Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Daily NCP
Caricato da
Kuennie SabalCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Daily NCP
Caricato da
Kuennie SabalCopyright:
Formati disponibili
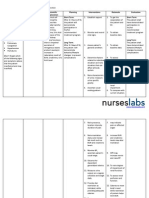
Room: 305 Diagnosis: PTB III, Diabetes Mellitus Type II (uncontrolled) NURSING DIAGNOSIS DEFICIENT KNOWLEDGE related to information
misinterpretation and unfamiliarity with information resources, as manifested by uncontrolled blood glucose and verbalization of sa pila na ka tuig nako na diabetic kay wala gihapon ko kasabot sa akong sakit and abi nako para sa kidney nang insulin. SB: Knowledge deficit is an absence or deficiency of cognitive information related to a specific topic. The deficit in knowledge may relate to clients or SOs lack of information about the disease process, medication, self-care skills and so on. The nurse needs to provide the information that will increase clients knowledge or learning and that will change clients behavior. Source: Berman, A., Snyder, S. J., Kozier, B., & Erb, G. (2007). Kozier & Erb's Fundamentals of nursing (8th ed., p. 490). Singapore: Pearson Education, Inc. INTERVENTIONS Independent Interventions: 1. Assessed clients knowledge and level of understanding about her disease. R: Provides opportunity to assure accuracy and completeness of knowledge as bases for future learning. 2. Determined motivation and expectation for learning. R: Provides insight useful in developing goals and identifying information needs. 3. Assisted client to identify learning goals and measurable outcomes. R: Helps to frame or focus content to be learned. Provides motivation for learning and a measure to evaluate learning process. 4. Discussed about the disease; its risk factors, causes, symptoms, treatment and management. R: To supplement the client with ideas about his disease 5. Stressed the importance of minimizing sugar intake. R: Eliminating sugar (sucrose and glucose) lowers blood glucose concentrations in both Type 1 and Type 2 diabetic patients, and although recent dietary recommendations suggest that eating small amounts of sugar is of little consequence. 6. Encouraged to have a balanced diet consisting of foods rich in protein, carbohydrates, and vitamin C such as organ meat, green leafy vegetables, rice, orange and guava. R: To ensure that client is receiving enough nutrients in the body 7. Educated about the signs and symptoms to note when the patient is hypoglycemic (shacking, sweating, headache, palpitations, and hunger) and hyperglycemic (). R: Avoiding hypoglycaemia anf hyperglycemia can restore proper warning symptoms and may prevent complications. 8. Instructed to eat hard candies or drink a glass of juice once hypoglycemia is noted and to administer the prescribed medication once hyperglycemic. R: Both hypoglycemia and hyperglycemia can cause complications that threaten your health thus must be treated immediately. 9. Emphasized the importance of proper foot care. R: Many foot problems can be prevented, and all diabetic patients should be aware of the potential problem of foot damage. 10. Stressed the importance of daily monitoring of blood sugar. R: The facility for patients to measure their own blood glucose empowers them to achieve optimal control by their own interventions. 11. Allowed adequate time for integration with clients personal beliefs. R: to address direct conflict and provide information 12. Encouraged asking questions R: To address uncertainties and clarification 13. Provide information about additional or outside learning resources (e.g. pertinent Web sites). R: Promotes ongoing learning at own pace. EVALUATION Desired Outcome: Within an hour of student nurse client interaction, client will be able to verbalize understanding about her disease and enumerate ways on how to manage it. Actual Outcome: December 11, 2012 After an hour of student nurse client interaction, the client was able to verbalize the signs and syptoms she noted before she was admitted in relation to her disease, Mao d.i sige kog ihi-ihi, niya pirmi pa jud ko uhawon. She enumerated ways to manage her disease, Dapat na gyud d.i nako hinayhinayan ang softdrinks noh, kung mu gamay ako sugar mu inom kog juice and dapat ko mag.tsinelas sa sulod sa balay.
