Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Clinical Approach To Respiratory Distress in Newborn
Caricato da
abhivnairTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Clinical Approach To Respiratory Distress in Newborn
Caricato da
abhivnairCopyright:
Formati disponibili
Clinical approach to Respiratory Distress in Newborn.
Indian J Pediatr (Supplement- optimum pulmonary care of neonates) 2003;70: S53 S59
CLINICAL APPROACH TO RESPIRATORY DISTRESS IN NEWBORN
K. K. Diwakar MD. Head, Neonatal Division, Professor, Department of Pediatrics, Kasturba Medical College, Manipal, Karnataka 576119.
Correspondence:
K. K. Diwakar MD. Head, Neonatal Division, Professor, Department of Pediatrics, Kasturba Medical College, Manipal, Karnataka 576119
Tel: 08252 571201 ext 22466 FAX: 08252 570061 attn: KK Diwakar, NICU. e-mail: krishnadiwakar@mail.fulbrightweb.org 1
ABSTRACT
Respiratory distress is a common reason for a neonate seeking medical attention. The clinical features of tachypnea, intercostals retractions, grunting or cyanosis could be the manifestations of a variety of etiological causes. Both pulmonary and extrapulmonary causes could present as tachypnea and respiratory distress. While conditions like Hyaline membrane disease (HMD) is seen more in premature infants, others like Meconium Aspiration Syndrome (MAS) considered a disease of the more mature infant. Infections and structural anomalies like Tracheo-esophageal fistula (TEF)and Congenital Diaphragmatic Hernia (CDH) are common in both term and preterm infants. Stabilization of the infant and early recognition of the etiology helps in minimizing complication and ensuring appropriate definitive therapy. An overview of a few common cause of respiratory distress in the newborn is being discussed in this article.
Key words: Respiratory Distress, Newborn.
Respiratory distress is a common cause of admission of a Neonate in the intensive care unit. 1, 2 .The clinical picture of a neonate with varied combination of tachypnea, retractions, nasal flaring, grunting and cyanosis constitute a familiar scenario in a neonatal intensive care unit. When faced with a neonate with respiratory distress it becomes necessary to compartmentalize the management into an initial phase focusing on the degree of respiratory compromise, resuscitation of the neonate and optimizing its tissue oxygenation, and a planned subsequent phase to clarify the nuances of etiology, definitive management and follow up.
The weight and gestation of the infant and the degree of respiratory compromise would be the key factors to decide the level of care the infant would require. While infants of lower weight and gestation would require more advanced facilities, larger infants can often be managed at smaller centers. Simple clinical scores like the Downess score 3 if meticulously documented at 30 60 minutes intervals are very useful to determine the progression of the respiratory distress. The importance of such an evaluation would be invaluable to plan referrals in the resource-limited environment of developing countries, where structured neonatal transportation facilities are unavailable. A clinical evaluation should whenever possible include oxygen saturation (SaO2) assessment by Pulse Oximetry. SaO2 below 88 % would indicate hypoxia. While SaO2 between 88 94 % would be normal in the more premature neonates, higher SaO2 values are the norm in
term infants. Increasing requirement of inspired oxygen, to maintain normal SaO2 would therefore be an ominous sign.
While the clinical presentation could be similar, the etiology, prognosis and management of the patients presenting with respiratory distress could be varied and diverse. The distress of the infant could be attributed to pulmonary or extra-pulmonary disorders. A functionally normal lung could be at times called upon to work at a capacity far exceeding natural level, in order to compensate for abnormalities of other systems. eg. In the presence of metabolic acidosis, cardiac disease or abdominal distension. The extra effort required of lungs enclosed in a compliant rib-cage could manifest as tachypnea, chest retraction, prominence of accessory muscles of respiration and resultant fatigue leading to further de-compensation. The definitive management of such an infant would naturally be based on the treating the primary extra-pulmonary etiology.
It must be reinforced that the initial management of all infants presenting with respiratory distress is aimed at preventing hypoxia, hypercapnia and acidosis in the newborn. The methods adapted for this could vary from oxygen supplementation to various strategies of mechanical ventilation.
Despite a relatively uniform approach to the initial management, one must realize that procrastination and delay in instituting definitive therapy would result in adverse outcome. For example, an infant with tension pneumothorax could rapidly deteriorate despite the transient improvement of initial therapy, if the pneumothorax is not
evacuated. Similarly, repeated aspiration pneumonia would contribute to poor surgical outcome in patients with delayed diagnosis of tracheoesophageal fistula (TEF). Therefore a definite diagnosis is mandatory for successfully managing infants with respiratory distress.
The cause of for neonatal respiratory distress could be broadly classified as 1) Causes affecting respiration at alveolar level: HMD, Pneumonia, Meconium Aspiration Syndrome, Pneumothorax, pulmonary hemorrhage, PPHN, TTN 2) Structural anomalies of respiratory tract: eg Choanal Atresia, Tracheo-esophageal fistula, Congenital Diaphragmatic hernia, Congenital Lobar Emphysema. 3) Extrapulmonary causes: eg. Bone defects of the chest wall, Congenital heart disease, Metabolic acidosis.
Is the respiratory distress and cyanosis due cardiac or pulmonary problems? Is the distress an effect of metabolic acidosis due to some other cause?
Differentiating a cardiac from pulmonary cause is often easier said than done. The radiological picture of total anomalous pulmonary venous connection (TAPVC) or that of a hypoplastic left heart with pulmonary edema would often resemble that of common pulmonary causes for neonatal respiratory distress. Radiological differentiation becomes even more difficult in the presence of an under expanded lung or a rotated view! It used
to be believed that hyperoxia test done by ventilating the infant for 20 minutes in 100% oxygen would help differentiate the pulmonary from cardiac causes. While an arterial oxygen concentration (PaO2) greater than 200 - 250 torr favours a pulmonary cause, lower values do not positively indicate a cardiac etiology. The availability of Echocardiography has thankfully made the diagnosis of a cardiac disease immeasurably easier.
Tachypnea and respiratory distress could be a presentation of metabolic acidosis. Renal disease, inborn errors of metabolism (IEM) and late metabolic acidosis are forerunners of a long list of causes for metabolic acidosis. While a history of oligohydraminios, poor urine output or urine stream could suggest a renal disease, a history of sibling death or sibling with similar clinical presentation would favour IEM. A low birth weight infant on cows milk supplementation should arouse the suspicion of late metabolic acidosis. Chest X-ray unexplainably normal to justify the degree of tachypnea should alert one to the possibility of metabolic acidosis being the cause for the distress. SaO2 is usually normal in these patients. Arterial blood gases would confirm metabolic acidosis. Biochemical evaluation for renal failure, renal tubular acidosis (RTA) and IEM constitute an essential part of managing such patients.
