Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
892
Caricato da
Thessa Grace OrnoDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
892
Caricato da
Thessa Grace OrnoCopyright:
Formati disponibili
Clinical Chemistry 56:6 892896 (2010)
Clinical Case Study
Hyperphosphatemia in a 56-Year-Old Man with Hypochondrial Pain
Tze Ping Loh,* Sharon Saw, and Sunil Kumar Sethi
CASE A 56-year-old Caucasian man with a history of colon cancer status post resection and chemoradiotherapy presented to the emergency medicine department with unintentional weight loss and 6 months of dull right hypochondrial pain with no change in bowel habit. The abdominal pain turned sharp and severe on the day of admission. He was not jaundiced, and no abdominal mass was felt. Initial laboratory investigations revealed a macrocytic, normochromic anemia [hemoglobin, 71 g/L (reference interval, 126 169 g/L); mean corpuscular volume, 98.0 fL (reference interval, 80.196.7 fL); mean corpuscular hemoglobin concentration, 320 g/L (reference interval, 308 384 g/L)]. Serum creatinine, alanine aminotransferase, aspartate aminotransferase, and bilirubin values were within the reference limits. The total protein concentration was 113 g/L (reference interval, 65 82 g/L), and the albumin concentration was 33 g/L (reference interval, 38 48 g/L). The phosphate concentration was markedly increased at 4.84 mmol/L (reference interval, 0.851.45 mmol/L). The total and corrected calcium concentrations were 1.98 mmol/L and 2.20 mmol/L (reference interval for both, 2.152.55 mmol/L), respectively, and the magnesium concentration was 0.76 mmol/L (reference interval, 0.751.07 mmol/L). The analytical indices (lipemia,
bilirubin, and hemolysis) were within acceptable limits. The only medication the patient was taking was atenolol for hypertension. DISCUSSION Phosphate, the most abundant intracellular anion, exists in organic and inorganic forms in the human body. Its multifaceted function involves providing structural support, regulation of intermediary metabolism, genetic coding, cellular signaling, and cell growth (1, 2 ). Nonpathologic homeostasis of phosphate is intimately related to calcium. It is maintained by bone, the kidneys, and the gut in response to changing concentrations of calcium and phosphate, which are mediated by vitamin D, calcitonin, and parathyroid hormone (1, 2 ). Only serum inorganic phosphate, which is 1% of the total body phosphate, is routinely measured (2 ). Measurement of serum inorganic phosphate is commonly based on the reaction of phosphate ions with ammonium molybdate to form a phosphomolybdate complex, which is then measured with a spectrophotometer at 340 nm (1, 2 ). The phosphomolybdate complex can be further reduced to a molybdate complex, which is measured at 600 700 nm to avoid the positive interference of hemolysis, icterus, and lipemia associated with the 340-nm wavelength (1, 2 ). Other, less commonly used methods include the vanadate molybdate and enzymatic methods (1, 2 ). The vanadatemolybdate method, which is carried out at an acidic pH, has a positive bias owing to the hydrolysis of organic phosphate esters, whereas enzymatic methods performed at neutral pH do not (1 ). Hyperphosphatemia occurs when there is a decreased renal excretion of phosphate, an increased phosphate intake, or an increased extracellular phosphate load (1 ). Clinically, a decreased glomerular filtration rate (as in acute or chronic renal failure) leading to decreased renal phosphate excretion is the most common cause of hyperphosphatemia. In the absence of renal failure, increased tubular reabsorption, hypoparathyroidism, pesudohypoparathyroidism, and acromegaly should be suspected (13 ). Increased phosphate intake (frequently iatrogenic) may arise from excessive oral or intravenous phosphate administration or overuse of phosphate-containing laxatives or enemas. Respiratory or metabolic acidosis may hydro-
QUESTIONS TO CONSIDER 1. What are the clinical causes of hyperphosphatemia? 2. What factors are known to cause interference with laboratory phosphate measurement? 3. How can physiological and analytical causes for increased phosphate be distinguished?