READINESS FOR ENHANCED KNOWLEDGE related to unfamiliarity of the disease process and management of the disease as manifested by willingness to learn and expresses interest in learning, Maayo kayo imo kong sulti-an kung unsa nang diabetes dai kay sa pila na ka tuig nako na diabetic kay wala gihapon ko kasabot sa akong sakit SB: Health demonstration of behaviours or cues that reflect the learners motivation to learn at a specific time. Reflects not only the desire orwillingness to learn, but also the ability to learn in a specific time. Source: Berman, A., Snyder, S. J., Kozier, B., & Erb, G. (2007). Kozier & Erb's Fundamentals of nursing (8th ed., p. 490). Singapore: Pearson Education, Inc. Knowledge deficit, frustration, fears can result in the clients decreased compliance with the prescribed therapy, therefore client education is necessary before beginning therapy. It is a fact or causing nonadherance of therapeutic regimen. It is lack of cognitive information on the things required for health recovery, maintenance or health promotion. Source: Smeltzer, S. C., Bare, B. G., Hinkle, J. L., & Cheever, K. H. (2010). Brunner & Suddarth's textbook of medical-surgical nursing (12th ed., p. 848 - 851). Philadelphia: Lippincott Williams & Wilkins. An integral aspect of diabetes care is to inform all patients of the nature of the disorder and its treatment, and to place the potential
threat of complications in their true perspective. Source: Watkins, P.J. (2003). ABC of diabetes. (5th ed). London: BMJ Publishing Group.
14. Asked client on how she is feeling and dealing with the problem and discussed ways on how she could make use of interventions taught and performed. R: To promote independence
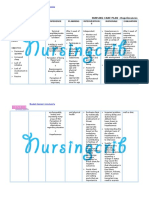
Room: 304 Diagnosis: Non-healing wound, SLE, Diabetes Mellitus Type II NURSING DIAGNOSIS RISK FOR FLUID VOLUME DEFICIT related to excessive gastric losses Cues: 3 episodes of brownish colored watery stools amounting to glass per episode INTERVENTIONS Independent Interventions 1. Assessed frequency and characteristic of stools and other history related to duration and intensity of symptoms such as vomiting and excessive urination. R: Helps estimate total volume depletion. 2. Assessed peripheral pulses, capillary refill time, skin turgor, and mucous membranes. R: Indicators of level of hydration and adequacy of circulating volume. 3. Monitored vital signs R: Vital signs changes such as increased heart rate, decreased blood pressure, and increased temperature may indicate hypovolemia. 4. Monitored intake and output. R: to ensure accurate picture of fluid status 5. Encouraged to increase fluid intake, as tolerated. R: To replace lost volume. 6. Encouraged to have frequent oral hygiene, at least twice a day. R: Oral hygiene decreases unpleasant tastes in the mouth and allows the client to respond to the sensation of thirst. 7. Discussed with patient and SO about factors related to ways they can prevent dehydration. R: Promotes wellness and active family participation. EVALUATION Desired Outcome: Within 8 hours of nursing intervention, client will not manifest signs of dehydration such as dry oral, crack lips, CRT > 2 secs, and poor skin turgor. Patients vital signs will be within normal range (BP = 90120/60-90 mmHg, PR = 60 100 bpm, RR = 12 20 cpm, and T = 36.5 37.5C/axilla). Actual Outcome: December 11, 2012 After 8 hours of nursing intervention, client manifest the following smooth, moist lips, CRT < 2 secs, and good skin turgor. Patients vital signs is as follows (BP = mmHg, PR = bpm, RR = cpm, and T = C/axilla).
SB: Diarrhea is the most common reason for a person to loose excess amounts of water. A significant amount of water can be lost with each bowel movement. Source: Wedro, B. (n.d.). Dehydration.MedicineNet.com. Retrieved December 13, 2012, from www.medicinenet.com.
