Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Try This 20
Caricato da
Khairul MustafaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Try This 20
Caricato da
Khairul MustafaCopyright:
Formati disponibili
general assessment series
Best Practices in Nursing Care to Older Adults
From The Hartford Institute for Geriatric Nursing, New York University, College of Nursing
Issue Number 20, Revised 2012
Editor-in-Chief: Sherry A. Greenberg, PhD(c) MSN, GNP-BC New York University College of Nursing
Preventing Aspiration in Older Adults with Dysphagia
By: Norma A. Metheny, RN, PhD, FAAN, Saint Louis University School of Nursing
WHY: Aspiration (the misdirection of oropharyngeal secretions or gastric contents into the larynx and lower respiratory tract) is common in older adults with dysphagia and can lead to aspiration pneumonia. In fact, it has been suggested that dysphagia carries a sevenfold increased risk of aspiration pneumonia and is an independent predictor of mortality (Singh & Hamdy, 2006). Early recognition of dysphagia and intervention in hospitalized patients is advised to reduce morbidity and use of hospital resources (Altman et al., 2010). TARGET POPULATION: Dysphagia is common in persons with neurologic diseases such as stroke, Parkinsons disease, and dementia. Aspiration occurs in about 40% to 50% of stroke patients with dysphagia (Marik & Kaplan, 2003). The older adult with one of these conditions is at even greater risk for aspiration because the dysphagia is superimposed on the slowed swallowing rate associated with normal aging. Conditions that suppress the cough reflex (such as sedation) further increase the risk for aspiration. BEST PRACTICES: ASSESSMENT AND PREVENTION ASSESSMENT Videofluoroscopy is considered the gold standard to study the mechanisms of dysphagia; if unavailable, fiberoptic endoscopic evaluation may be used instead (Rofes et al., 2011). Others recommend these tests only for patients who fail a reliable clinical swallowing assessment (Leder et al., 2012) Clinical Symptoms of Aspiration: Sudden appearance of respiratory symptoms (such as severe coughing and cyanosis) associated with eating, drinking, or regurgitation of gastric contents. A voice change (such as hoarseness or a gurgling noise) after swallowing. Small-volume aspirations that produce no overt symptoms are common and are often not discovered until the condition progresses to aspiration pneumonia. Aspiration Pneumonia: Older persons with pneumonia often complain of significantly fewer symptoms than their younger counterparts; for this reason, aspiration pneumonia is under-diagnosed in this group. Delirium may be the only manifestation of pneumonia in elderly persons. An elevated respiratory rate is often an early clue to pneumonia in older adults; other symptoms to observe for include fever, chills, pleuritic chest pain and crackles. Observation for aspiration pneumonia should be ongoing in high-risk persons. PREVENTION OF ASPIRATION DURING HAND FEEDING: The following actions may be of some benefit during hand feeding: Provide a 30-minute rest period prior to feeding time; a rested person will likely have less difficulty swallowing. Sit the person upright in a chair; if confined to bed, elevate the backrest to a 90-degree angle. The chin-down or chin-tuck maneuver is widely used in dysphagia treatment, although it does not have a precise anatomical definition (Okada et al., 2007). The extent to which this maneuver is effective is unclear. A recent study of 47 patients with a videofluoroscopic diagnosis of aspiration found only 55% avoided aspiration during the chin-down posture (Terre & Mearin, 2012).Swallowing studies may be needed to determine which individuals are most likely to benefit from this position. Adjust rate of feeding and size of bites to the persons tolerance; avoid rushed or forced feeding. Alternate solid and liquid boluses. Vary placement of food in the persons mouth according to the type of deficit. For example, food may be placed on the right side of the mouth if left facial weakness is present. Determine the food viscosity that is best tolerated by the individual. For example, some persons swallow thickened liquids more easily than thin liquids. However, a recent study found that even in known thin liquid aspirators, offering water did not increase the incidence of aspiration pneumonia (Frey & Ramsberger, 2011). Be aware that some patients may find thickened liquids unpalatable and thus drink insufficient fluids (Colodny, 2005). Minimize the use of sedatives and hypnotics since these agents may impair the cough reflex and swallowing. Medications that dry up secretions should be avoided since they make it more difficult for patients to swallow (Marik, 2011). Evaluate the effectiveness of cueing, redirection, task segmentation and environmental modifications (minimizing distractions) as alternatives to hand feeding. (See Try This: Assessing Eating and Feeding Issues in Older Adults with Dementia).