Department of Laboratory Medicine, National University Health System, Singapore. * Address correspondence to this author at: 5 Lower Kent Ridge Rd., Singapore 119074. Fax 65-67771613. Received September 10, 2009; accepted December 18, 2009. DOI: 10.1373/clinchem.2009.136895
892
Clinical Case Study
lyze intracellular organic phosphate-containing compounds and release them into the extracellular compartment (1 ). Cell lysis disorders, such as tumor lysis syndrome, hemolytic anemia, and rhabdomyolysis, may all give rise to hyperphosphatemia (1, 2 ). Hyperphosphatemia is usually asymptomatic; however, an acute increase in the phosphate concentration may precipitate calcium and thereby lead to signs and symptoms of hypocalcemia, including paresthesia, tetany, seizure, Chvostek/Trousseau sign, and cardiovascular instability (3 ). Chronic hyperphosphatemia may lead to renal dystrophic calcification, secondary hyperparathyroidism, osteitis fibrosa, and metastatic calcification (3 ). Treatment is mainly targeted at the underlying cause but may involve hemodialysis, aggressive fluid hydration, administration of dextrose and insulin, or administration of acetazolamide acutely (3 ). Dietary restriction of phosphate and administration of phosphate-binding salts are useful for longterm management (1, 3 ).
PSEUDOHYPERPHOSPHATEMIA
Pseudohyperphosphatemia is a falsely increased phosphate concentration due to analytical or preanalytical errors in phosphate measurement. Clinical suspicion should be raised when a high phosphate concentration cannot be sufficiently explained by the patients pathophysiology. Hemolyzed, icteric, and lipemic samples are known to positively interfere with certain methods of phosphate measurement (2 ). Modern analyzers can detect most of these interferences as excessively high analytical indices. Additionally, a prolonged standing or clotting time for a sample may also raise the serum phosphate concentration because of a shift of phosphate from within erythrocytes and platelets to the serum (2 ). The use of liposomal amphotericin B is a lesser-known cause of a falsely increased phosphate concentration that has increasingly been reported with the rise in its use among immunocompromised patients (4 ). Two possible mechanisms have been postulated for this phenomenon. One suggestion is that biodegradation of the liposomal vehicle (for transporting the drug) may interfere with light scatter or precipitation, affecting the absorbance measurement. The second suggestion is that hydrolysis of the organic phosphate in liposome phospholipids is being measured by the assay. Another iatrogenic cause is heparin contamination of samples obtained from hemodialysis catheters (5 ). A simple discussion with the appropriate clinical staff will usually provide clues in the latter 2 scenarios. Spurious hyperphosphatemia in patients with dysproteinemia is well documented (6, 7 ). Causes of dysproteinemia include multiple myeloma, Waldenstrm macroglobulinemia, and monoclonal gammopathy of
undetermined significance (3 ). Frequently, persons with such conditions present with a very high serum phosphate concentration, a typical serum calcium concentration, and no symptoms related to hyperphosphatemia. Spurious hyperphosphatemia may be analytical (i.e., due to interference of paraproteins with the serum phosphate assay) or physiological (i.e., due to the presence of phosphate-binding proteins) (6 8 ). In one instance, hyperphosphatemia was actually thought to be physiologically active in a multiple myeloma patient with a depressed 1,25-dihydroxyvitamin D concentration (8 ). Paraprotein interference in phosphate measurement may be suggested by a serum total protein concentration that is disproportionately higher than the serum albumin concentration, which may be typical or even low. Manual deproteinization of the sample by trichloroacetic/sulfosalicylic acid precipitation, dialysis, wet-ashing with nitric acid and perchloric acid, ultrafiltration, and extreme dilution have previously been described to achieve a more accurate measurement of serum phosphate (7, 9 ). Furthermore, the purine nucleoside phosphorylase based enzymatic method has been suggested as an appropriate alternative assay for paraproteinemic sera (2 ). It is important to identify pseudohyperphosphatemia secondary to paraproteinemia because it not only eliminates unnecessary clinical interventions but also may reveal a major diagnosis. Use of dry-film technology, which removes proteins before phosphate analysis, reduces the likelihood of miscalling a dysproteinemic sample as hyperphosphatemic and avoids misleading clinicians (10 ). Ironically, the elimination of pseudohyperphosphatemia may in turn deprive clinicians of a valuable clue to the presence of these clinically important disorders if total protein is not measured. Not all patients with dysproteinemia and a high serum phosphate concentration will have pseudohy-
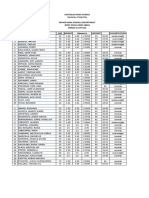
Table 1. Summary of patients laboratory investigation before and after manual deproteinization.
Before deproteinization After deproteinization
Phosphate, mmol/L Advia 2400 Vitros 5600 IgG, g/L Integra 400 Plus Total protein, g/L Advia 2400 113 0 108.3 0.05 3.81 1.28 1.15 1.09
Clinical Chemistry 56:6 (2010) 893
Clinical Case Study
Fig. 1. Serum protein electrophoresis showing the M band and its quantification. A/G, albumin globulin ratio.
perphosphatemia; further workup may be required, depending on the clinical scenario. Good communication between clinical laboratory and clinical staff is key to identifying such unsuspected and rare cases of pseudohyperphosphatemia.