Pulmonary disorders that manifest in the newborn are usually related to immaturity of the lung, events that occurred in the perinatal period, or a result of congenital
malformations 4 . The role of history in diagnosing the disease can never be overestimated. It could be confidently said that the pulmonary causes for respiratory distress are far commoner than the extra pulmonary ones. The gestation of the infant is probably the single most important factor that influences our clinical outlook. While structural anomalies and pneumonia are common in both term and preterm infants, conditions like Hyaline membrane disease is almost an exclusive disease of the premature infant. Meconium aspiration on the other hand is almost always seen in term infants. (Table 1). Some of these conditions are being briefly discussed.
HYALINE MEMBRANE DISEASE This is the commonest respiratory problem of a premature infant . Nearly 80 % of infants less than 28 weeks develop RDS compared to about 20 % among those between 33 34 weeks gestation. 4 . The increased use of antenatal corticosteroids, have definitely shown to decrease the incidence and severity of HMD 5 . Factors like poorly controlled diabetes in the mother, fetal or perinatal asphyxia, anterpartum hemorrhage in mother and multiple pregnancies 6 increase the chances of RDS in the neonate. The picture of rapidly progressing respiratory distress, manifesting with tachypnea, expiratory grunt, intercostals recession, active accessory muscles of respiration and cyanosis in a premature infant would highlight a diagnosis respiratory distress syndrome. Often the infant is born with a good cry. This forced expiration thru a partially closed glottis generates significant distending pressures to open up most of the alveoli. The
inadequacy of surfactant however results in progressive alveolar collapse. The rapidity of the collapse and the efficacy of respiratory efforts of the infant determining the progression and severity of the clinical features. It is therefore easy to understand the reason for very premature or inadequately resuscitated infants and neonates with severe surfactant deficiency to present immediately after birth with cyanosis and often as respiratory failure.
By 72 to 96 hrs of postnatal age the infant would start generating its own surfactant to increase the compliance of the lung, thereby resulting in natural recovery. Preventing the progression of alveolar collapse during this intervening period therefore forms the basis of all treatment. A heavier less premature infant could probably sustain its alveolar surface area by its own respiratory effort till this dramatic natural turn about of events occur by 72 to 96 hrs of life. More often than not mechanical ventilator support and surfactant replacement are required to tide over the tumultuous initial days of this surfactant deficiency state.
PNEUMONIA
Indian literature attributes pneumonia as the commonest cause for neonates presenting with respiratory distress. 2, 7 . Pneumonia could be acquired due to a transplacental spead of virus or bacteria, or acquired in the perinatal or post natal period. A detailed history to seek out maternal infection or Premature rupture of membranes would therefore be invaluable 8 .
One must always hasten to rule out pneumonia in an infant presenting beyond the 1st few days of life with Tachypnea and difficulty to feed. A decrease in the normal activity of the infants as noticed by the mother would most certainly reinforce this suspicion. Early onset pneumonia is very difficult to distinguish from conditions like HMD more so in the premature infant. While radiological evaluation could help differentiate pneumonia from other conditions, in some cases like group B streptococcal pneumonia even this becomes virtually impossible. Its this authors personal observation systemic features like poor perfusion, metabolic acidosis and altered glucose homeostasis are more common in pneumonia than in hyaline membrane disease. Another clue could be the excessive and thick endotracheal secretion in the 1st day of life --- a feature that is almost never seen in infants being ventilated for hyaline membrane disease.
Early antibiotic therapy with a Penicillin + Aminoglycoside combination, still continues to be the most accepted line of therapy. It must be reinforced that intravenous antibiotics must be commenced without delay. Its the practice to collect blood samples for investigations including blood culture as soon as the infant is admitted and thereof immediately give the first dose of antibiotics as per the policy of the treating unit. Antibiotics can subsequently be tailored according to the culture and sensitivity pattern of the isolates. Supportive therapy with inotropes and ventilator support must be initiated based on the clinical condition of the infant. These play very significant role in the survival of the infant.
MECONIUM ASPIRATION SYNDROME:
Any infant who passes meconium in-utero is at risk for developing meconium aspiration syndrome (MAS). While 10 15 % of all babies could pass meconium before birth, its rare before 37 weeks 9. The passage of meconium could at occasions be an effect of fetal hypoxemia. Occasionally pre-term infants over 34 wks of gestation may pass meconium inutero. The clinical features of these infants are the same as those seen in term infants 4. Therefore a history of meconium stained amniotic fluid is mandatory before attributing the respiratory distress of the neonate to meconium aspiration syndrome.
The consistency of the meconium, adequacy of oro-pharyngeal suction before delivery of shoulder, associated perinatal asphyxia warranting active resuscitation have all been shown to influence the severity of meconium aspiration syndrome 9. The aspirated meconium can completely or partially block the conducting airways leading to segmental or sub-segmental collapse of the lung. The partial block could function as a ball-valve leading to emphysematous changes in the area distal to the obstruction. Rapidity of the resultant distention could lead to airleaks manifesting as pneumothorax. The immediate respiratory distress seen in an infant who has aspirated meconium can therefore easily be attributed to the mechanical effects of meconium. However over the next few hours, diffuse inflammatory responses occur throughout the lung leading to a picture of chemical pneumonitis 9. We have, not uncommonly, noticed such a picture developing even in infants born through thin MSAF who were asymptomatic in the initial period after delivery.
10
The progressive ventilation /perfusion mismatch and inflammatory responses of MAS can lead pulmonary vasoconstriction resulting in persistent pulmonary hypertension of the newborn (PPHN), with its additional morbidity.
The approach to management would be to anticipate MAS in all infants with MSAF.