Permission is hereby granted to reproduce, post, download, and/or distribute, this material in its entirety only for not-for-profit educational purposes only, provided that The Hartford Institute for Geriatric Nursing, New York University, College of Nursing is cited as the source. This material may be downloaded and/or distributed in electronic format, including PDA format. Available on the internet at www.hartfordign.org and/or www.ConsultGeriRN.org. E-mail notification of usage to: hartford.ign@nyu.edu.
PREVENTION OF ASPIRATION DURING TUBE FEEDING: Tube feeding is not necessary for all patients who aspirate (Marik, 2011). However, short-term tube feeding may be needed for elderly patients with severe dysphagia and aspiration in whom improvement of swallowing is likely to occur (Marik, 2011). Results from a clinical trial suggest that patients with dysphagic stroke should be fed early by nasogastric tube and then transitioned to oral feeding as their dysphagia resolves (Dennis et al., 2005). Patients whose dysphagia does not resolve may ultimately require placement of a percutaneous gastrostomy tube. For patients with tube feedings, the following considerations are important: Keep the beds backrest elevated to at least 30 during continuous feedings. When the tube-fed person is able to communicate, ask if any of the following signs of gastrointestinal intolerance are present: nausea, feeling of fullness, abdominal pain or cramping. These signs are indicative of slowed gastric emptying that may, in turn, increase the probability for regurgitation and aspiration of gastric contents. Measure gastric residual volumes every 4 to 6 hours during continuous feedings and immediately before each intermittent feeding. This assessment is especially important when the tube-fed person is unable to communicate signs of gastrointestinal intolerance. There is no convincing research-based information regarding how much gastric residual volume is too much. Use of a promotility agent should be considered when an adult patient has two or more gastric residual volumes 250 ml (Bankhead et al., 2009). The incidence of pneumonia is not different in patients with nasogastric tubes and percutaneous endoscopic tubes (Gomes et al., 2010). However, a gastrostomy tube is more comfortable for the patient than is prolonged use of a nasogastric tube. PREVENTION OF ASPIRATION PNEUMONIA BY ORAL CARE: Missing teeth and poorly fitted dentures predispose to aspiration by interfering with chewing and swallowing. Infected teeth and poor oral hygiene predispose to pneumonia following the aspiration of contaminated oral secretions. Tube feeding in elderly persons is associated with significant pathogenic colonization of the mouth, more so than that observed in those who received oral feedings. There is evidence that providing regular dental care and cleaning the elder persons teeth with a toothbrush after each meal lowers the risk of aspiration pneumonia. Development and maintenance of an oral hygiene program is a critical step in preventing pneumonia in nursing home residents (El-Solh, 2011). MORE ON THE TOPIC: Best practice information on care of older adults: www.ConsultGeriRN.org. Altman, K.W., Yu, G.P., & Schaefer, S.D. (2010). Consequence of dysphagia in the hospitalized patient: Impact on prognosis and hospital resources. Archives of Otolaryngology-Head & Neck Surgery, 136(8), 784-789. Bankhead, R., Boullata, J., Brantley, S., Corkins, M., Guenter, P., Krenitsky, J., Lyman, B., Metheny, N.A., Mueller, C., Robbins, S., Wessel, J., & A.S.P.E.N. Board of Directors. (2009). A.S.P.E.N. enteral nutrition practice recommendations. Journal of Parenteral and Enteral Nutrition. 