RESOLUTION OF THE CASE
val, 0.80 2.00 g/L). The same sample was then subjected to ultrafiltration with a 10K Amicon Ultracel Centrifugal Filter device (Millipore), centrifuged at 1811g for 30 min (Eppendoff centrifuge), and then measured again with the 2 analyzers. The phosphate
Pseudohyperphosphatemia was suspected when the clinical presentation and initial laboratory investigations failed to explain the excessively high phosphate concentration, and the laboratory was consulted. In the absence of preanalytical causes such as abnormal analytical indices, medication, and prolonged processing of the patients sample, an analytical interference was regarded as the most likely source of the interference. Paraproteinemia was strongly considered in view of the discordant serum concentrations of total protein and albumin, and the patient was investigated for possible multiple myeloma. The initial phosphate concentration was measured by means of the 1-step phosphomolybdate/UV principle (Advia 2400; Siemens Healthcare Diagnostics). We subsequently received a second request for a phosphate concentration, which was measured on both the Advia 2400 instrument and the Vitros 5600 platform (Ortho Clinical Diagnostics), which includes the additional step of converting the phosphomolybdate complex to heteropolymolybdate blue for measurement. The results were 3.81 mmol/L (Advia 2400) and 1.28 mmol/L (Vitros 5600). Immunoglobulin quantification revealed the following: IgA, 0.21 g/L (reference interval, 0.80 4.00 g/L); IgG, 108.30 g/L (reference interval, 5.00 15.00 g/L); and IgM, 0.13 g/L (reference inter894 Clinical Chemistry 56:6 (2010)
POINTS TO REMEMBER 1. Hyperphosphatemia can be caused by a decreased renal excretion of phosphate (most commonly due to renal failure), increased oral or intravenous phosphate intake (usually iatrogenic), respiratory or metabolic acidosis, or a major cellular lysis event, such as tumor lysis syndrome or intravascular hemolysis. 2. Pseudohyperphosphatemia is a falsely increased phosphate concentration that can be caused by preanalytical issues such as improper sampling, prolonged clotting, very high analytical indices, and, occasionally, medication. More importantly, it may be caused by dysproteinemia, especially in the presence of disproportionately high total protein concentration relative to the serum albumin concentration. 3. Chemical and physical deproteinization can be used to separate the interfering protein for a better measurement of serum inorganic phosphate, although an enzyme-based assay may work just as well. 4. Communication between the clinical laboratory and clinical staff is key to the early identification of potential pseudohyperphosphatemia.
Clinical Case Study
concentration decreased noticeably to 1.15 mmol/L on the Advia 2400 and less so to 1.09 mmol/L on the Vitros 5600. The concentrations of IgG and total protein in the ultrafiltrate were also measured. The IgG concentration was 0.05 g/L with the Integra 400 Plus instrument (Roche Diagnostics), and the total protein concentration was 0 g/L with the Advia 2400. Table 1 summarizes the patients laboratory investigations. The discrepancy between the phosphate results obtained with the Advia 2400 and Vitros 5600 was dramatically reduced with physical deproteinization of the blood sample. The ability of the Vitros 5600 instrument to measure the serum phosphate concentration in a dysproteinemic sample closer to its deproteinized state may be attributed to the effectiveness of the multilayered reaction slide used. The multilayered reaction slide is topped with a BaSO4 spreading layer, which is capable of filtering large molecules such as proteins, lipids, and hemoglobin (10 ). In this setting, the spreading layers appeared to be effective in removing IgG, which would otherwise interfere with the phosphate measurement. The eventual diagnosis for the patient was multiple myeloma, according to serum protein electrophoresis (Fig. 1) and hematologic studies, and he was treated accordingly.
data, or analysis and interpretation of data; (b) drafting or revising the article for intellectual content; and (c) final approval of the published article. Authors Disclosures of Potential Conflicts of Interest: No authors declared any potential conflicts of interest. Role of Sponsor: The funding organizations played no role in the design of study, choice of enrolled patients, review and interpretation of data, or preparation or approval of manuscript. Acknowledgments: We are thankful to the technical staff of Core Laboratory, National University Health System, for their help.
