Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Dosage - Chapter 11
Caricato da
kaukau4everDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Dosage - Chapter 11
Caricato da
kaukau4everCopyright:
Formati disponibili
Pharmaceutical Dosage Chapter 11: Transdermal Drug Delivery Systems Topical Dermatological Products Drugs delivered into the
the skin for treatment of dermal disorders For local effects Skin as the target organ
Factors Affecting Percutaneous Absorption Physical and chemical properties of drugs including its molecular weight, solubility, partition coefficient, and dissociation constant, the nature of the carrier vehicle, and the conditioning of the skin Drug concentration Area of application: the larger, the more drug is absorbed Greater physiochemical attraction to the skin than to the vehicle Can permeate skin: with molecular weights ranging from 100 to 800 (ideal molecular weight for TDDS: 400 or less) and adequate lipid and aqueous solubility Hydration of the skin favors percutaneous absorption Site with a thin horny layer than with a thick one The longer the medicated application is permitted to remain in contact with the skin and the greater is the total drug absorption
Transdermal Products Drugs delivered through the skin (percutaneous absorption) to the general circulation For systemic effects Skin: not the target organ
Transdermal Drug Delivery System (TDDS) Facilitate the passage of therapeutic quantities of drug substances through the skin and into the general circulation for their systemic effects Transderm scop First transdermal (Ciba, now Novartis) approved by the FDA in 1979 Prevents motion sickness, nausea, and vomiting resulting from the use of certain anesthetics
Cadaver Skin Permeation Testing Helps determine the feasibility of a compound to be incorporated into a TDDS
Chemical Enhancers Chemical skin permeation enhancer: increases skin permeability by damaging or altering the physiochemical nature of the stratum corneum to reduce its diffusion substance Among the alterations of the stratum corneum are: Increased hydration of the stratum corneum Change in the structure of lipids and lipoproteins in the intercellular channels through solvent action or denaturation or both Some drugs inherent capacity to permeate the skin without chemical enhancer. Chemical permeation enhancer: render impenetrable substance useful in TDDS More than 275 chemical compounds have cited as skin penetration enhancers that include: acetone, azone, dimethyl acetamide, dimethly formamide, dimethyl sulfoxide, ethanol, oleic acid, PEG, PG, and sodium lauryl sulfate
Evidences of Percutaneous Drug Absorption Evidences of percutaneous drug absorption Measurable blood levels of the drug Detectable excretion of the drug and/or its metabolites in the urine Clinical response of the patient to the therapy Blood concentration needed to achieve (with TDDS) therapeutic efficacy determined by: Comparative analysis of the patients response to the drug blood levels Ideal for the drug To migrate through the skin: blood supply without build up in the dermal layers
Stratum Corneum Skin is composed of: Stratum corneum (the outer layer) Living epidermis Dermis: provide the skin barrier (blockade) layers to penetration by external agents Stratum corneum (keratinized tissue: major rate limiting barrier of TDDS) Behaves as a semipermeable artificial membrane drug molecules penetrate by passive diffusion
Physical Methods to Enhance TDDS Iontophoresis Delivery of charged chemical compounds across the skin membrane using an applied electrical field Drugs examined: lidocaine, dexamethasone, amino acids, peptides, insulin, verapamil, propanolol, Delivered by rapid injection because of rapid metabolism and poor absorption in oral delivery and from TDDS (large molecular size, ionic character) Enhance TDDS for peptide or protein administration
Drug Penetration in the Barrier Drug molecules through the stratum corneum: deeper epidermal tissues: dermis: vascularized dermal layer, Becomes available for absorption into the general circulation Good candidates for diffusion through the stratum corneum, epidermis, and dermis: aqueous and lipid soluble substances
Sonophoresis Studied as a means to enhance TDDS Influence integrity of stratum corneum and thus affect penetrability Agents examined: hydrocortisone, lidocaine, and salicylic acid in such formulations as gels, creams and lotions
Different Purposes for In-Vivo Skin Penetration Studies To verify and quantify: Cutaneous bioavailability of a topically applied drug Systemic bioavailability of a transdermal drug To establish bioequivalence of different topical formulations of the same drug substance To determine the incidence and degree of systemic toxicological risk following topical application of a specific drug or drug product To relate resultant blood levels of drug in human to systemic therapeutic effects
In-Vivo Skin Penetration Studies Most relevant studies performed in humans and animal models (predictors of human response)
