Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Disorders of Cranial Nerves
Caricato da
theglobalnursingTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Disorders of Cranial Nerves
Caricato da
theglobalnursingCopyright:
Formati disponibili
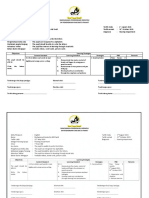
DISORDERS OF CRANIAL NERVES
Disorder Nursing Olfactory NerveI Head trauma Intracranial tumor Intracranial surgery Optic NerveII Optic neuritis Increased intracranial pressure Pituitary tumor Oculomotor NerveIII Trochlear NerveIV Abducens NerveVI Vascular Brain stem ischemia Hemorrhage and infarction Neoplasm Trauma Infection Clinical Manifestations Unilateral or bilateral anosmia (temporary or persistent) Diminished taste for food Lesions of optic tract producing homonymous hemianopsia Interventions Assess sense of smell. Assess for cerebrospinal uid rhinorrhea if patient has sustained head trauma. Assess visual acuity. Restructure environment to prevent injuries. Teach patient to accommodate for visual loss.
Dilation of pupil with loss of light reex on one side Impairment of ocular movement Diplopia Gaze palsies Ptosis of eyelid
Assess extraocular movement and for nonreactive pupil.
Trigeminal NerveV Trigeminal neuralgia Head trauma Cerebellopontine lesion Sinus tract tumor and metastatic disease Compression of trigeminal root by tumor
Pain in face Diminished or loss of corneal reex Chewing dysfunction
Assess for pain and triggering mechanisms for pain. Assess for difculty in chewing. Discuss trigger zones and pain precipitants with patient. Protect cornea from abrasion. Ensure good oral hygiene. Educate patient about medication regimen. Recognize facial paralysis as emergency; refer for treatment as soon as possible. Teach protective care for eyes. Select easily chewed foods; patient should eat and drink from unaffected side of mouth. Emphasize importance of oral
Facial NerveVII Bells palsy Facial nerve tumor Intracranial lesion Herpes zoster
Facial dysfunction; weakness and paralysis Hemifacial spasm Diminished or absent taste Pain
hygiene. Provide emotional support for changed appearance of face. Vestibulocochlear NerveVIII Tumors and acoustic neuroma Vascular compression of nerve Mnires syndrome Tinnitus Vertigo Hearing difculties Assess pattern of vertigo. Provide for safety measures to prevent falls. Ensure that patient can maintain balance before ambulating. Caution patient to change positions slowlyAssist with ambulation. Encourage use of assistive devices. Assess for paroxysmal pain in throat, decreased or absent swallowing, and gag and cough reexes. Monitor for dysphagia, aspiration, and nasal dysarthric speech. Position patient upright for eating or tube feeding.
Glossopharyngeal NerveIX Glossopharyngeal neuralgia from neurovascular compression of cranial nerves IX and X Trauma Inammatory conditions Tumor Vertebral artery aneurysms
Pain at base of tongue Difculty in swallowing Loss of gag reex Palatal, pharyngeal, and laryngeal paralysis
Vagus NerveX Spastic palsy of larynx; bulbar paralysis; high vagal paralysis Guillain-Barr syndrome Vagal body tumors Nerve paralysis from malignancy, surgical trauma such as carotid endarterectomy Spinal Accessory NerveXI Spinal cord disorder Amyotrophic lateral sclerosis Trauma Guillain-Barr syndrome
Voice changes (temporary or permanent hoarseness) Vocal paralysis Dysphagia
Assess for airway obstruction/provide airway management. Prevent aspiration. Support patient having voice reconstruction procedures.
Drooping of affected shoulder with limited shoulder movement Weakness or paralysis of head rotation, exion, extension; shoulder elevation
Support patient undergoing diagnostic tests.