At Delivery: A good suction of the pharynx before delivery of the shoulders would significantly reduce the chances of meconium aspiration. It was the recommendations of the American Academy of Pediatrics and American Heart Association 10 to undertake endotracheal suction in all infants if there was a (1) Evidence of in utero fetal distress (2) Neonate is depressed or requires positive pressure ventilation in the delivery room (3) Meconium is thick, including moderately thick or particulate in nature (4) if obstetric pharyngeal suction was not performed. However reservations have been expressed about undertaking endotracheal suction in a vigorously crying infant, even in the presence of thick meconium 11. Subsequent management: This phase of management is to evaluate the progression of MAS and to detect and treat promptly the complications like pneumothorax and PPHN. An X-ray of the chest might show patchy non-homogeneous opacities often confluencing towards the mid-zone, with evidence of segmental or subsegmental collapse and areas of hyperaeration. The presence of a pneumothorax must always be looked for. Occasionally the X-ray taken immediately after birth could look apparently normal, but a subsequent film taken over the next 12 24 hours might show diffused haziness, non-homgeneous opacity --- probably reflecting the occurrence of chemical pneumonitis. Infants are
11
more often than not symptomatic during this period. Irrespective of the controversies of endotracheal suction, its best not to forget that even a vigorously crying infant can develop all the meconium associated morbidity. It has therefore been our practice to observe all infants born thru MSAF for at least 24 hrs, keeping an hourly record of the Downes score 3 and continuously monitoring the SaO2 by pulseoximetry. An increasing respiratory distress would imply that the pulmonary functions have been compromised by the mechanical effects of meconium or due to the development of chemical pneumonitis. Occurrence of pneumothorax must always be anticipated. Efforts to rule out pneumothorax must be undertaken especially when, an apparently normal infant with minimal tachypnea, shows increasing respiratory distress, often after an episode of vigorous and active crying. A fibre optic source of light is often used to detect pneumothorax by transilluminating the chest. While a positive transillumination is suggestive of pneumothorax, one must remember that this test could be negative in term infants with thicker skin. A chest X-ray would confirm the presence of pneumothorax. A progressive increase in the clinical score would undoubtedly be the most practical and cost effective way for continuous evaluation. Increasing oxygen demand and a worsening Downes score are ominous signs of a progressive disease.
Fluctuations in the oxygen saturation with the same Fi02, in a quiet infant should arouse the suspicion of pulmonary vascular instability. Such infants must be monitored more carefully, with arterial blood gases from an indwelling arterial catheter. A higher ambient Fi02 could reduce the chances of hypoxemia with its accompanying risk of pulmonary vasoconstriction. 4. Progressive hypoxia, increasing oxygen demands, metabolic or
12
respiratory acidosis, or hypercapnia, should be taken as indications for initiating mechanical ventilation. Its best to prevent an infant from progressing to established PPHN.
Antibiotics are usually not warranted. It is however a common practice of doctors to commence antibiotics, in the presence of abnormal chest-X-ray or respiratory distress 6. This is probably done keeping in mind the differential diagnosis congenital pneumonia. Antibiotics are discontinued with in 48 72 hrs if the respiratory distress settles or if investigations are not suggestive of infection. An uncomplicated MAS normally recovers over 48 72 hrs, rarely being symptomatic beyond the 1st week of life.
PNEUMOTHORAX Pneumothorax can occur in 1 % of all newborns 12 though only 10 % of these are symptomatic. 15 20 % of pneumothoraces are bilateral. An infant with lung disease like MAS & HMD, or those given positive pressure ventilation are more to develop a pneumothorax. The compression of the underlying lung and progressive mediastinal shift to the opposite side pressure result in pulmonary and hemodynamic changes. A sudden increase in cerebral blood flow corresponding to the changes systemic hemodynamics, could cause or increase the bleed in to the germinal matrix or cerebral ventricles 12, especially in premature infants.
13
The occurrence of a pneumothorax must be frequently evaluated in all at risk infants. The clinical presentation could varied. It maybe dramatic with severe respiratory distress, hyperinflated chest, shift in cardiac apex, unilateral decrease in breath sounds, and a positive transillumination. Not uncommonly an infant under treatment for other cause of respiratory distress would develop a pneumothorax. The progression could be fairly gradual. An unexplained increase in heart rate, or gradual drop in blood pressure in an infant with respiratory distress should arouse the suspicion of pneumothorax. More so if the infant is on mechanical ventilator support or required positive pressure resuscitation. Screening for pneumothorax by transilluminating the chest of an at-risk infant at regular intervals have been incorporated in the standard protocol of most neonatal intensive care units.
A chest-Xray would confirm the diagnosis. While the incidentally detected asymptomatic pneumothorax requires no treatment other than close observation, immediate decompression is the rule in all symptomatic patients. Aspiration thru a 21G or 22 G scalp-vein needle inserted in to the 2nd intercostals space in the mid-clavicular line or 5th / 6th inercostal space in the mid-axillary line would temporarily abate symptoms while awaiting preparations for intercostals drain insertion. Insertion of the intercostals catheter under local anesthesia in the 6th intercostals space in the mid-axillary line, connected to an under water sealed drain would satisfactorily drain out the airleak. A negative suction of 10 15 cms of water is often applied to the drainage bottle. In the absence of availability of controlled suction, a vacuum breaker bottle with a 10 15 cm water level can be connected between the ICD bottle and the suction apparatus. If the infant
14
continues to be symptomatic, despite a bubbling ICD, think of a pneumothorax on the opposite side! It must be remembered that if all the clinical features are exclusively due to the pneumothorax, the recovery would also be quite dramatic. However in the presence of an underlying lung disease, improvement in symptoms are significantly influenced by the extent of the primary disease. It is worthwhile to maintain an hourly chart to document the bubbling of the ICD. The catheters are clamped when the ICD has not bubbled for 24 hours. Should the infant deteriorate, the clamp is release to see if there had been any fresh accumulation of pneumothorax.. If there is no clinical worsening, the infant is observed for a 6 -12 hr period and the clamped catheters are removed.
PULMONARY HEMORRHAGE Pulmonary hemorrhage or massive pulmonary hemorrhage in the newborn is not an uncommon manifestation. In majority of cases its a manifestation of massive pulmonary edema. Its seen more often in low birth weight infants. A shunt thru a persistent ductus arteriosus or fluid load could be the main cause of pulmonary hemorrhage in premature infants. We have seen SGA and growth retarded infants presenting with pulmonary hemorrhage. Multiple factors could be contributing to pulmonary hemorrhage in the severely growth retarded infant. Hypothermia, hypoglycemia, thrombocytopenia and sepsis are a commonly encountered combination. The clinical presentation could range from mild tachypnea to severe respiratory distress depending of the severity of the hemorrhage and the ability of the infant to generate distending pressure. A grunt in a growth retarded infant often manifesting beyond the first few hours of life should always
15
arouse the clinical suspicion of pulmonary hemorrhage. The relatively normal activity of the infant and ability to suck at the breast in the near term infant, often contributes to the complacency seen in detecting this condition. Early management with ventilator support with a continuous positive airway pressure (CPAP) of 6 8 cm or intermittent positive pressure ventilation with high PEEP, would effectively control the hemorrhage. More severe the hemorrhage more complicated and less gratifying becomes the ventilator management, with mortality being proportionate to the severity of the bleed and general condition of the infant. If the hemorrhage is due to conditions like PDA, definitive treatment of medically or surgically closing the ductus must be undertaken. .