References
1. Endres DB, Rude RK. Bone and mineral metabolism. In: Burtis CA, Ashwood ER, Bruns DE, eds. Tietz textbook of clinical chemistry and molecular diagnostics. 4th ed. St. Louis: Elsevier; 2006. p 19059. 2. Schmidt-Gayk H. Measurement of calcium, phosphate and magnesium. In: Seibel M, Robins S, Bilezikian J, eds. Dynamics in bone and cartilage metabolism. Burlington (MA): Academic Press; 2006. p 4959. 3. Weiss-Guillet E-M, Takala J, Jakob SM. Diagnosis and management of electrolyte emergencies. Best Pract Res Clin Endocrinol Metab 2003;17:62351. 4. Mendoza D, Connors S, Lane C, Stehnach S. Liposomal amphotericin B as a cause of pseudohyperphosphatemia. Clin Infect Dis 2008;46:645 6. 5. Schiller B, Virk B, Blair M, Wong A, Moran J. Spurious hyperphosphatemia in patients on hemodialysis with catheters. Am J Kidney Dis 2008;52:61720. 6. Larner AJ. Pseudohyperphosphatemia. Clin Biochem 1995;28:3913. 7. Sonnenblick M, Eylath U, Brisk R, Eldad C, Hershko C. Paraprotein interference with colorimetry of phosphate in serum of some patients with multiple myeloma. Clin Chem 1986;32:15379. 8. Mandry JM, Posner MR, Tucci JR, Eil C. Hyperphosphatemia in multiple myeloma due to a phosphate-binding immunoglobulin. Cancer 1991;68:1092 4. 9. Adler SG, Laidlaw SA, Lubran MM, Kopple JD. Hyperglobulinemia may spuriously elevate measured serum inorganic phosphate levels. Am J Kidney Dis 1988;11:260 3. 10. Ortho Clinical Diagnostics. VITROS Chemistry Products PHOS Slides. Instructions for use [Product Insert]. Publication No. MP2 45, version 6.0.
Author Contributions: All authors confirmed they have contributed to the intellectual content of this paper and have met the following 3 requirements: (a) significant contributions to the conception and design, acquisition of
Commentary
Vivek Roy*
Laboratory tests are an important component of comprehensive medical evaluations. These tests provide helpful information that can complement or confirm clinical suspicion, and they can sometimes identify problems that are not clinically evident. On the other hand, tests may provide inaccurate or misleading information under certain circumstances. Hyperphosphatemia is a relatively uncommon laboratory abnormality most often seen in patients with advanced renal failure, hypoparathyroidism, cellular lysis, or excessive phosphate intake (or iatrogenic administration). Hyperphosphatemia may occur artifactually from a
Mayo Clinic, Jacksonville, FL. * Address correspondence to the author at: Mayo Clinic, 4500 San Pablo Rd., Jacksonville, FL 32224. E-mail roy.vivek@mayo.edu. Received March 23, 2010; accepted March 26, 2010. DOI: 10.1373/clinchem.2010.146514
hemolysed, icteric, or lipemic sample; a prolonged delay between blood draw and analysis; or heparin contamination. Hyperglobulinemia (paraproteinemia) has long been recognized to cause spurious serum phosphate readings because of analytical interference. Paraproteinemia is also known to affect many other laboratory parameters, including blood urea nitrogen, creatinine, bilirubin, calcium, iron, sodium, and lipoproteins. The precise frequency with which these artifactual abnormalities are encountered in the clinic or laboratory is unknown, but the phenomenon is potentially substantially underrecognized. The frequency is likely to increase in the future. The prevalence of paraproteinemia increases with age, reaching 10% in persons 80 years of age. Older persons are also more likely to have multiple comorbidities and therefore require multiple laboratory tests. Thus, with the increasing mean age of the population, there are increasing opportunities for clinicians to
Clinical Chemistry 56:6 (2010) 895
Clinical Case Study
encounter paraproteinemia-related artifactual laboratory abnormalities. The importance of recognizing this phenomenon is self-evident: to avoid misinterpretation of data and unnecessary testing. This possibility should be considered when encountering a totally unexpected abnormality that does not fit in the clinical context. When paraproteinemia is suspected, further evaluation should be undertaken in consultation with a laboratory medicine specialist. Repeating the test after deproteination, further dilution of the sample, or use of an alternative testing methodology are some of the strategies available for further investigation.
Author Contributions: All authors confirmed they have contributed to the intellectual content of this paper and have met the following 3 requirements: (a) significant contributions to the conception and design, acquisition of data, or analysis and interpretation of data; (b) drafting or revising the article for intellectual content; and (c) final approval of the published article. Authors Disclosures of Potential Conflicts of Interest: No authors declared any potential conflicts of interest. Role of Sponsor: The funding organizations played no role in the design of study, choice of enrolled patients, review and interpretation of data, or preparation or approval of manuscript.