Materials Used In-Vitro Skin Penetration Studies Skin penetration may be tested in vitro using: Various skin tissues (human or animal) in a diffusion cell Using human skin: limited because of difficulties of procurement, storage, expense, and variation in permeation Animal skin: shown to be effective like shed snakeskin (Elaphe obsolete, black rat snake) which is nonliving, pure stratum corneum, hairless and similar to human skin but slightly less permeable Living Skin Equivalent (LSE) Test Skin (Organogenesis Inc.) Product developed as an alternative for dermal absorption studies An organotypic culture of human dermal fibroblasts in a collagen-containing matrix and stratified epidermis composed of human epidermal keratinocytes
Controls the rate at which the drug is released for percutaneous absorption 2 types either with or without an excess of drug with regard to its equilibrium solubility and steady: state concentration gradient at the stratum corneum As the concentration of the drug in the device diminishes below the skins saturation limit Transport of drug from device to skin declines Most TDDs designed to contain an excess of drug Drug-releasing capacity beyond the time frame recommended for replacement Membrane-controlled transdermal system Designed to contain drug reservoir or pouch (in liquid or in gel form, a rate controlling membrane) Backing, adhesive, and protecting layers Examples of this technology: TransdermNitro (Novartis) and Transderm-Scop (Novartis) Advantage over monolithic systems: release rate of drug remains constant when the drug solution in the reservoir remains saturated Prepared by preconstruction of the delivery unit filling the drug reservoir: sealing or lamination Continuous process Serves as a rate-controlling mechanism or factor: Drug delivery device o If the drug is delivered to the stratum corneum at a rate less than the absorption capacity Skin o If the drug is delivered to the skin area to
The Transderm-Nitro System Comprises of Four Layers A tan-colored backing layer (aluminized plastic) that is impermeable to nitroglycerin A drug reservoir or matrix system containing nitroglycerin adsorbed on lactose, colloidal silicon dioxide, and silicon medical fluid An ethylene-vinyl acetate copolymer membrane that is permeable to nitroglycerin A layer of hypoallergenic silicon adhesive: a protective peel strip that is removed from the adhesive surface prior to use
Diffusion Systems and Principle Utilized Diffusion cell systems Employed in vitro to quantify the release rates of drugs from topical preparations Skin membranes or synthetic membranes employed as barriers to the flow of drug and vehicle to stimulate the biologic system
Different Layers of the Transdermal Drug Delivery System Occlusive or blockade backing membrane Protects the system from environmental entry and from loss of drug from the system or moisture from skin Drug reservoir or matrix system Stores and releases the drug at the skin site Release liner Removed before application and enables drug release
Two Categories of the TDDS Monolithic system Incorporate a drug matrix layer between backing and frontal layers Drug matrix layer Composed of polymeric material (drug is dispersed)
Adhesive layer Maintains contact application
with
the
skin
after Examples of Transdermal Drug Delivery Systems Transdermal Scopolamine (transderm scop system) Patch is worn (at least 4 hours before the antinausea effect is required) in a hairless area behind the ear Prevents motion sickness, nausea and vomiting resulting from the use of certain anesthetics and analgesics used in surgery Transdermal Nitroglycerin For prophylactic treatment of angina When taken sublingually: relatively low dose, short plasma half-life, high peak plasma levels, and inherent side effects Examples: Deponit (Schawarz), Minitram (3M Pharmaceuticals), Nitro-Dur (Key), and Transderm-Nitro (Novartis) Transdermal Clonidine (Catapres TTS) First trandermal system for hypertension Transdermal Nicotine (Nicotrol) As adjunct in smoking cessation programs Effective aid in quitting smoking Provides sustain blood levels of nicotine replacement therapy Transdermal Estradiol Treatment of moderate to severe vasomotor symptoms associated with menopause, female hypogonadism, female castration, primary ovarian failure, and atrophic conditions caused by deficient endogenous estrogen production (atrophic vaginitis and kraurosis vulvae) Examples: Vivelle (Novartis) Transdermal Testosterone For optimal absorption, applied to clean, dry scrotal skin that has been dry-shaved Placed on the scrotum (stretching the scrotal skin with one hand and pressing the adhesive side of the TDDS against the skin with the other hand, holding it in place for about 10 seconds) Androderm TDDS: applied nightly to a clean, dry unbraded area of the skin of the back, abdomen, upper arms, or thighs
Backing Layer Must be occlusive To retain the skin moisture and hydrate the site of application for increase drug penetration Used as backing liners Transparent or pigmented films of propylene, polyethylene, and polyofelin
Adhesive Layer Must be pressure sensitive Adheres to the skin with minimal pressure and remains in place for intended period of wear Should be non-irritating, permit unimpeded drug flux to the skin, compatible with all other systems, allow easy peel-off after use Commonly used as adhesive: polybutyl acrylate