TRANSIENT TACHYPNEA OF THE NEWBORN (TTN) This is a well recognized entity, attributed to delay in fetal lung fluid clearance. This is a transient phenomenon usually lasting for 6 24 hrs, 4 manifesting with increased respiratory rate, occasionally accompanied by other features of respiratory distress like grunt and cyanosis. Infants rarely require more than 40% Oxygen.. Occasionally the clinical features could persist for 2- 5 days. However under such circumstances it would be more prudent to search for other cause for the respiratory distress. The radiographic findings are non-specific and include prominent vascular markings, pleural and interstitial fluid and prominence of the interlobar fissure 6. The final diagnosis of TTN is always considered after EXCLUDING all other cause for a similar presentation.
PERSISTENT PULMONARY HYPERTENSION OF THE NEWBORN (PPHN)
16
Persistent pulmonary hypertension of the newborn is one of the most challenging conditions of neonatal care. The in-utero status of high pulmonary vascular resistance starts to drop the first cry of the normal infant, a rapid drop seen with in the first minute of birth. The drop in pulmonary pressures continues to occur at a fast pace over the first 24 hrs and then at a more gradual pace up to the 7th 10th post natal day 13. Any factor (TABLE 2) hampering this drop in pulmonary vascular resistance could ensure that the infant continues to retain in-utero features of circulation with its right to left shunt with the resultant associated hypoxemia and cyanosis.
PPHN should be always considered when an at-risk neonate presents with cyanosis often being referred from a peripheral hospital as congenital cyanotic heart disease. Often the clinical presentation could be dominated by the features of the precipitating causes like MAS or Pneumonia. This author feels that under such conditions, hypoxemia disproportionate to the radiological picture would be a good clue to suspect PPHN. Echocardiography could confirm the suspicion.
Once a diagnosis of PPHN is made, the significance of this labile condition and the high associated mortality must be recognized and respected. A dictum of minimal handling, continuous measurement of oxygen saturation (SaO2) by pulse-oximetry or trancutaneous PO2 (TcPO2) monitoring, high ambient oxygen, and arterial blood gas assessment thru an indwelling catheter, maintenance of blood pressure and fluid and electrolyte balance, form the sheet anchor of management. Occasionally SaO2 difference
17
greater than 10% between the right hand and the lower limbs is seen if the PPHN results in a right to left shunt thru a persistent ductus ateriosus. High Fi02 4, 13 contributes to the gradual reduction of the pulmonary vascular resistance. Swings in SaO2 or TcPO2 in a quiet infant without any changes in FiO2 is a good indicator of significant pulmonary vascular lability. Such a labile vasculature could rapidly constrict to an irreversible state under adverse circumstances. Its must therefore be remembered that the FiO2 would have to be weaned very slowly, often at 1-2 % every one two hours. A more rapid or erratic weaning strategy could lead to a disproportionate drop in the PaO2, due to the extremely labile pulmonary vascular physiology. The resultant hypoxemia would further worsen the vasoconstriction and elevate the pulmonary pressure --- leading to a progressive deterioration of the infant. If the oxygenation of the infant continues to deteriorate varied ventilator strategies, addition of inhaled Nitric Oxide (iNO) or ECMO might have to be resorted to. Specifics of these methods would be beyond the purview of this article. Infants would often have to be transported to advanced centers for these modes of treatment.
Transporting a sick infant is a specialized task undertaken by trained neonatal transport teams. In most developing countries such transport facilities are unavailable. It is therefore best to anticipate this eventuality and prepare oneself in advance. This author recommends a dictum of COME for transporting these infant.. Communicate with the referral hospital well before transferring the patient; Ensure appropriate Oxygen delivery to the infant during transport; Minimal handling of infant during transport; Evaluate the
18
clinical condition during transport, preferably with pulseoximetry and cardio-respiratory monitors.
It should be appreciated that adequate ambient oxygen 4 could significantly prevent the labile pulmonary vasculature of the at-risk infant from progressing to an established stage of PPHN.
While an infant treated for PPHN often has normal pulmonary functions at one year of age, the over all outcome is influenced by the etiological cause, duration and mode of therapy required.
STRUCTURAL ANOMALIES Most of these conditions would come under the purview of surgical management. Early recognition of these entities would undoubtedly ensure better management.
Choanal atresia: Bilateral choanal atresia warrants mention here due to its interesting presentation. A infant who is normal and pink when it cries but rapidly develops respiratory distress becomes cyanosed when it stops crying should be evaluated for bilateral choanal atresia. Residents attending the delivery would be the first to be exposed to this perplexing presentation. As neonates are obligate nasal breathers, bilateral choanal obstruction results in their becoming cyanosed when they stop crying. An oral airway would often immediately alleviate the symptoms. Occasionally the presentation would be as respiratory distress while attempting to breast feed.
19
Diagnosis is suspected when one is unable to introduce a nasopharyngeal catheter. CT scan would confirm the diagnosis. Surgical intervention to alleviate the membranous or bony obstruction to the choanae would have to be undertaken with out delay.
Tracheo-esophageal Fistula: (TEF) While a detailed discussion would be beyond the purview of this article, it must be remembered that an early recognition of this condition would dramatically influence the therapeutic outcome. An antenatal history of polyhydraminos may be occasionally available. A clinical suspicion of TEF must be aroused in an infant who continues to pour out oral secretion warranting repeated oral suction. Esophageal atresia associated with the proximal tracheo esophageal connection, would result in the inability of the to swallow its oral secretions. While there is a high chance of the infant aspirating these oropharyngeal secretion, aspiration of gastric secretion through the lower tracheoesophageal communication and resultant pneumonia would further contribute to the morbidity. If undetected at the time of delivery presentation could be as cyanotic episodes associated with feeding, respiratory distress, abdominal distension in the presence of fistula, and a scaphoid abdomen in the presence of pure esophageal atresia.14 . Radiographic evaluation with a gastric tube would demonstrate the absence of the tube in the stomach with the tube getting coiled up at the point of obstruction. Instilling about 5 10 ml of air thru the tube would make it easy to observe these coils of the tube against the air in the esophageal pouch obviating the necessity of a radio-opaque dye. The
20
presence of a gastric bubble is due to the movement of air into the stomach thru the lower tracheo-esophageal connection.