Hypoglossal NerveXII Medullary lesions Amyotrophic lateral sclerosis Polio and motor system disease, which may destroy hypoglossal nuclei Multiple sclerosis Trauma
Abnormal movements of tongue Weakness or paralysis of tongue muscles Difculty in talking, chewing, and swallowing
Observe swallowing ability. Observe speech pattern. Be aware of swallowing or vocal difculties. Prepare for alternate feeding methods (tube feeding) to maintain nutrition.
Source:Brunner and Suddharths Med-Surgical Nursing 12th Edition p.1971
Potrebbero piacerti anche
- Cranial Nerves SummaryDocumento3 pagineCranial Nerves SummaryJoash F. Pacquing75% (4)
- Cranial NervesDocumento14 pagineCranial NervesIrina Garlea-Robu100% (1)
- Pathognomonic SignsDocumento12 paginePathognomonic Signsclarice_jimenezNessuna valutazione finora
- Musculoskeletal DISORDERSDocumento6 pagineMusculoskeletal DISORDERSJoe Stewart100% (1)
- Cranial Nerves: DR Dyan Roshinta Laksmi Dewi, SP.S SMF Saraf Rsud DR Soedarso PontianakDocumento19 pagineCranial Nerves: DR Dyan Roshinta Laksmi Dewi, SP.S SMF Saraf Rsud DR Soedarso PontianakVidia AsriyantiNessuna valutazione finora
- Patients With Hearing and Balance DisordersDocumento33 paginePatients With Hearing and Balance Disordershalloween candyNessuna valutazione finora
- Neurologic Disorders - NCM 102 LecturesDocumento12 pagineNeurologic Disorders - NCM 102 LecturesBernard100% (4)
- Gastrointestinal Nclex Questions Part 2Documento11 pagineGastrointestinal Nclex Questions Part 2Manilyn Delos Reyes Patlunag100% (1)
- Cranial NervesDocumento17 pagineCranial Nervesdankirsh100% (17)
- The GastroDocumento25 pagineThe Gastroangel_maui100% (7)
- Med Surg NotesDocumento64 pagineMed Surg NotesRAYMUND IAN ABALOS100% (2)
- Endocrine DisordersDocumento3 pagineEndocrine DisordersIrish OrleansNessuna valutazione finora
- MnemonicsDocumento4 pagineMnemonicsKarol Delagana67% (3)
- Neurologic DisordersDocumento51 pagineNeurologic DisordersYamSomandar100% (1)
- Endocrine SystemDocumento8 pagineEndocrine Systemtheglobalnursing80% (5)
- Physical Examination: Binal Joshi Assistant Professor Child Health Nursing Manikaka Topawala Institute of NursingDocumento101 paginePhysical Examination: Binal Joshi Assistant Professor Child Health Nursing Manikaka Topawala Institute of NursingBinal JoshiNessuna valutazione finora
- MedSurg NeuroDocumento8 pagineMedSurg NeuroZachary T Hall100% (1)
- Neuro Lecture NotesDocumento41 pagineNeuro Lecture Notescziel23Nessuna valutazione finora
- Cranial NervesDocumento2 pagineCranial Nervescrsoriano2011Nessuna valutazione finora
- Spinal Cord InjuryDocumento17 pagineSpinal Cord InjuryTom MallinsonNessuna valutazione finora
- MnemonicsDocumento23 pagineMnemonicsJot grewalNessuna valutazione finora
- Mnemonics - ClinicalDocumento16 pagineMnemonics - Clinicalkavidi100% (1)
- Exam 2 - Neurological Study GuideDocumento10 pagineExam 2 - Neurological Study GuideStephanieNessuna valutazione finora
- Onco PharmacologyDocumento9 pagineOnco Pharmacologyarn0ld21Nessuna valutazione finora
- Common Signs and Symptoms of DiseasesDocumento88 pagineCommon Signs and Symptoms of DiseasesAbdul QuyyumNessuna valutazione finora
- Cranial NervesDocumento3 pagineCranial Nervesjulialeo100% (1)