Room: 303 Diagnosis: Non-healing wound, Diabetes Mellitus Type II, S/P BKA right and debridement on left foot NURSING DIAGNOSIS ACUTE PAIN related to physical injury tissue and nerve trauma, psychological impact of loss of body part secondary to S/P Below the Knee Amputation as manifested by facial grimacing, sharp pain noted after his operation (December 10, 2012) on right leg with a duration of 1-3 mins per episode with a pain scale of 8/10 (10 as the highest and 1 as the lowest), aggravated by movement and relieved by rest and immobilization. INTERVENTIONS Independent Interventions 1. Assessed pain using COLDSPA. R: Aids in evaluating need for and effectiveness of interventions. Changes may indicate developing complications, such as necrosis or infection. 2. Elevated affected leg using 1 2 pillows. R: Lessens edema formation by enhancing venous return; reduces muscle fatigue and skin or tissue pressure. Note: After initial 24 hours and in absence of edema, residual limb may be extended and kept flat. 3. Encouraged relaxation techniques such as deep-breathing exercises. R: Refocuses attention, promotes sense of control, and may enhance coping abilities in the management of the stress of traumatic injury and pain, which is likely to persist for an extended period. 4. Conversed with patient while rendering care. R: Prevents boredom, reduces muscle tension, and can increase muscle strength; may enhance coping abilities. 5. Encouraged verbalization of feelings R: can reduce anxiety and fear thereby reducing perception of intensity of pain 6. Accepted patients description of pain R: To convey acceptance to patients response to pain since pain is a subjective experience and cannot be felt by others 7. Observed nonverbal cues such as facial expressions R: To confirm verbal report of pain 8. Evaluated pain relief/control at regular intervals R: to rule out worsening of underlying condition/development of complications. 9. Provided a therapeutic environment by minimizing noise upon entering the room R: A comfortable environment aids in relaxation and minimizes distractions, promoting effective coping to manage discomfort Collaborative Interventions EVALUATION Desired Outcome: Within 8 hours of nursing intervention, client will be able to report lessened pain based on the pain scale and show non verbal cues such as absence of facial grimacing and guarding behaviour. Actual Outcome: December 11, 2012 After 8 hours of nursing intervention, the client still experience sharp pain noted after his operation (December 10, 2012) on right leg with a duration of 1-3 mins per episode with a pain scale of 7/10 (10 as the highest and 1 as the lowest), aggravated by movement and relieved by rest, immobilization, and medication. Facial grimacing was also still noted.
Room: 303 Diagnosis: Non-healing wound, Diabetes Mellitus Type II, S/P BKA right and debridement on left foot NURSING DIAGNOSIS IMPAIRED PHYSICAL MOBILITY related to neuromuscular involvement: paralysis as manifested by right sided weakness, slurred speech, muscle strength of 2/5 on both upper and lower right extremities. SELF-CARE DEFICIT (feeding, grooming, dressing, ambulation) related to neuromuscular involvement: paralysis as manifested by right sided weakness, slurred speech, muscle strength of 2/5 on both upper and lower right extremities INTERVENTIONS Independent Interventions 1. Inspected skin regularly, especially over bony prominences. R: Pressure points over bony prominences are most at risk for decreased perfusion that may lead to pressure ulcers. 2. Encouraged to have adequate intake of fluids and nutritious foods. R: Promotes well-being and maximizes energy production. 3. Assisted in turning to side or changing positions. R: Reduces risk of tissue ischemia/injury. Affected side has poorer circulation and reduced sensation and is more predisposed to skin breakdown/decubitus. 4. Provided pillows at sides. R: To promote safe environment, to reduce risk of injury. 5. Encouraged to participate in doing ADLs or self care such as eating. R: Enhances self-concept and sense of independence. 6. Encourage to perform passive ROM. R: Exercise promotes increased venous return, prevents stiffness, and maintains muscle strength and endurance. 7. Kept side-rails up and bed in low position. R: This promotes a safe environment. 8. Assisted patient in performing ADLs such as dressing and feeding. R: To aid patient in difficult tasks. 9. Taught the S.O. the importance of providing self-care to the patient R: To motivate the S.O. to perform self-care activities to the patient 10. Encourage scheduling of activities to provide adequate time for rest and sleep. R: To conserve energy. Patients with self-care deficit should conserve as much energy as possible in order to perform rehabilitative interventions effectively. 11. Encouraged SOs to stay with the patient at all times R: To ensure safety and assist patient in doing difficult tasks Collaborative Interventions 1. Encouraged to abide with the therapy ordered by the doctor. R: To develop individual exercise/mobility program and identify appropriate adjunctive devices. EVALUATION Desired Outcome: Within 8 hours of nursing intervention, client will be able to report lessened pain based on the pain scale and show non verbal cues such as absence of facial grimacing and guarding behaviour. Actual Outcome: December 11, 2012 After 8 hours of nursing intervention, the client still experience sharp pain noted after his operation (December 10, 2012) on right leg with a duration of 1-3 mins per episode with a pain scale of 6/10 (10 as the highest and 1 as the lowest), aggravated by movement and relieved by rest, immobilization, and medication. Facial grimacing was also still noted.