33(2), 122-167. doi: 10.1177/0148607108330314 Colodny, N. (2005). Dysphagic independent feeders justifications for noncompliance with recommendations by a speech-language pathologist. American Journal of Speech-Language Pathology, 14(1), 61-70. Dennis, M.S., Lewis, S.C., & Warlow, C. (2005). Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): A multicentre randomized controlled trial. Lancet, 365, 764-772. El-Solh, A.A. (2011). Association between pneumonia and oral care in nursing home residents. Lung. 189(3), 173-180. Frey, K.L. & Ramsberger, G. (2011). Comparison of outcomes before and after implementation of a water protocol for patients with cereberovascular accident and dysphagia. Journal of Neuroscience Nursing, 43(3), 165-171. Gomes, C.A., Lustosa, S.A., Matos, D., Andriolo, R.B., Waisberg, D.R., & Waisberg, J. (2010). Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database of Systematic Reviews. (11)DC008096. Leder, S.B., Suiter, D.M., Warner, H.L., Acton, L.M., & Swainson, B.A. (2012). Success of recommending oral diets in acute stroke patients based on passing a 90-cc water swallow challenge protocol. Topics in Stroke Rehabilitation, 19(1), 40-44. Marik, P.E. (2011). Pulmonary aspiration syndrome. Current Opinion in Pulmonary Medicine, 17, 148-154. Marik, P.E., & Kaplan, D. (2003). Aspiration pneumonia and dysphagia in the elderly. Chest, 124, 328-336. Okada, S., Saitoh, E., Palmer, J.B., Matsuo, K., Yokoyama, M., Shigeta, R., & Baba, M. (2007). What is the chin-down posture? A questionnaire survey of speech language pathologist in Japan and the United States. Dysphagia, 22(3), 204-209. Rofes, L., Arreloa, V., Almirall, J., Cabre, M., Campins, L., Garcia-Peris, P., Speyer, R., & Clave P. (2011). Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterology Research and Practice. Volume 2011, 1-13. doi:10.1155/2011/818979 Singh, S., & Hamdy, S. (2006). Dysphagia in stroke patients. Postgraduate Medical Journal, 82(968), 383-391. Terre, R., & Mearin, F. (2012). Effectiveness of chin-down posture to prevent tracheal aspiration in dysphagia secondary to acquired brain injury. A videofluoroscopy study. Neurogastroenterology & Motility, 24(5), 414-419.
general assessment series
Best Practices in Nursing Care to Older Adults
A series provided by The Hartford Institute for Geriatric Nursing, New York University, College of Nursing
EMAIL CLINICAL NURSING WEBSITE
hartford.ign@nyu.edu HARTFORD INSTITUTE WEBSITE www.hartfordign.org www.ConsultGeriRN.org
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- 5 PBDocumento10 pagine5 PBKhairul MustafaNessuna valutazione finora
- 07-3 Biopiracy Imitations Not InnovationsDocumento76 pagine07-3 Biopiracy Imitations Not InnovationsKhairul MustafaNessuna valutazione finora
- National Descriptors Texture Modification AdultsDocumento21 pagineNational Descriptors Texture Modification AdultsKhairul MustafaNessuna valutazione finora
- Antibiotic Prophylaxis in Surgery: Module MenuDocumento5 pagineAntibiotic Prophylaxis in Surgery: Module MenuKhairul MustafaNessuna valutazione finora
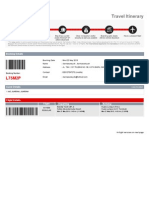
- Travel Itinerary: Booking DetailsDocumento5 pagineTravel Itinerary: Booking DetailsKhairul MustafaNessuna valutazione finora
- 2 Family+MedicineDocumento23 pagine2 Family+MedicineKhairul MustafaNessuna valutazione finora
- 1principlesof FMDocumento26 pagine1principlesof FMKhairul MustafaNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- IDL Tubex TestDocumento5 pagineIDL Tubex TestMaya RustamNessuna valutazione finora
- CBCT-Scan in DentistryDocumento24 pagineCBCT-Scan in DentistryBilly Sam80% (5)
- Ectopic Pregnancy Nursing Care PlansDocumento27 pagineEctopic Pregnancy Nursing Care Plansviper7967880% (20)
- Triage Assessment of Psychiatric Patient LectureDocumento31 pagineTriage Assessment of Psychiatric Patient Lectureهشام عفانه100% (1)