Commentary
David B. Endres*
Loh et al. report the clinical case of a patient with pseudohyperphosphatemia owing to paraprotein (monoclonal immunoglobulin) interference and remind us of the importance of correlating laboratory results with clinical findings and of encouraging communication between the laboratory and physicians. Paraproteins are common interferents in routine chematology assays. More than 70 published reports have documented paraprotein interference with a variety of analytes, including calcium, direct and total bilirubin, creatinine, glucose, HDL and LDL cholesterol, iron, phosphate, sodium, urea, uric acid, coagulation tests, and blood cell counts (1 ). The importance of paraprotein interference should not be underestimated, given the prevalence of paraproteinemia (3.2% and 5.3% for persons 50 and 70 years of age, respectively) (2 ). Paraproteins cause interference via several mechanisms. The most common is the formation of turbidity due to the precipitation of paraproteins during the test reaction. Test results can be falsely low or high. Paraprotein interference is underrecognized and underreported. Systematic studies of sera from patients with monoclonal gammopathies have reported that interference is far more frequent than can be inferred from case reports (3 ). Given the prevalence of paraproteins and their interference with analyte measurements, more approaches are needed for reducing and detecting this interference. Manufacturers of diagnostic reagents can
optimize reagents (e.g., detergents, ionic strength) to reduce interference and can flag interference by monitoring reaction kinetics and sample consistency. Laboratories can use software to identify samples that may have paraproteins or paraprotein interference. Examples of the use of test results and interference indices to identify such samples include (a) samples with a low albumin concentration and an increased total protein concentration, (b) samples with discordant interference indices and test results (e.g., an increased icteric index and normal total or direct bilirubin values), (c) samples with discordant test results (e.g., a direct bilirubin value greater than the total bilirubin value), and (d) samples with negative or improbable undetectable results (e.g., HDL cholesterol).
Author Contributions: All authors confirmed they have contributed to the intellectual content of this paper and have met the following 3 requirements: (a) significant contributions to the conception and design, acquisition of data, or analysis and interpretation of data; (b) drafting or revising the article for intellectual content; and (c) final approval of the published article. Authors Disclosures of Potential Conflicts of Interest: No authors declared any potential conflicts of interest. Role of Sponsor: The funding organizations played no role in the design of study, choice of enrolled patients, review and interpretation of data, or preparation or approval of manuscript.
References
1. Roy V. Artifactual laboratory abnormalities in patients with paraproteinemia. South Med J 2009;102:16770. 2. Kyle RA, Therneau TM, Rajkumar SV, Larson DR, Plevak MF, Offard JR, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med 2006;354:13629. 3. Yang Y, Howanitz PJ, Howanitz JH, Gorfajn H, Wong K. Paraproteins are a common cause of interferences with automated chemistry methods. Arch Pathol Lab Med 2008;132:21723.
Keck School of Medicine, University of Southern California, Los Angeles, CA. * Address correspondence to the author at: Keck School of Medicine, University of Southern California, 1100 North State St., LAC USC Medical Center, Clinic Tower, A7E113, Los Angeles, CA 91214. Fax 323-843-9376; e-mail endres@ usc.edu. Received March 30, 2010; accepted March 31, 2010. DOI: 10.1373/clinchem.2010.146522
896 Clinical Chemistry 56:6 (2010)
Potrebbero piacerti anche
- Phosphate BishopDocumento3 paginePhosphate BishopElvan Dwi WidyadiNessuna valutazione finora