The infant should be kept nil by mouth, with nutrition, fluid and electrolytes requirements being maintained intravenously. The baby should be nursed in a 15 30 degrees head elevated prone or lateral position. The upper pouch should be continuously drained, preferably with minimal continuous suction. Once stabilized the infant must be transferred to the surgical team for further management. The surgical management could vary between an immediate definitive correction OR a feeding gastrostomy with exteriorization of the upper pouch followed by corrective surgery after a few months. These options are based on the anatomy of the anomaly, the general condition of the infant and policies of individual surgical units.
It is not uncommon for other VACTERL group of congenital anomalies to be associated with TEF.
CONGENITAL DIAPHRAGMATIC HERNIA (CDH) Survival of patients with Congenital diaphragmatic hernia have gradually improved over the years. Antenatal diagnosis of CDH has made anticipatory management at delivery and a planned subsequent management a welcome reality. It has been the traditional teaching to rule out diaphragmatic hernia in all neonates presenting with respiratory distress at birth with a cardiac impulse better felt in the right hemithorax. The only
21
differential diagnosis would be a left sided pneumothorax, as rarely does a complex congenital heart disease with dextrocardia present in such a manner. Radiograph of the chest would confirm the diagnosis.
If warranting resuscitation at the time of delivery, this is one of two conditions, the other being MSAF, where positive pressure ventilation thru a mask is discouraged and ventilation is commenced after directly intubating the infant. The associated hypoplasia of the ipsilateral lung, compression of the contralateral lung, and the associated hypoxemia, acidosis and hypercapnia result in these infants having a significant degree of PPHN. No longer is immediate emergency surgery recommended. Instead a period of stabilization with adequate fluid support, maintenance of blood pressure, control of PPHN and ventilatory stability have ensured better surgical outcome. The primary aim of respiratory management is to ensure adequate oxygenation and avoiding acidosis. Various strategies of conventional and high frequency ventilation are adapted for attaining this. It was the aim to try and lower the PaCO2 to acceptable low values by hyperventilation, providing adequate FiO2 and Mean Airway pressure (MAP) for oxygenation. An oxygenation index (OI) greater than 20 at 6 hrs of life, was associated with higher mortality. A modified ventilation index (MVI) greater than 70, (MVI = Respiratory Rate X Peak Inspiratory Pressure X PaCO2/ 1000) was seen to predict 93% mortality with 98 % specificity and 67 % sensitivity 15. However a more gentle way of ventilation with permissive hypercapnia has been shown to be very effective, ensuring survival with minimal pulmonary morbidity 16.
22
Surgical correction is mandatory, though the major determinants of the final outcome would be prenatal factors that affect the development of pulmonary parenchyma, pulmonary vascular bed and surfactant system15. Postoperative care would involve continued ventilator support, strategies to manage the associated PPHN and if warranted extracorporeal membrane oxygenation (ECMO). Follow-up of the survivors is necessary to evaluate and manage respiratory problems and tackle issues of those of feeding, growth and development.
CONGENITAL LOBAR EMPHSEMA: This is a rare but well recognized cause for an infant presenting with respiratory distress anytime within the neonatal period 17. The infant would present with tachypnea, recessions, cyanosis and hyperinflation of the affected side. Breath sounds on the affected side may be diminished. A differential diagnosis of pneumothorax may be considered. A chest X-ray would show hyperinflation of the affected lobe, mediastinal shift to the opposite side and on closer examination would reveal the lung markings --- thus differentiating this from pneumothorax. Definitive surgical treatment of lobectomy should be undertaken without delay.
Intranasal tumours, laryngeal webs, laryngeal cysts, laryngomalacia are few of the anomalies of the upper airway that could present as respiratory distress in the neonatal period. Other rare developmental anomalies like cystic adenomatoid malformation of the lung, congenital pulmonary lymphangectasia etc. could present as neonatal respiratory
23
distress, warranting surgical intervention . The outcome of these conditions depends on the extent of lung involvement and association of other congenital anomalies.
Conclusion Respiratory distress could be a clinical presentation of both pulmonary and nonpulmonary causes. While HMD and congenital pneumonia would be the first differential diagnosis in a preterm infant presenting with these features, pneumonia and meconium aspiration syndrome form a bulk of the respiratory problems in term infants. Its imperative that surgical causes like TEF and CDH be detected early, to optimize the effect of surgical intervention. It must be recognized that the entity of PPHN could complicate all pulmonary conditions presenting during the early first week of life. Early detection and appropriate management is essential to ensure better outcome in all infants presenting with respiratory distress. A systematic approach would useful to confirm the diagnosis and cause for the respiratory distress. (table 3).
24
References 1. National Neonatal Perinatal Data base, report for the year 2000. 2. Mathur NB, Garg K, Kumar S. Respiratory distress in neonates with special reference to pneumonia. Indian Pediatr 2002;39: 529 537 3. Downes JJ, Arya S, Morrow G, Boggs TR. Transient respiratory distress syndrome in the newborn. Arch. Dis.Child. 1967; 42: 659 4. John E, The infant with respiratory problems, in Neonatal Handbook, Sydney, 1st Edn. Editor & Publisher by Elizabeth John, 2000; pp 75 93. 5. Kattner E, Metze B, Waiss E, Obladen M. Accelerated lung maturation following maternal steroid treatment in infants born before 30 weeks gestation., J Perinat Med 1992;20(6):449-57 (Pubmed). 6. Whitsett JA, Pryhuber GS, Rice WR, Warner BB, Wert SE, Acute respiratory disorders, In: Neonatology Pathophysiology & Management of the newborn Eds. Avery GB, Fletcher MA, Macdonald MG. 4th edn. JB Lippincott Company, Philadelphia 1994, 429 452. 7. Khatau SP, Ganfwal A, Basu P, Palodhi PKR, The incidence and etiology of respiratory distress in New born. Indian pediatr 1979; 26.1121-26. 8. Evaldson GR, Malmborg A, Nord CE, Premature rupture of membranes and ascending infection. Br J Obster Gynecol 1982; 89:793 801. 9. Wiswell TE, Bent RC. Meconium staining and meconium aspiration syndrome. Pediatr clinics North Am1993; 40 : 955 981.
