx. Histological findings of the tonsil and nasopharynx included caseous granulomatous lesions with positive AFB. Three patients were tested serologically for HIV infection: the tests were negative. Three patients received standard full-length antituberculosis treatment, which consisted of 2 months of isoniazid, rifampicin, ethambuthol and pyrazinamide followed by 4 months of isoniazid and rifampicin. All patients responded to the first two months of treatment, as shown by a reduction in the size of the cervical lymph nodes and the disappearance of tonsillar leVol 33 No. 1 March 2002
TONSILLAR TUBERCULOSIS
sions. Those who received the full course of chemotherapy showed complete resolution of cervical lymphadenopathy and tonsillar lesions. Three patients completed only 3 months of treatment and thereafter contact with them was lost. DISCUSSION Tuberculosis is regarded as the most common communicable disease worldwide (Robbins and Cotran, 1979). After the introduction of antituberculous therapy and immunization, the incidence of tuberculous infection declined dramatically (Adiego et al, 1994). The upper respiratory tract is generally resistant to tuberculosis, perhaps because saliva has an inhibitory effect on tubercle bacilli (Verma et al, 1989). In our study, the most common presenting symptom of tonsillar tuberculosis was a sore throat. The abnormalities of the tonsils found - such as ulceration, mass, or white patches are not easily differentiated from similar abnormalities seen in tonsillar carcinomas. Differential diagnoses of oral and pharyngeal tuberculosis includes traumatic ulcers, aphthous ulcer, Plaut-Vincents tonsillitis, hematological disorders, actinomycosis, syphilis, midline granuloma, Wegeners disease and carcinoma (Adiego et al, 1994; Williams and Douglas, 1995; Selimoglu et al, 1995). To establish a definitive diagnosis a biopsy of tonsil tissue is mandatory. Primary tuberculous infections of tonsils are rare (Selimoglu et al, 1995): and in our study those who underwent chest X-rays had pulmonary tuberculosis and one also had nasopharyngeal tuberculosis. Tuberculosis tends to present in atypical forms, and extrapulmonary localizations are common in patients with a poor immune response eg alcoholics and those with HIV infections (Sunderam et al, 1986; Chaisson et al, 1987; Pedrol et al, 1989; Adiego et al, 1994). In our study, three patients were screened for HIV infection but the results were negative.
Vol 33 No. 1 March 2002
A larger sample might have demonstrated the association of tonsillar tuberculosis with HIV infection. Tonsillar tuberculosis responds well to treatment with antituberculous drugs (Selimoglu et al, 1995). The three patients who underwent complete treatment experienced total resolution of tonsillar lesions and cervical lymphanopathy. CONCLUSION Tonsillar tuberculosis commonly presents with a sore throat and cervical lymphadenopathy. This presentations, as well as the common abnormal tonsillar findings, make it difficult to differentiate tonsillar tuberculosis from a malignant tumor. Four of our six patients had secondary tonsillar tuberculosis from a pulmonary source and one of these patients also had nasopharyngeal tuberculosis Since AIDS patients are prone to mycobacterial infection and an increased number of extrapulmonary tuberculous infections, we recommend that a chest X-ray and HIV-screening should be conducted whenever a patient is diagnosed with tonsillar tuberculosis.
ACKNOWLEDGEMENTS We thank Mr Bryan Roderick Hamman for his assistance with the English-language presentation of the paper.
REFERENCES
Adiego MI, Million J, Royo J, et al. Unusual association of secondary tonsillar and cerebral tuberculosis. J Laryngol Otol 1994; 108: 348-9. Anim JT, Dawlatly EE. Tuberculosis of the tonsil revisited. West Afr J Med 1991; 10: 194-7. Chaisson RE, Schecter GF, Theuer CP, et al. Tuberculosis in patients with acquired immunodeficiency syndrome. Am Rev Respir Dis 1987; 136: 570-4. 149
SOUTHEAST ASIAN J TROP MED PUBLIC HEALTH Cleary K, Batsakis JG. Mycobacterial disease of the head and neck: current perspective. Ann Otol Rhinol Laryngol 1995; 104: 830-3. Pedrol E, Estruck R, Barcelo, et al. Tonsillar and pharyngeal tuberculosis in patients without HIV antibodies. J Infect Dis 1989; 159: 598. Robbins SL, Cotran RS. Pathologic basis of disease. Philadelphia: WB Saunders, 1979: 396-7. Rohwedder J. Upper respiratory tract tuberculosis. Sixteen cases in a general hospital. Ann Intern Med 1974; 80: 708-13. Selimoglu E, Sutbeyaz Y, Ciftcioglu A, et al. Primary tonsillar tuberculosis: a case report. J Laryngol Otol 1995; 109: 880-2. Sunderam G, McDonald RJ, Maniatis T, et al. Tuberculosis as a manifestation of the acquired immunodeficiency syndrome (AIDS). J Am Med Assoc 1986; 256: 362-6. Thomson SC. Disease of the nose and throat, 2nd ed. London: Cassell 1919: 632-54. Verma A, Mann SBS, Randotra B. Primary tuberculosis of tongue. Ear Nose Throat J 1989; 68: 719-20. Williams RG, Douglas JT. Mycobacterium marches back. J Laryngol Otol 1995; 109: 5-13.