- Fouque Et Al AJKDDocumento8 pagineFouque Et Al AJKDhubik38Nessuna valutazione finora
- Abnormalities of Calcium Phosphorus and MagnesiumDocumento56 pagineAbnormalities of Calcium Phosphorus and MagnesiumGiancarlo CajahuaringaNessuna valutazione finora
- Hypercalcemia: Etiology and Management: Amanda Demauro Renaghan and Mitchell H. RosnerDocumento3 pagineHypercalcemia: Etiology and Management: Amanda Demauro Renaghan and Mitchell H. RosnerbabiNessuna valutazione finora
- Approach To Treatment of Hypophosphatemia: Acid-Base and Electrolyte Teaching CaseDocumento7 pagineApproach To Treatment of Hypophosphatemia: Acid-Base and Electrolyte Teaching CasemasranraisaNessuna valutazione finora
- Drug Induced Hyperuricemia GoutDocumento3 pagineDrug Induced Hyperuricemia GoutAnggun Cahya MertyanaNessuna valutazione finora
- Hyperparathyroidism Main Jan 2020Documento20 pagineHyperparathyroidism Main Jan 2020paingmyint100% (1)
- Phospha TDocumento2 paginePhospha TTanveerNessuna valutazione finora
- What Are The Classification of ALP?Documento4 pagineWhat Are The Classification of ALP?Frances FranciscoNessuna valutazione finora
- Journal of Pharmaceutical and Biomedical AnalysisDocumento9 pagineJournal of Pharmaceutical and Biomedical AnalysisriskaNessuna valutazione finora
- Metabolic HyperferritinemiaDocumento12 pagineMetabolic HyperferritinemiakocagerahmetNessuna valutazione finora
- Lmad 012Documento5 pagineLmad 012Arturo Eduardo Huarcaya OntiverosNessuna valutazione finora
- Halothane Induced..CrDocumento2 pagineHalothane Induced..CrMuhammad Azhar QureshiNessuna valutazione finora
- Guidelines For The Diagnosis and Treatment of Cobalamin and Folate DisordersDocumento6 pagineGuidelines For The Diagnosis and Treatment of Cobalamin and Folate DisordersOndire PatrickNessuna valutazione finora
- Drug-Induced Endocrine and Metabolic Disorders: OrrespondenceDocumento2 pagineDrug-Induced Endocrine and Metabolic Disorders: OrrespondenceApocalypto StatumNessuna valutazione finora
- Hypo Phosphate MiaDocumento15 pagineHypo Phosphate Miacute_maimaiNessuna valutazione finora
- 2359 4292 Aem 66 05 0651Documento7 pagine2359 4292 Aem 66 05 0651Juanjo Moreno LópezNessuna valutazione finora
- Phosphorus Restriction Prevents Parathyroid Gland Growth: High Phosphorus Directly Stimulates PTH Secretion in VitroDocumento7 paginePhosphorus Restriction Prevents Parathyroid Gland Growth: High Phosphorus Directly Stimulates PTH Secretion in VitroDaniel Lee Eisenberg JacobsNessuna valutazione finora
- UKMI QA How Is Acute Hypophosphataemia Treated in Adults Update July 2017Documento4 pagineUKMI QA How Is Acute Hypophosphataemia Treated in Adults Update July 2017RobMarvinNessuna valutazione finora
- BiomedicinesDocumento12 pagineBiomedicinessamuelNessuna valutazione finora
- ChoiDocumento19 pagineChoiLuciana RafaelNessuna valutazione finora
- Jurnal Hiperfosfat 1Documento25 pagineJurnal Hiperfosfat 1Anggie Pradetya MaharaniNessuna valutazione finora
- Article Casey LIVER Hepatic CirrhosisDocumento8 pagineArticle Casey LIVER Hepatic CirrhosisMaría José Muñoz PalaciosNessuna valutazione finora
- Patel 2020Documento31 paginePatel 2020larissa brandaliseNessuna valutazione finora
- Alteraciones Metabólicas y Hormonales en Gatos Con Lipidosis Hepática (Inglés)Documento7 pagineAlteraciones Metabólicas y Hormonales en Gatos Con Lipidosis Hepática (Inglés)AndreaNessuna valutazione finora
- 5 Revathi EtalDocumento5 pagine5 Revathi EtaleditorijmrhsNessuna valutazione finora
- 1 s2.0 S0272638614013572 Main PDFDocumento9 pagine1 s2.0 S0272638614013572 Main PDFemyNessuna valutazione finora
- Normal Anion GapDocumento5 pagineNormal Anion Gapatribecalledquest20Nessuna valutazione finora
- Intensive Care 1Documento6 pagineIntensive Care 1raitchuNessuna valutazione finora
- Fechner 2001Documento7 pagineFechner 2001Daniel PmNessuna valutazione finora
- A Review of Drug Induced HypocalcemiaDocumento8 pagineA Review of Drug Induced HypocalcemiaKrisna MulasimadhiNessuna valutazione finora