Potrebbero piacerti anche
- HoplessnessDocumento16 pagineHoplessnessHamza IshtiaqNessuna valutazione finora
- Clinical Example:: What Additional Assessments Would The Nurse Want To Make To Plan Care For This Client?Documento2 pagineClinical Example:: What Additional Assessments Would The Nurse Want To Make To Plan Care For This Client?Kim Kristine D. GuillenNessuna valutazione finora
- Word Ncp.......... TetanusDocumento6 pagineWord Ncp.......... TetanusaianrNessuna valutazione finora
- Compartment Syndrome NCP (PAIN)Documento2 pagineCompartment Syndrome NCP (PAIN)eunica16Nessuna valutazione finora
- Hypertonic SolutionsDocumento4 pagineHypertonic SolutionsVanessa PaguiriganNessuna valutazione finora
- NCPDocumento4 pagineNCPAndrea BroccoliNessuna valutazione finora
- NCPDocumento3 pagineNCPJoevelyn LaynoNessuna valutazione finora
- Nursing Diagnosis Rationale Interventions Rationale EvaluationDocumento2 pagineNursing Diagnosis Rationale Interventions Rationale EvaluationJobie CasipongNessuna valutazione finora
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Documento6 pagineRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroNessuna valutazione finora
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocumento3 pagineSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNessuna valutazione finora
- Nursing Care Plan For Special ChildrenDocumento2 pagineNursing Care Plan For Special Childrenharas_dcsaisNessuna valutazione finora
- Body Weakness NCPDocumento1 paginaBody Weakness NCPtwicetrashNessuna valutazione finora
- Nursing Care Plan For Tissue InjuryDocumento2 pagineNursing Care Plan For Tissue InjuryJobelle AcenaNessuna valutazione finora
- NCP T2DMDocumento5 pagineNCP T2DMFrancym R. BatengaNessuna valutazione finora
- Imbalanced Nutrition Less Than Body Requirements Diabetes NCP PDFDocumento5 pagineImbalanced Nutrition Less Than Body Requirements Diabetes NCP PDFashamy acolNessuna valutazione finora
- Nursing Care PlanDocumento3 pagineNursing Care Planjnx_anonymousNessuna valutazione finora
- Risk For Acute Confusion 1-4Documento2 pagineRisk For Acute Confusion 1-4DewiRestiNazullyQiran100% (1)
- Nursing Care Plan For LYING inDocumento4 pagineNursing Care Plan For LYING inKarissa CiprianoNessuna valutazione finora
- NCP Making (Ulcerative Colitis & Crohn's Disease)Documento2 pagineNCP Making (Ulcerative Colitis & Crohn's Disease)R Hornilla ArcegaNessuna valutazione finora
- NCP RiskDocumento3 pagineNCP RiskMaricar Azolae MascualNessuna valutazione finora
- Hypokalemia Nursing Care PlanDocumento2 pagineHypokalemia Nursing Care PlanIan Lelis100% (1)
- Impaired Verbal and or Written CommunicationDocumento2 pagineImpaired Verbal and or Written CommunicationHanya Bint Potawan100% (1)
- NCP For Activity IntoleranceDocumento1 paginaNCP For Activity IntoleranceKristine LonyenNessuna valutazione finora
- NCPDocumento8 pagineNCPJoseph Anthony Benitez VerzosaNessuna valutazione finora
- NCP DM Group 6Documento4 pagineNCP DM Group 6Jeffrey Calicdan BucalaNessuna valutazione finora
- Altered Renal Perfusion CRFDocumento4 pagineAltered Renal Perfusion CRFKristel Anne Nillo ZepolNessuna valutazione finora
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocumento3 pagineAssessment Diagnosis Planning Implementation Rationale Evaluationria_soriano_2Nessuna valutazione finora
- NCP Imbalanced NutritionDocumento3 pagineNCP Imbalanced NutritionAav Canlas100% (1)
- NCP For HeadacheDocumento1 paginaNCP For HeadacheJohn MajanNessuna valutazione finora
- Carpenito-Moyet, L. J. (2009) : IndependentDocumento3 pagineCarpenito-Moyet, L. J. (2009) : IndependentClint DelacruzNessuna valutazione finora