- Handout OB MidtermsDocumento3 pagineHandout OB Midtermsaidan valin100% (7)
- Pharmacology Study Notes - Adrenergic DrugsDocumento2 paginePharmacology Study Notes - Adrenergic Drugsstuckaluck83% (6)
- Endocrine Pathophysiology Nursing Notes - Part 2Documento10 pagineEndocrine Pathophysiology Nursing Notes - Part 2grad_nurse_2015100% (1)
- Neuro Nursing-Seizure DisorderDocumento8 pagineNeuro Nursing-Seizure DisorderBell Jose50% (4)
- Endocrine NursingDocumento8 pagineEndocrine NursingBunny Bonny100% (5)
- Health AssessmentDocumento15 pagineHealth AssessmentrlinaoNessuna valutazione finora
- Hema, Onco, Cardiology Review NotesDocumento9 pagineHema, Onco, Cardiology Review Notesjeshema100% (1)
- Oncology NursingDocumento4 pagineOncology Nursingfairwoods100% (2)
- Endocrine System Review NotesDocumento8 pagineEndocrine System Review Notesjeshema100% (1)
- Pathology Lecture SeriesDocumento168 paginePathology Lecture SeriesButch DumdumNessuna valutazione finora
- Respirotary MnemonicsDocumento9 pagineRespirotary MnemonicsAymen Omer0% (1)
- Neuro Study GuideDocumento7 pagineNeuro Study GuideNursingSchoolNotes100% (2)
- Neuro NursingDocumento22 pagineNeuro Nursingheiyu100% (6)
- Med Surg A Neuro PPT 120515134413541 5Documento93 pagineMed Surg A Neuro PPT 120515134413541 5Sapiah RamanNessuna valutazione finora
- Nervous SystemDocumento10 pagineNervous Systemshenric16Nessuna valutazione finora
- Histology Lec-11 EndocrineDocumento10 pagineHistology Lec-11 EndocrineKevin C. AguilarNessuna valutazione finora
- Cranial Nerve AssessmentDocumento4 pagineCranial Nerve AssessmentAnonymous h2EnKyDbNessuna valutazione finora
- Endocrine Pathophysiology Nursing NotesDocumento4 pagineEndocrine Pathophysiology Nursing Notesgrad_nurse_2015100% (2)
- Fundamentals of Nursing: Prof. Ma. Teresa Pimentel-VanguardiaDocumento27 pagineFundamentals of Nursing: Prof. Ma. Teresa Pimentel-VanguardiaMaria Garcia Pimentel Vanguardia IINessuna valutazione finora
- 12 Cranial Nerves and AssessmentDocumento10 pagine12 Cranial Nerves and Assessmentapollo100% (17)
- Medical Surgical: Nervous SystemDocumento90 pagineMedical Surgical: Nervous SystemCatherine G. Borras100% (1)
- Summary of Cranial NervesDocumento1 paginaSummary of Cranial NervesjackieNessuna valutazione finora
- CardioDocumento10 pagineCardioMar OrdanzaNessuna valutazione finora
- Male Reproductive System and DiseasesDocumento10 pagineMale Reproductive System and DiseasesMadan Kumar100% (2)
- Neuro DisordersDocumento13 pagineNeuro DisordersMicz Celiz100% (3)
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Vertigo and DizzinessDocumento50 pagineVertigo and DizzinessRyanIndraSaputraNessuna valutazione finora
- Document 32Documento3 pagineDocument 32Play ListNessuna valutazione finora
- Lower Cranial NervesDocumento83 pagineLower Cranial NervesVamsi KrishnaNessuna valutazione finora
- Isolated Third Nerve PalsyDocumento4 pagineIsolated Third Nerve PalsySora KerovaNessuna valutazione finora
- Birthinjuries Dr.M.maniDocumento65 pagineBirthinjuries Dr.M.manimaniNessuna valutazione finora
- Neurological Disorders Key NotesDocumento31 pagineNeurological Disorders Key NotesHannah aswiniNessuna valutazione finora