- Encefalopatia Hepatica FisiopatologiaDocumento5 pagineEncefalopatia Hepatica FisiopatologiaEdson Saavedra EcheverreNessuna valutazione finora
- Febuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go ToDocumento9 pagineFebuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go ToAnadi GuptaNessuna valutazione finora
- Probióticos para Tratamiento de Hígado Graso No AlcohólicoDocumento8 pagineProbióticos para Tratamiento de Hígado Graso No AlcohólicoNorlan Ariel Caldera NavarreteNessuna valutazione finora
- An Update Related To Chronic Kidney DiseaseDocumento3 pagineAn Update Related To Chronic Kidney DiseaseMaan CheskaNessuna valutazione finora
- Serum Lysophospholipid Levels Are Altered in Dyslipidemic HamstersDocumento14 pagineSerum Lysophospholipid Levels Are Altered in Dyslipidemic HamstersTheodora TeddyNessuna valutazione finora
- Perez Pozo2009Documento8 paginePerez Pozo2009Anonymous 0mtGtB6u3Nessuna valutazione finora
- HypophosphatemiaDocumento11 pagineHypophosphatemiaFlorygene Kris DisagonNessuna valutazione finora
- Amorim, Et Al., 2021, OCR Mitochondria HepG2Documento27 pagineAmorim, Et Al., 2021, OCR Mitochondria HepG2dhanNessuna valutazione finora
- Effects of Resveratrol On High-AltitudeDocumento24 pagineEffects of Resveratrol On High-AltitudeJocilene Dantas Torres NascimentoNessuna valutazione finora
- Accumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaDocumento5 pagineAccumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaJana NgNessuna valutazione finora
- Hiperparatiroid: Dr. Dr. Shahrul Rahman, SP - PD, FINASIMDocumento50 pagineHiperparatiroid: Dr. Dr. Shahrul Rahman, SP - PD, FINASIMBonitavanyNessuna valutazione finora
- HS BCSH Sept 2011Documento40 pagineHS BCSH Sept 2011lidya_zhuangNessuna valutazione finora
- Acute Liver Injury and FailureDocumento14 pagineAcute Liver Injury and FailureWeslei ChaconNessuna valutazione finora
- Bio 2 Project For PresentationDocumento13 pagineBio 2 Project For PresentationAmr Hasan Abdelfattah NasrNessuna valutazione finora
- Current Concepts of And: Hyperuricemia GoutDocumento13 pagineCurrent Concepts of And: Hyperuricemia GoutAnonymous h0XxWy8SNessuna valutazione finora
- PhosphateDocumento5 paginePhosphateInna BeltranNessuna valutazione finora
- Glicerofosfato de Sodio Vs InogarnicoDocumento8 pagineGlicerofosfato de Sodio Vs InogarnicojhonNessuna valutazione finora
- Capstone Final Justin IsnerDocumento21 pagineCapstone Final Justin Isnerapi-312746225Nessuna valutazione finora
- Pattern of Elevated Serum Alkaline Phosphatase (ALP) Levels in Hospitalized PatientsDocumento7 paginePattern of Elevated Serum Alkaline Phosphatase (ALP) Levels in Hospitalized PatientsDannyNessuna valutazione finora
- LO Week 5 Tropmed SeninDocumento27 pagineLO Week 5 Tropmed Seninphineas ferbNessuna valutazione finora
- Toksik 1Documento5 pagineToksik 1wiwin nur halizaNessuna valutazione finora
- Changes in The Electrolyte Profile of Patients Having HypothyroidismDocumento5 pagineChanges in The Electrolyte Profile of Patients Having Hypothyroidism123someone123Nessuna valutazione finora
- Hemolytic Anemia, SuicideDocumento5 pagineHemolytic Anemia, SuicideturkiNessuna valutazione finora
- Pubmed HecidinaDocumento9 paginePubmed HecidinaeddcitoNessuna valutazione finora
- Acidose e Sua Implicação em Laminite NocekDocumento24 pagineAcidose e Sua Implicação em Laminite NocekRafael NicolinoNessuna valutazione finora
- Biochemical Measurement Aberrations in Extreme LeukocytosisDocumento2 pagineBiochemical Measurement Aberrations in Extreme LeukocytosisgunawanNessuna valutazione finora
- Sindrome de Lisis Tumoral 2017Documento12 pagineSindrome de Lisis Tumoral 2017JERÓNIMO RINCÓNNessuna valutazione finora
- Hypophosphatemia, (Low Phosphate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandHypophosphatemia, (Low Phosphate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Age NCPDocumento2 pagineAge NCPCharmaine Dela CruzNessuna valutazione finora