- NCP For Bladder CaDocumento4 pagineNCP For Bladder CaChris Tine CaccamNessuna valutazione finora
- NCP 1Documento1 paginaNCP 1hsiriaNessuna valutazione finora
- Deficient KnowledgeDocumento3 pagineDeficient KnowledgeCamilleAnneRoseRabinoNessuna valutazione finora
- Gi-Rle - NCP For Deficient Fluid VolumeDocumento2 pagineGi-Rle - NCP For Deficient Fluid VolumeEvangeline Villa de Gracia100% (1)
- NCPDocumento4 pagineNCPDaniel Garraton0% (1)
- NCPDocumento9 pagineNCPYesha Mae MartinNessuna valutazione finora
- Worksheet#2-Maintaining Asepsis: Medical Asepsis Includes All Practices Intended To Confine A SpecificDocumento4 pagineWorksheet#2-Maintaining Asepsis: Medical Asepsis Includes All Practices Intended To Confine A SpecificCj MayoyoNessuna valutazione finora
- Impaired Gas ExchangeDocumento2 pagineImpaired Gas ExchangeAura Salve Ildefonso Allas100% (3)
- Common Nursing Diagnosis Found in Nursing Care Plans For HypertensionDocumento2 pagineCommon Nursing Diagnosis Found in Nursing Care Plans For HypertensionRaveen mayiNessuna valutazione finora
- Ncp-Impaired S.i.-NavidasDocumento4 pagineNcp-Impaired S.i.-NavidasFran LanNessuna valutazione finora
- COLCHICINE pptx1800128929Documento15 pagineCOLCHICINE pptx1800128929April Mergelle LapuzNessuna valutazione finora
- NCPDocumento4 pagineNCPRachel PerandoNessuna valutazione finora
- Impaired Verbal CommunicationDocumento6 pagineImpaired Verbal CommunicationLaura Sansonetti100% (1)
- Nursing Care Plan Rheumatoid ArthritisDocumento3 pagineNursing Care Plan Rheumatoid ArthritisJashAnia MarIe EvArdo FloresNessuna valutazione finora
- NCP FVDDocumento2 pagineNCP FVDMarlon AnryNessuna valutazione finora
- Hyperthermia NCPDocumento1 paginaHyperthermia NCPMikko Anthony Pingol AlarconNessuna valutazione finora
- Nursing Care Plan For Hopelessness NCPDocumento5 pagineNursing Care Plan For Hopelessness NCPRammiel Saylo CarlosNessuna valutazione finora
- Critical Thinking ExerciseDocumento1 paginaCritical Thinking ExerciseMaye ArugayNessuna valutazione finora
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDocumento2 pagineNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaNessuna valutazione finora
- NCP DiabetesDocumento4 pagineNCP Diabeteskyshb67% (3)
- NCP AidsDocumento16 pagineNCP AidstferdianingsihNessuna valutazione finora
- Activity IntoleranceDocumento3 pagineActivity Intolerancelouie roderosNessuna valutazione finora
- Imbalanced NutritionDocumento2 pagineImbalanced NutritionRizza 이 동해 Ocampo100% (1)
- NCP and Drug Study For Case in SleDocumento34 pagineNCP and Drug Study For Case in SlePaolo Vittorio Perdigueros GonzalesNessuna valutazione finora
- NCP Ineffective Tissue Perfusion and Self Care DeficitDocumento5 pagineNCP Ineffective Tissue Perfusion and Self Care DeficitFrances Anne Pasiliao100% (3)
- NCPDocumento10 pagineNCPannamargie07Nessuna valutazione finora
- Nursing Care PlansDocumento5 pagineNursing Care PlansYannah Mae EspineliNessuna valutazione finora
- CarePlan #2Documento3 pagineCarePlan #2Monika StasiakNessuna valutazione finora
- PlateletDocumento16 paginePlateletArgene Rose MilletNessuna valutazione finora
- Icu NCPDocumento4 pagineIcu NCPdrsabuegNessuna valutazione finora
- Cynosure Starlux 500 Palomar Technical Service ManualDocumento47 pagineCynosure Starlux 500 Palomar Technical Service ManualJF SilvaNessuna valutazione finora
- Proefschrift T. Steenstra - tcm24-268767Documento181 pagineProefschrift T. Steenstra - tcm24-268767SLAMET PAMBUDINessuna valutazione finora