- Final - Im Ward PresentationDocumento6 pagineFinal - Im Ward PresentationElla MuskNessuna valutazione finora
- Major Fluid and Electrolyte ImbalancesDocumento5 pagineMajor Fluid and Electrolyte ImbalancestheglobalnursingNessuna valutazione finora
- Perioperative NursingDocumento12 paginePerioperative Nursingtheglobalnursing100% (12)
- Summary Differences Between Dementia and DeliriumDocumento4 pagineSummary Differences Between Dementia and Deliriumtheglobalnursing100% (1)
- NLE 12-2012 ResultsDocumento359 pagineNLE 12-2012 ResultsPRC Baguio0% (2)
- Common Eye Problems in ChildrenDocumento6 pagineCommon Eye Problems in ChildrentheglobalnursingNessuna valutazione finora
- Congenital Heart DiseasesDocumento6 pagineCongenital Heart Diseasestheglobalnursing100% (2)
- Expanded Program On ImmunizationDocumento1 paginaExpanded Program On ImmunizationtheglobalnursingNessuna valutazione finora
- Emergency Management of Patients With Drug OverdoseDocumento6 pagineEmergency Management of Patients With Drug Overdosetheglobalnursing0% (1)
- Common Signs and Symptoms of Diseases (Pathognomonic Sign)Documento3 pagineCommon Signs and Symptoms of Diseases (Pathognomonic Sign)theglobalnursing91% (11)
- Disorders of The Lips, Mouth and GumsDocumento5 pagineDisorders of The Lips, Mouth and GumstheglobalnursingNessuna valutazione finora
- Gastrointestinal SystemDocumento8 pagineGastrointestinal Systemtheglobalnursing100% (1)
- Musculoskeletal System Nursing ReviewerDocumento11 pagineMusculoskeletal System Nursing Reviewerposh003850% (2)
- Fundamentals of NursingDocumento44 pagineFundamentals of Nursingtheglobalnursing100% (2)
- Cardiovascular SystemDocumento10 pagineCardiovascular Systemtheglobalnursing75% (4)
- Pyschiatric NursingDocumento40 paginePyschiatric Nursingtheglobalnursing100% (1)
- Respiratory SystemDocumento9 pagineRespiratory Systemtheglobalnursing89% (9)
- Neurologic NursingDocumento14 pagineNeurologic Nursingtheglobalnursing100% (6)
- Endocrine SystemDocumento8 pagineEndocrine Systemtheglobalnursing80% (5)
- Maternal and Child NursingDocumento63 pagineMaternal and Child Nursingtheglobalnursing100% (1)
- Community Health NursingDocumento9 pagineCommunity Health NursingtheglobalnursingNessuna valutazione finora
- Notes of CH 7 Control and Coordination - Class 10th Science Study RankersDocumento9 pagineNotes of CH 7 Control and Coordination - Class 10th Science Study Rankerssamy0% (1)
- Transcranial Magnetic Stimulation: Rachel Mcateer Bme 281Documento12 pagineTranscranial Magnetic Stimulation: Rachel Mcateer Bme 281ANTolaniNessuna valutazione finora
- Principles of Anatomy and Physiology: 14 EditionDocumento62 paginePrinciples of Anatomy and Physiology: 14 EditionWilliam C Chisha100% (1)
- Sindrome de FregoliDocumento3 pagineSindrome de FregoligabacorreaNessuna valutazione finora
- Test Nuro 2Documento11 pagineTest Nuro 2Litsa XeimariouNessuna valutazione finora
- Red, Yellow and Green Flags For Low Back Pain: For Serious Underlying DiseaseDocumento1 paginaRed, Yellow and Green Flags For Low Back Pain: For Serious Underlying DiseaseShafira DianiNessuna valutazione finora
- Modified Ashworth Scale Instructions PDFDocumento3 pagineModified Ashworth Scale Instructions PDFIndah BerlianaNessuna valutazione finora