25
10. Committee on neonatal ventilation/ meconium / chest compressions: Guidelines proposed at 1992 National Conference on Cardiopulmonary Resuscitation and Emergency cardiac care, Dallas, 1992. JAMA 1992; 268:2276. 11. Wiswell ET, Gannon CM, Jacob J, Goldsmith L, Edgardo S, Weiss K, Schutzman D, et al. Delivery room management of apparently vigorous meconium stained neonate: Results of the multicenter, international collaborative trial. Pediatr 2000;105:1-7. 12. Greenough A, Morley CJ, Roberton NRC. Acute respiratory Diseases in the newborn. In Textbook of Neonatology Ed. Roberton NRC 2nd Edn Churchill Livingstone London 1992; 385 - 504 13. Spitzer AR, Davis J, Clarke WT, Bernbaum J, Fox WW. Pulmonary hypertension and persistent fetal circulation in the newborn. Clinics in Perinatol 1988; 15: 391 413. 14. Dave S, Bajpai M, Gupta DK, Agarwala S, Bhatnagar V, Mitra DK. Esophageal atresia and tracheo-esophageal fistula : A review. Indian J Pediatr 1999; 66: 759 772. 15. Bohn DJ, Pearl Are, Irish MS, Glick PL, Postanatal Management of Congenital diaphragmatic Hernia. Clinics in Perinatol 1996; 23: 843 872. 16. Boloker J, Bateman DA, Wung JT, Stolar CJH. Congenital Diaphragmatic Hernia in 120 infants treated consecutively with permissive hypercapnia / spontaneous respiration/ elective repair. J. Pediatr Surg 2002;35: 357 366. 17. Milner AD, Greenough A. Malformation of the lower respiratory tract. In. Textbook of Neonatology Ed. Roberton NRC 2nd Edn Churchill Livingstone London 1992; 529 546
26
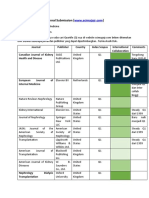
(Table 1) RESPIRATORY DISTRESS IN NEWBORN (adapted with permission from Neonatal Handbook by Elizabeth John 4) Respiratory Distress in Newborn
At birth or soon after birth
Hours to days later
Term
Preterm
Term and Preterm
MAS PPHN
HMD Immature Lung
PPHN Obstructed airways Laryngo tracheomalacia Pneumonia & Sepsis Cardiac Failure Diaphragmatic hernia Pulmonary Hemorrhage
Asphyxia Congenital Pneumonia Transient Tachypnea of the newborn Diaphragmatic hernia Choanal Atresia Aspiration of other matter (eg. Blood or mucus) Pulmonary Hypoplasia Skeletal Anomalies
27
Table 2. Classification Based on Pathophysiology Pulmonary Vasoconstriction Perinatal Asphyxia / Hypoxia Pulmonary Parenchymal Disease Premature in utero ductal closure Decreased Pulmonary Vascular Bed Congenital Pulmonary Hypoplasia Secondary pulmonary hypoplasia eg. Diaphragmatic hernia, Oligohydramnios Increased Pulmonary blood flow associated with congenital heart disease Decreased pulmonary blood flow as in Hyperviscosity syndrome Pulmonary Venous hypertension associated with pulmonary venous obstruction, LVF etc. (with permission from Elizabeth John- Neonatal Handbook 4)
28
Table 3: Approach to Evaluation ANTENATAL Polyhydramnios or oligohydramnio, Cervical incompetence Maternal Illness: Diabetes, PIH, Infections, Maternal medications, antenatal Steroids Antenatal Ultrasound suggestive of anomaly History of Sibling death / similar clinical presentation in sibling. Prolonged / Premature rupture of membranes MSAF, Asphyxia Term or Preterm Time of presentation and progression of Respiratory Distress External congenital anomalies, shape of the chest Tachypnea, Grunt, Cyanosis, Acces. Muscles of Respiration, excessive oral secretions, Hyperinflation of chest, Position of cardiac apex, Breath sounds, Transillumination Normal passage of nasogastric tube Clinical monitoring by Downes score ;
DELIVERY CLINICAL
INVESTIGATION Pulseoximetry : SaO2, Fluctuations of SaO2, Differential SaO2 Chest Xray (with gastric tube in place) Arterial Blood gas. Echocardiography & CT scan if required.
29
Potrebbero piacerti anche
- FamorcaDocumento137 pagineFamorcaStephanie Villanueva Advincula88% (32)
- 3 - Full Pulpotomy With Biodentine in Symptomatic Young Permanent Teeth With Carious Exposure PDFDocumento6 pagine3 - Full Pulpotomy With Biodentine in Symptomatic Young Permanent Teeth With Carious Exposure PDFAbdul Rahman AlmishhdanyNessuna valutazione finora
- Nursing Bullets 5Documento268 pagineNursing Bullets 5kate annNessuna valutazione finora
- Strickland PresentationDocumento1 paginaStrickland Presentationmariopi2495Nessuna valutazione finora
- Case 7 - Newborn With Respiratory DistressDocumento10 pagineCase 7 - Newborn With Respiratory DistressSue HuangNessuna valutazione finora
- Nursing the NeonateDa EverandNursing the NeonateMaggie MeeksNessuna valutazione finora
- Diseases of the Small Intestine in ChildhoodDa EverandDiseases of the Small Intestine in ChildhoodNessuna valutazione finora
- Respiratory Distress Management in NewbornDocumento5 pagineRespiratory Distress Management in Newbornagirl_9807100% (1)
- Division of Perinatology Department of Child Health Medical School University of Sumatera UtaraDocumento37 pagineDivision of Perinatology Department of Child Health Medical School University of Sumatera UtaraJosephine IrenaNessuna valutazione finora
- Gestational Age Related Problems of The Newborn: Carla Reinke, RN, MN, Arnp, CNMDocumento120 pagineGestational Age Related Problems of The Newborn: Carla Reinke, RN, MN, Arnp, CNMsulekhaanoobNessuna valutazione finora
- Keyes Neonatal Emergencies FinalDocumento108 pagineKeyes Neonatal Emergencies FinalthanyunNessuna valutazione finora
- Mechanical Ventilation of The Neonate Principles and StrategiesDocumento6 pagineMechanical Ventilation of The Neonate Principles and StrategiesKelly HoffmanNessuna valutazione finora
- Fetal Distress: Lin Qi de 2005.9.5Documento16 pagineFetal Distress: Lin Qi de 2005.9.5Rendy ChandraNessuna valutazione finora