- ScabiesDocumento14 pagineScabiessyemiNessuna valutazione finora
- Icmr Specimen Referral Form For Covid-19 (Sars-Cov2) : Section A - Patient DetailsDocumento2 pagineIcmr Specimen Referral Form For Covid-19 (Sars-Cov2) : Section A - Patient DetailsPcrNessuna valutazione finora
- Health Reporting Mind IllnessesDocumento8 pagineHealth Reporting Mind IllnessesChristian Kyle Talledo BaclayNessuna valutazione finora
- AcuteExpertSystem PDFDocumento3 pagineAcuteExpertSystem PDFMMHMOONNessuna valutazione finora
- Toxic Anterior Segment SyndromeDocumento13 pagineToxic Anterior Segment SyndromePrathibha M ChachadiNessuna valutazione finora
- Test Bank For Pathology For The Physical Therapist Assistant 1st Edition by GoodmanDocumento5 pagineTest Bank For Pathology For The Physical Therapist Assistant 1st Edition by Goodmanblanchepandorat6bNessuna valutazione finora
- Anthony Olvera - Psa Brochure Assignment - 4682908Documento5 pagineAnthony Olvera - Psa Brochure Assignment - 4682908api-501232916Nessuna valutazione finora
- 2024-Article Text-6560-1-10-20230128Documento4 pagine2024-Article Text-6560-1-10-20230128Adniana NareswariNessuna valutazione finora
- BMI2018Documento9 pagineBMI2018jeffordillasNessuna valutazione finora
- Chapter 3Documento7 pagineChapter 3vine32515Nessuna valutazione finora
- (JURNAL, Eng) A Retrospective Cohort Review of Prescribing in Hospitalised Patients With Heart Failure Using Beers Criteria and STOPP RecommendationsDocumento7 pagine(JURNAL, Eng) A Retrospective Cohort Review of Prescribing in Hospitalised Patients With Heart Failure Using Beers Criteria and STOPP RecommendationsAurellia Annisa WulandariNessuna valutazione finora
- Lec. Deep CariesDocumento47 pagineLec. Deep CariesMaria EvergardenNessuna valutazione finora
- UNIT II MedicalDocumento34 pagineUNIT II Medicalangelax1.1Nessuna valutazione finora
- Community - Based NursingDocumento16 pagineCommunity - Based NursingManu CvNessuna valutazione finora
- Inflammation - The Silent Killer - Terra Health EssentialsDocumento6 pagineInflammation - The Silent Killer - Terra Health EssentialshighlanderoneNessuna valutazione finora
- UTI Prevention Fact SheetDocumento1 paginaUTI Prevention Fact Sheetalifia alqibtiaNessuna valutazione finora
- WHO - Weekly Epidemiological Update On COVID-19 - 22 February 2022Documento26 pagineWHO - Weekly Epidemiological Update On COVID-19 - 22 February 2022Adam ForgieNessuna valutazione finora
- 10 Squamouspapilloma-ReportoftwocasesDocumento7 pagine10 Squamouspapilloma-ReportoftwocasesAyik DarkerThan BlackNessuna valutazione finora
- Case-Presentation OTITIS MEDIADocumento22 pagineCase-Presentation OTITIS MEDIAJean nicole GaribayNessuna valutazione finora
- Photodynamic TherapyDocumento5 paginePhotodynamic TherapyPranav UpadhyayaNessuna valutazione finora
- Job Objective: Core CompetenciesDocumento2 pagineJob Objective: Core Competenciessrivari sriniNessuna valutazione finora
- The REMAP-CAP InvestigatorsDocumento32 pagineThe REMAP-CAP InvestigatorsAaron Nureña JaraNessuna valutazione finora
- Stroke 2Documento8 pagineStroke 2Jarmy BjNessuna valutazione finora
- First Aid Book PDFDocumento47 pagineFirst Aid Book PDFHannan AliNessuna valutazione finora
- (Bio 024) Lab Activity 12 - BloodDocumento7 pagine(Bio 024) Lab Activity 12 - BloodJelleane Paja TaoataoNessuna valutazione finora
- Mrcs Part A ScheduleDocumento6 pagineMrcs Part A ScheduleOliverYousryNessuna valutazione finora
- Excessive Gingival Display - FinalDocumento11 pagineExcessive Gingival Display - FinalPhilippe Bocanegra FernándezNessuna valutazione finora
- Health Science Students' Attitudes Towards Healthcare Teams: A Comparison Between Two UniversitiesDocumento8 pagineHealth Science Students' Attitudes Towards Healthcare Teams: A Comparison Between Two Universitieshamayal xNessuna valutazione finora
- To Whomsoever It May ConcernDocumento7 pagineTo Whomsoever It May ConcernMuhammad IbrahimNessuna valutazione finora