- GCSE AstronomyDocumento30 pagineGCSE Astronomyharris123mc100% (1)
- Kinematics in One DimensionDocumento4 pagineKinematics in One DimensionAldrin VillanuevaNessuna valutazione finora
- Worlds Apart: A Story of Three Possible Warmer WorldsDocumento1 paginaWorlds Apart: A Story of Three Possible Warmer WorldsJuan Jose SossaNessuna valutazione finora
- Texto EBAU 1Documento2 pagineTexto EBAU 1haridianrm13Nessuna valutazione finora
- Lecture Planner - Inorganic Chemistry (Legend) - Yakeen NEET 2.0 2024Documento1 paginaLecture Planner - Inorganic Chemistry (Legend) - Yakeen NEET 2.0 2024Dipendra KumarNessuna valutazione finora
- Dual Op Amp and Voltage Reference Ap4310/ADocumento12 pagineDual Op Amp and Voltage Reference Ap4310/AМихаил ЯненкоNessuna valutazione finora
- FRP Handrail Fittings CatalogDocumento6 pagineFRP Handrail Fittings CatalogAl Adel MorenoNessuna valutazione finora
- Solutions GoldsteinDocumento10 pagineSolutions GoldsteinAnyiNessuna valutazione finora
- NCP Orif Right Femur Post OpDocumento2 pagineNCP Orif Right Femur Post OpCen Janber CabrillosNessuna valutazione finora
- Syllabus Unit Iv Unit Commitment and Economic DispatchDocumento23 pagineSyllabus Unit Iv Unit Commitment and Economic DispatchBALAKRISHNANNessuna valutazione finora
- Considerations For Impeller Trimming - Empowering Pumps and EquipmentDocumento8 pagineConsiderations For Impeller Trimming - Empowering Pumps and Equipment김기준Nessuna valutazione finora
- IV. Network Modeling, Simple SystemDocumento16 pagineIV. Network Modeling, Simple SystemJaya BayuNessuna valutazione finora
- Fully Automatic Coffee Machine - Slimissimo - IB - SCOTT UK - 2019Documento20 pagineFully Automatic Coffee Machine - Slimissimo - IB - SCOTT UK - 2019lazareviciNessuna valutazione finora
- Drilling & GroutingDocumento18 pagineDrilling & GroutingSantosh Laxman PatilNessuna valutazione finora
- Bomba MixerDocumento2 pagineBomba MixerBinelli79Nessuna valutazione finora
- FYP ProposalDocumento11 pagineFYP ProposalArslan SamNessuna valutazione finora
- Highway-And-Railroad-Engineering SummaryDocumento15 pagineHighway-And-Railroad-Engineering SummaryRodin James GabrilloNessuna valutazione finora
- Shawal 1431 AH Prayer ScheduleDocumento2 pagineShawal 1431 AH Prayer SchedulemasjidibrahimNessuna valutazione finora
- Eng DS Epp-2314 1410Documento2 pagineEng DS Epp-2314 1410MarkusAldoMaquNessuna valutazione finora
- Midterm Exam Gor Grade 11Documento2 pagineMidterm Exam Gor Grade 11Algelle AbrantesNessuna valutazione finora
- 02-Building Cooling LoadsDocumento3 pagine02-Building Cooling LoadspratheeshNessuna valutazione finora
- H107en 201906 r4 Elcor Elcorplus 20200903 Red1Documento228 pagineH107en 201906 r4 Elcor Elcorplus 20200903 Red1mokbelNessuna valutazione finora
- Fyp-Hydraulic Brakes CompleteDocumento32 pagineFyp-Hydraulic Brakes CompleteRishabh JainNessuna valutazione finora
- Learning Activity Sheets Introduction To World Religions and Belief SystemDocumento56 pagineLearning Activity Sheets Introduction To World Religions and Belief SystemAngelica Caranzo LatosaNessuna valutazione finora
- Sony Cdm82a 82b Cmt-hpx11d Hcd-hpx11d Mechanical OperationDocumento12 pagineSony Cdm82a 82b Cmt-hpx11d Hcd-hpx11d Mechanical OperationDanNessuna valutazione finora
- Sustainable Events Guide May 30 2012 FINAL PDFDocumento118 pagineSustainable Events Guide May 30 2012 FINAL PDFInter 4DMNessuna valutazione finora
- OurCatholicFaith PowerPoint Chapter1Documento21 pagineOurCatholicFaith PowerPoint Chapter1VinNessuna valutazione finora
- PEH Q3 Long QuizDocumento1 paginaPEH Q3 Long QuizBenedict LumagueNessuna valutazione finora