- Neonatal Emergencies FinalDocumento90 pagineNeonatal Emergencies FinalDr Raseena VattamkandathilNessuna valutazione finora
- Neonates Maternal Drugs Which May Adversely Affect The Newborn BabyDocumento9 pagineNeonates Maternal Drugs Which May Adversely Affect The Newborn BabyAnonymousNessuna valutazione finora
- Neonatal SubgalealDocumento6 pagineNeonatal SubgalealIrenLayNessuna valutazione finora
- Neonatal PharmacologyDocumento61 pagineNeonatal PharmacologyAnaNessuna valutazione finora
- Neonatal SepsisDocumento20 pagineNeonatal SepsisJustine Nyangaresi100% (1)
- Follow-upoftheNICUPatient Medscape FormatDocumento65 pagineFollow-upoftheNICUPatient Medscape FormatJohn ParudaNessuna valutazione finora
- InTech-Neonatal Pneumonia PDFDocumento14 pagineInTech-Neonatal Pneumonia PDFClaudia PalominoNessuna valutazione finora
- Infection in NeonateDocumento28 pagineInfection in Neonateamel015Nessuna valutazione finora
- Case Study #1: HistoryDocumento39 pagineCase Study #1: Historyleonzon_ben442296Nessuna valutazione finora
- Infant and Young Child Feeding: Dr. Malik Shahnawaz AhmedDocumento71 pagineInfant and Young Child Feeding: Dr. Malik Shahnawaz AhmedRiyaz AhamedNessuna valutazione finora
- AARC Clinical Practice Guideline Blood Gas Analysis and Hemoximetry: 2013Documento10 pagineAARC Clinical Practice Guideline Blood Gas Analysis and Hemoximetry: 2013jvalenciagNessuna valutazione finora
- Neonatal ResuscitationDocumento138 pagineNeonatal ResuscitationAbcdeNessuna valutazione finora
- Sepsis Neonatal: Bryan L Ohning, MD, PHD, Clinical Associate Professor of Pediatrics, MedicalDocumento43 pagineSepsis Neonatal: Bryan L Ohning, MD, PHD, Clinical Associate Professor of Pediatrics, Medicalapi-19492580Nessuna valutazione finora
- Perinatal Asphyxia: Walter Otieno Consultant PaediatricianDocumento25 paginePerinatal Asphyxia: Walter Otieno Consultant PaediatricianMalueth AnguiNessuna valutazione finora
- NRP 2011 SummaryDocumento6 pagineNRP 2011 Summaryvanstar7Nessuna valutazione finora
- Neonatal Resuscitation. Advances in Training and PracticeDocumento10 pagineNeonatal Resuscitation. Advances in Training and PracticeFer45Nessuna valutazione finora
- Retinopathy of Prematurity: Aao ReadingDocumento34 pagineRetinopathy of Prematurity: Aao ReadingUNHAS OphthalmologyNessuna valutazione finora
- Golden Hours Management of High Risk Newborns - 2019Documento10 pagineGolden Hours Management of High Risk Newborns - 2019Suryadi LimardiNessuna valutazione finora
- 05 Polycythemia in The NewbornDocumento11 pagine05 Polycythemia in The NewbornMorales Eli PediatraNessuna valutazione finora
- Respiratory DistressDocumento11 pagineRespiratory DistressHina MasoodNessuna valutazione finora
- 9, Procedure of PICCDocumento9 pagine9, Procedure of PICCputriseptinaNessuna valutazione finora
- Physical Growth and Development: Different Aspects and AssessmentDocumento60 paginePhysical Growth and Development: Different Aspects and AssessmentDipti RamiNessuna valutazione finora
- Neonatal PneumoniaDocumento16 pagineNeonatal Pneumoniaelyuchan100% (1)
- Congenital Anomalies of Ureter BladderDocumento17 pagineCongenital Anomalies of Ureter BladderAfiq SabriNessuna valutazione finora
- Neonatal Ventilation PDFDocumento29 pagineNeonatal Ventilation PDFIsabella HosanaNessuna valutazione finora
- Prevention & Treatment of Rop: Presentation: DR Manaswinee Sahoo Guide: DR Swati UpadhyayDocumento42 paginePrevention & Treatment of Rop: Presentation: DR Manaswinee Sahoo Guide: DR Swati Upadhyaypranaya mallNessuna valutazione finora
- Delayed Vs Immediate Umbilical Cord ClampingDocumento37 pagineDelayed Vs Immediate Umbilical Cord ClampingAndi DeviriyantiNessuna valutazione finora
- Non-Cyanotic Congenital Heart Disease-UpDate 4-22-53Documento136 pagineNon-Cyanotic Congenital Heart Disease-UpDate 4-22-53getnusNessuna valutazione finora
- Adjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Documento9 pagineAdjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Edrei Lopez CNessuna valutazione finora
- Ductus Arteriosus Dependent Congenital Heart Disease: Amjad Kouatli MD. FAAP. FACCDocumento28 pagineDuctus Arteriosus Dependent Congenital Heart Disease: Amjad Kouatli MD. FAAP. FACCKartik KumarasamyNessuna valutazione finora
- PREMATURITYDocumento27 paginePREMATURITYHamizi MD HanapiahNessuna valutazione finora
- Assessment and Management of High Risk Neonates DrLawHN PDFDocumento45 pagineAssessment and Management of High Risk Neonates DrLawHN PDFShiva KarthikeyanNessuna valutazione finora
- Neonatal Asphyxia FinalDocumento20 pagineNeonatal Asphyxia FinalAtawna AtefNessuna valutazione finora
- Approach To Sick NeonateDocumento47 pagineApproach To Sick NeonateblitheleevsNessuna valutazione finora
- NRP ppt1Documento29 pagineNRP ppt1sumana BanerjeeNessuna valutazione finora
- Sepsis Management of Neonates With Suspected or Proven Early-Onset BacterialDocumento12 pagineSepsis Management of Neonates With Suspected or Proven Early-Onset BacterialAldo CancellaraNessuna valutazione finora
- Prematurity: DR - Azhar Hamza AlsaqyDocumento18 paginePrematurity: DR - Azhar Hamza AlsaqyChro MANessuna valutazione finora
- Neonatal JaundiceDocumento72 pagineNeonatal JaundiceThya HakimNessuna valutazione finora
- An Approach To Respiratory Distress in NewbornDocumento52 pagineAn Approach To Respiratory Distress in NewbornWira Febrisandi IrsanNessuna valutazione finora
- Theraputic Agent in NeonateDocumento7 pagineTheraputic Agent in Neonateد. محمد فريد الغنامNessuna valutazione finora