- PHYSIO PSY Worksheet 1 - Article Reading. The Brain The Mystery of Consciousness Printout by TIMEDocumento8 paginePHYSIO PSY Worksheet 1 - Article Reading. The Brain The Mystery of Consciousness Printout by TIMEKissieNessuna valutazione finora
- ANPH Midterm NotesDocumento44 pagineANPH Midterm NotesClaudine Jo B. TalabocNessuna valutazione finora
- Neural Network PDFDocumento3 pagineNeural Network PDFSUREKHA SNessuna valutazione finora
- Physiology of VisionDocumento49 paginePhysiology of VisionPrakash PanthiNessuna valutazione finora
- Simon Humphreys 8july15Documento45 pagineSimon Humphreys 8july15Pudu MounikaNessuna valutazione finora
- ASD Comparison Information Brief PDFDocumento6 pagineASD Comparison Information Brief PDFMaryam BehramNessuna valutazione finora
- Rancangan Pendidikan Individu SK Pendidikan Khas Batu PahatDocumento2 pagineRancangan Pendidikan Individu SK Pendidikan Khas Batu PahatKOH KIAN NGEE MoeNessuna valutazione finora
- Dissociation and Dissociative Disorders (Review)Documento6 pagineDissociation and Dissociative Disorders (Review)Carolina ValenciaNessuna valutazione finora
- ABC ChecklistDocumento1 paginaABC ChecklistSameer Samoua100% (1)
- Wearing On Her Nerves Case Study - Werner Williams Mccool Floyd AhmadDocumento50 pagineWearing On Her Nerves Case Study - Werner Williams Mccool Floyd Ahmadapi-320365850100% (2)
- NCP LeonilaDocumento2 pagineNCP LeonilarhoinezaNessuna valutazione finora
- Schwann Cells PowerpointDocumento16 pagineSchwann Cells PowerpointabibtdottyNessuna valutazione finora
- Kooij, 2010 TDAH Diag Adul Eur en Ingles PDFDocumento24 pagineKooij, 2010 TDAH Diag Adul Eur en Ingles PDFMalka SarmientoNessuna valutazione finora
- Application of OMAHA System of Community DiagnosisDocumento5 pagineApplication of OMAHA System of Community DiagnosisEula Angelica OcoNessuna valutazione finora
- Humor For Good Health: Presented By: Michael Brodie, MBA, NHADocumento32 pagineHumor For Good Health: Presented By: Michael Brodie, MBA, NHAYuva Lakshmi Ramesh BabuNessuna valutazione finora
- 3CNCPDocumento7 pagine3CNCPHelen MontesNessuna valutazione finora
- Kleptomania: Recent Advances in Symptoms, Etiology and TreatmentDocumento4 pagineKleptomania: Recent Advances in Symptoms, Etiology and TreatmentHelwa SalsabelaNessuna valutazione finora
- Proprioceptive Pathway: ObjectivesDocumento17 pagineProprioceptive Pathway: ObjectivesHuyền ĐinhNessuna valutazione finora
- 10.5 Speed of The Nerve ImpulseDocumento23 pagine10.5 Speed of The Nerve ImpulsequinNessuna valutazione finora
- Brain Processing of Rectal Sensation in Adolescents With Functional Defecation Disorders and Healthy ControlsDocumento11 pagineBrain Processing of Rectal Sensation in Adolescents With Functional Defecation Disorders and Healthy ControlsDaniela Rodríguez MartínezNessuna valutazione finora
- Biological Causes For AggressionDocumento7 pagineBiological Causes For Aggressionblah100% (1)
- Effectiveness Of: Transcranial Magnetic StimulationDocumento20 pagineEffectiveness Of: Transcranial Magnetic StimulationRaluca ComanescuNessuna valutazione finora
- Paper D (KMU) 2nd Year - 0Documento2 paginePaper D (KMU) 2nd Year - 0G.R. JamesNessuna valutazione finora