- Functional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVDocumento20 pagineFunctional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVwenyinriantoNessuna valutazione finora
- Contact Nummular (Discoid) Eczema From Depilating Cream: Case ReportDocumento2 pagineContact Nummular (Discoid) Eczema From Depilating Cream: Case ReportMorindaNessuna valutazione finora
- Pelatihan Pembuatan Sabun Cuci Tangan Anti Bakteri Berbasis Eco Enzym Dari Limbah Buah-Buahan Dan SayuranDocumento9 paginePelatihan Pembuatan Sabun Cuci Tangan Anti Bakteri Berbasis Eco Enzym Dari Limbah Buah-Buahan Dan Sayuran11Dehan Avino Aurisky AqilaNessuna valutazione finora
- Chronic Limb Ischaemia: MR Hanif Hussein Consultant Vascular Surgeon, HKLDocumento35 pagineChronic Limb Ischaemia: MR Hanif Hussein Consultant Vascular Surgeon, HKLZulzaire ZulkefliNessuna valutazione finora
- Hemotology ReviewDocumento61 pagineHemotology ReviewSukma EffendyNessuna valutazione finora
- Literature Review Ectopic PregnancyDocumento4 pagineLiterature Review Ectopic Pregnancyakjnbowgf100% (1)
- Abdul Malik Hassim Lecturer DMA Management & Science UniversityDocumento21 pagineAbdul Malik Hassim Lecturer DMA Management & Science UniversitykimmgizelleNessuna valutazione finora
- FCPS SurgeryDocumento106 pagineFCPS Surgeryrehan hayderNessuna valutazione finora
- Dog Bite Show NotesDocumento5 pagineDog Bite Show NotesLakshay ChananaNessuna valutazione finora
- Acne Keloidalis NuchaeDocumento16 pagineAcne Keloidalis NuchaejalalfaizNessuna valutazione finora
- Vaccination Certificate 20435699572410Documento1 paginaVaccination Certificate 20435699572410MANOJ BHADANENessuna valutazione finora
- Chapter 11 Obesity and NutritionDocumento14 pagineChapter 11 Obesity and NutritionAlan ShimNessuna valutazione finora
- SWAN Parkinson MRIDocumento9 pagineSWAN Parkinson MRIulfi yunitaNessuna valutazione finora
- Ophthalmology: Cycloplegic Refraction in Children With Cyclopentolate Versus AtropineDocumento6 pagineOphthalmology: Cycloplegic Refraction in Children With Cyclopentolate Versus AtropineKiara NurmathiasNessuna valutazione finora
- 2014 @nucproflib Helen Ryder, GiorgioDocumento128 pagine2014 @nucproflib Helen Ryder, Giorgioe'Rfan k'AguyaNessuna valutazione finora
- 2003 HemaDocumento19 pagine2003 Hemahavana1975Nessuna valutazione finora
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocumento6 pagineAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationRenea Joy ArruejoNessuna valutazione finora
- Risk For Infection Related To Presence of Surgical Wounds As Evidenced by MER 2nd DegreeDocumento3 pagineRisk For Infection Related To Presence of Surgical Wounds As Evidenced by MER 2nd DegreeSenyorita KHaye75% (12)
- Malunggay Leaf ResearchDocumento3 pagineMalunggay Leaf ResearchEj KasimNessuna valutazione finora
- Intrapartum HandoutDocumento29 pagineIntrapartum HandoutZahNessuna valutazione finora
- The Pediatric Physical Exam:: Who, When, What and Why?Documento26 pagineThe Pediatric Physical Exam:: Who, When, What and Why?Carlo Emmanuel SantosNessuna valutazione finora
- Disorders of The Adrenal Glands: Adrenal Cortical Adenoma and CarcinomaDocumento9 pagineDisorders of The Adrenal Glands: Adrenal Cortical Adenoma and Carcinomahussain AltaherNessuna valutazione finora
- Sugar and Blood 2Documento19 pagineSugar and Blood 2shaira ubaldeNessuna valutazione finora
- Prostaglandins in Pregnancy: Scott W. Walsh, PHDDocumento21 pagineProstaglandins in Pregnancy: Scott W. Walsh, PHDIrene AtimNessuna valutazione finora
- Types of Feeding-GastrostomyDocumento8 pagineTypes of Feeding-GastrostomyElda KuizonNessuna valutazione finora
- Acute Rheumatic FeverDocumento39 pagineAcute Rheumatic FeverUzma BanoNessuna valutazione finora