- Sickle Cell Anemia PowerpointDocumento29 pagineSickle Cell Anemia Powerpointapi-263353704100% (1)
- Low Birth Weight Baby and HyalineDocumento42 pagineLow Birth Weight Baby and Hyalineakhmad rizky subkiNessuna valutazione finora
- Enteral Feeding of The High Risk NewbornDocumento56 pagineEnteral Feeding of The High Risk NewbornSri SoelistijawatiNessuna valutazione finora
- Bleeding in A NeonateDocumento36 pagineBleeding in A NeonateDrBibek AgarwalNessuna valutazione finora
- Anemia of PrematurityDocumento14 pagineAnemia of PrematurityMariel HuamancayoNessuna valutazione finora
- A Neonate With Acute Kidney Injury: Case PresentationDocumento4 pagineA Neonate With Acute Kidney Injury: Case PresentationSahil DhamijaNessuna valutazione finora
- Respiratory Distress Syndrome: Islamic University Nursing CollegeDocumento21 pagineRespiratory Distress Syndrome: Islamic University Nursing Collegeyaumil agisnaNessuna valutazione finora
- Infants Diabetic MothersDocumento17 pagineInfants Diabetic MothersJaya PrabhaNessuna valutazione finora
- Disseminated Intravascular CoagulationDocumento16 pagineDisseminated Intravascular CoagulationDocRNNessuna valutazione finora
- Birth InjuriesDocumento11 pagineBirth Injuriesdapurna86Nessuna valutazione finora
- Citizens Charter: The Office of The Travancore-Cochin Medical CouncilsDocumento5 pagineCitizens Charter: The Office of The Travancore-Cochin Medical CouncilsabhivnairNessuna valutazione finora
- An Overview of The European Diploma of Anaesthesia and Intensive Care and of Other Important Initiatives of The European Society of AnaesthesiologyDocumento8 pagineAn Overview of The European Diploma of Anaesthesia and Intensive Care and of Other Important Initiatives of The European Society of AnaesthesiologyabhivnairNessuna valutazione finora
- Failure To Thrive Malnutrition Pediatric Outpatient Setting PDFDocumento11 pagineFailure To Thrive Malnutrition Pediatric Outpatient Setting PDFabhivnairNessuna valutazione finora
- AIIMS ProtocolsDocumento5 pagineAIIMS ProtocolsabhivnairNessuna valutazione finora
- LymphadenopathyDocumento2 pagineLymphadenopathyabhivnairNessuna valutazione finora
- Hypoglycemia in The Newborn: AIIMS-NICU Protocols 2010Documento13 pagineHypoglycemia in The Newborn: AIIMS-NICU Protocols 2010abhivnairNessuna valutazione finora
- Blood Transfusion Protocols PDFDocumento5 pagineBlood Transfusion Protocols PDFabhivnairNessuna valutazione finora
- NUR 210 Syllabus and Outline - Summer 2021Documento15 pagineNUR 210 Syllabus and Outline - Summer 2021Penny TratiaNessuna valutazione finora
- Pe103-Course-Guide-And-Module-Sem. 2022-2023Documento55 paginePe103-Course-Guide-And-Module-Sem. 2022-2023Thomas Danjo ManulatNessuna valutazione finora
- IDS - Tuberculosis (Dr. Sy)Documento5 pagineIDS - Tuberculosis (Dr. Sy)Renrenz PayumoNessuna valutazione finora
- 162 319 1 SMDocumento8 pagine162 319 1 SMAsniar RNessuna valutazione finora
- Family Care PlanDocumento3 pagineFamily Care PlanAngie MandeoyaNessuna valutazione finora
- Business Prospect and ProposalDocumento3 pagineBusiness Prospect and ProposalSUBHANKAR GHOSHNessuna valutazione finora
- DR Sandeep Dewan Webinar InvitationDocumento3 pagineDR Sandeep Dewan Webinar InvitationShehbaz ThakurNessuna valutazione finora
- Undangan Seminar Internasional 2021-DikonversiDocumento4 pagineUndangan Seminar Internasional 2021-DikonversiJandi PermadiNessuna valutazione finora
- Bowel Management Following Spinal Cord InjuryDocumento24 pagineBowel Management Following Spinal Cord InjuryBogdan PuscalauNessuna valutazione finora
- Critical Care-Sepsis Case StudyDocumento25 pagineCritical Care-Sepsis Case Studyapi-378305067Nessuna valutazione finora
- What Is Clinical Psychology?: DefinitionsDocumento15 pagineWhat Is Clinical Psychology?: DefinitionsJay Mark CabreraNessuna valutazione finora
- International Profiles of Health Care Systems Dec2020Documento228 pagineInternational Profiles of Health Care Systems Dec2020GODWIN MAYSON LIWANAGNessuna valutazione finora
- Healthcare Fraud in CanadaDocumento28 pagineHealthcare Fraud in CanadaMartin McTaggartNessuna valutazione finora
- Journal SubmissionDocumento3 pagineJournal SubmissionMaruhum Bonar MarbunNessuna valutazione finora
- Reading New E2 PDFDocumento50 pagineReading New E2 PDFMary Jis100% (1)
- Athlete's FootDocumento8 pagineAthlete's Footsneh1509Nessuna valutazione finora
- March 2013 Board of Nursing NoticesDocumento528 pagineMarch 2013 Board of Nursing NoticesJames LindonNessuna valutazione finora
- Society of Radiographers - PDFDocumento9 pagineSociety of Radiographers - PDFOsama AhmedNessuna valutazione finora
- Stress Testing of Drug SubstancesDocumento29 pagineStress Testing of Drug SubstancesMr. HIMANSHU PALIWALNessuna valutazione finora
- Inc Tnai IcnDocumento7 pagineInc Tnai IcnDeena MelvinNessuna valutazione finora
- NATIONAL INSURANCE - National Parivar Mediclaim PolicyDocumento31 pagineNATIONAL INSURANCE - National Parivar Mediclaim PolicyStigan IndiaNessuna valutazione finora
- ResumeDocumento1 paginaResumeapi-353709440Nessuna valutazione finora
- Jurnal KesehatanDocumento17 pagineJurnal KesehatanDiani Rista SariNessuna valutazione finora
- Semmelweis University Brochure ENGDocumento5 pagineSemmelweis University Brochure ENGZita Nemet SeresNessuna valutazione finora
- Assesement of KapDocumento50 pagineAssesement of Kapggdawit80% (5)
- Summative Test in Arts & Health 8 (3rd Grading)Documento4 pagineSummative Test in Arts & Health 8 (3rd Grading)MARIA CRISTINA TEMAJONessuna valutazione finora