150
Vol 33 No. 1 March 2002
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Faraz Pearls For MRCPDocumento223 pagineFaraz Pearls For MRCPSyed Ali Akbar86% (14)
- Diagnosa Icd 10 SilDocumento51 pagineDiagnosa Icd 10 SilinayaNessuna valutazione finora
- STI in PregnancyDocumento49 pagineSTI in PregnancynabilaNessuna valutazione finora
- Gestational Diabetes Mellitus (GDM)Documento26 pagineGestational Diabetes Mellitus (GDM)Chrizzia Del RosarioNessuna valutazione finora
- John Hopkins ForwardDocumento603 pagineJohn Hopkins ForwardAliefia Ditha K100% (1)
- Physical Therapy AbbreviationsDocumento2 paginePhysical Therapy Abbreviationspearl042008100% (1)
- Neonatal Emergencies FinalDocumento90 pagineNeonatal Emergencies FinalDr Raseena VattamkandathilNessuna valutazione finora
- Niemann Pick DiseaseDocumento3 pagineNiemann Pick Diseaseडा. सत्यदेव त्यागी आर्यNessuna valutazione finora
- Ilovepdf MergedDocumento45 pagineIlovepdf Mergedacte minophenNessuna valutazione finora
- Ijam 1Documento5 pagineIjam 1Chakradhar ChakrreNessuna valutazione finora
- Valencia Baribar Global Health InitiativesDocumento17 pagineValencia Baribar Global Health InitiativesKrisha Tañare-MalateNessuna valutazione finora
- Introductionto Community MedicineDocumento151 pagineIntroductionto Community MedicineHibaaq AhmedNessuna valutazione finora
- Bovine Tuberculosis: The Role of BadgersDocumento5 pagineBovine Tuberculosis: The Role of BadgerspranalinshahNessuna valutazione finora
- Suicide and Mental Health Problems in Men in PolandDocumento6 pagineSuicide and Mental Health Problems in Men in PolandNatalia Alva ZavalaNessuna valutazione finora
- Jurnal Tinea Unguium - 1Documento6 pagineJurnal Tinea Unguium - 1FazaKhilwanAmnaNessuna valutazione finora
- Fecal Calprotectin in IBDDocumento34 pagineFecal Calprotectin in IBDNathania Nadia Budiman100% (1)
- Hexyon LeafletDocumento49 pagineHexyon LeafletEllaNessuna valutazione finora
- DM Type 2Documento153 pagineDM Type 2Taufiqurrochman Nur AminNessuna valutazione finora
- NKOM Self Declaration Form Rev-07Documento1 paginaNKOM Self Declaration Form Rev-07Adrian Cantaragiu100% (1)
- Biochemical and Clinical Profile of With Diabetic Ketoacidosis: A Single Centre ExperienceDocumento1 paginaBiochemical and Clinical Profile of With Diabetic Ketoacidosis: A Single Centre ExperienceBianca ChiriacNessuna valutazione finora
- G7 Health Q4 W1 - Non-CommunicableDocumento17 pagineG7 Health Q4 W1 - Non-CommunicableLeonora P AtienzaNessuna valutazione finora
- How We Can Spread AwerenessDocumento47 pagineHow We Can Spread AwerenessFaurel AzmiNessuna valutazione finora
- 15 - Consumption of Fish and n-3 Fatty Acids and Risk of Incident Alzheimer Disease - PubMedDocumento2 pagine15 - Consumption of Fish and n-3 Fatty Acids and Risk of Incident Alzheimer Disease - PubMedNaïs LABBADINessuna valutazione finora
- Xavier University Ateneo de Cagayan College of Nursing: Flaviviridae GenusDocumento4 pagineXavier University Ateneo de Cagayan College of Nursing: Flaviviridae GenusYhen CapistranoNessuna valutazione finora
- M1 Intro To Disease IntroDocumento35 pagineM1 Intro To Disease IntrorealforgiveNessuna valutazione finora
- Swine DiseaseDocumento38 pagineSwine DiseasehapipillyelloNessuna valutazione finora
- AppendicitisDocumento5 pagineAppendicitisaiNessuna valutazione finora
- Acute Leukemia ProtocolDocumento13 pagineAcute Leukemia ProtocolBol Dhalbeny MalualNessuna valutazione finora
- Dr. NandaDocumento28 pagineDr. NandaAlban RamadhanNessuna valutazione finora
- Weekly Epi Update 79Documento19 pagineWeekly Epi Update 79Lee Ji EunNessuna valutazione finora