Different Design Objectives of TDDS Deliver the drug to the skin for percutaneous absorption at therapeutic levels at an optimal rate Contain medicinal agents having necessary physiochemical characteristics to release from the system, and partition to the stratum corneum Occlude the skin to ensure one way flux of drug into the stratum corneum Have a therapeutic advantage over other dosage forms and drug delivery systems No irritation or sensitize the skin Adhere well to the patients skin and have size, appearance, and site placement that encourage acceptance
Advantages of TDDS Avoid: Gastrointestinal absorption difficulties First-pass effect Inconvenience of parenteral therapy Substitute for oral administration of medication Provide extended: Therapy with a single application Activity of drugs having a short half- life through the reservoir of drug in the therapeutic delivery system and its controlled release Drug therapy may be terminated rapidly by removal of the application from the surface of the skin Identified easily and rapidly in emergencies
Other Transdermal Therapeutic Systems Include: Diltiazem, isosorbide dinitrade, propranolol, nifedipine, mepindolol, and verapamil, cardiovascular agents Levonorgestrel with estradiol for hormonal contraception Physostigmine and xanomeline for Alzheimers disease therapy Naltrexone and methadone for substance addiction Buspirone for anxiety Bupropion for smoking cessation Papaverine for male impotence
Disadvantages of TDDS Only relatively potent drugs are suitable candidates for transdermal delivery Some patients develop contact dermatitis at the site of application
General Clinical Considerations in the Use of TDDSs Percutaneous absorption varies with the site of application Applied to clean, dry skin: relatively free of hair and not oily, irritated, inflamed, broken, or callused Use of skin lotion: avoided at the application site: affect skin hydration and can alter the partition coefficient between the drug and the skin Should not be physically altered by cutting since it destroys the integrity of the system Should be removed from its protective package or backing Placed at a site not subjected to being rubbed off by clothing or movement Worn for full period stated in the products instructions The patient or caregiver should clean the hands thoroughly before and after applying TDDS. In case of sensitivity or intolerance, the patient should seek revaluation TDDS should be folded in half: cannot be reused
Crystal Reservoir Technology Resulted in smaller patches with a more controlled and sustained drug release
Single Layer Drug-in-Adhesive Backing Drug-in-adhesive Liner
Multilayer Drug-in-Adhesive Backing Drug-in-adhesive Membrane Drug-in-adhesive Liner
Drug Reservoir-in-Adhesive Backing Drug Membrane Adhesive Liner
Drug Matrix-in-Adhesive Backing Adhesive Drug liner
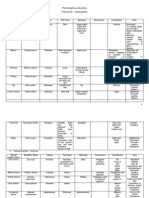
Therapeutic Agent Clonidine
TDDS Catapres-TTS (Boehringer Ingelheim)
Design and Content Four layer patch: (a) Backing of pigment polyester film (b) Reservoir of clonidine, mineral oil, polyisobutylene, colloidal silicone dioxide (c) Microporous polypropylene membrane controlling rate of delivery (d) Adhesive formulation of agents Four layer patch: (a) Transparent polyester film (b) Reservoir of estradiol, alcohol gelled with hydroxypropyl cellulose, (c) Ethylene vinyl acetate copolymer membrane (d) Adhesive formulation of light mineral oil, polyisobutylene Three-layer patch: (a) Translucent ethylene vinyl alcohol copolymer film (b) Estradiol in matrix of medical adhesive of poly isobutylene, ethylene vinyl acetate copolymer (c) Polyester release liner, removed prior to application Three-layer patch: (a) Translucent polyethylene film (b) Acrylate adhesive matrix containing estradiol (c) Protective liner of siliconized or fluoropolymer-coated polyester film, removed prior to use Four layer patch: (a) Backing layer of polyester film (b) Reservoir of fentanyl, alcohol gelled with hydroxyethyl cellulose (c) Rate controlling ethylene-vinyl acetate copolymer membrane (d) Fentanyl containing silicone adhesive Multilayer round patch: (a) Aluminized backing film (b) Pressure sensitive acrylate adhesive (c) Methacrylic acid copolymer solution of nicotine dispersed in pad of nonwoven viscose, cotton (d) Acrylate adhesive layer (e) Protective aluminized release liner that overlies adhesive layer, removed prior to use
Comments Transdermal therapeutic system to deliver therapeutic dose of antihypertensive drug at constant rate for 7 days. TDDS generally applied to hairless or shave are of upper arm or torso
Estradiol
Estraderm (Novartis)
Transdermal system to release 12b-estradiol continuously. Patch is generally applied to trunk, including abdomen and buttocks, alternating sites twice a weekly over 3-week cycle with dosage frequency adjusted as required
Vivelle (Novartis)
Use and application similar to Estraderm TDDS
Climara (Berlex )
Use and application similar to Estraderm TDDS and system may be applied weekly
Fentanyl
Duragesic (Janssen)
Transdermal therapeutic system providing continuous 72 hour systemic delivery of potent opioid analgesic and indicated in patients with chronic pain requiring opioid analgesia
Nicotine
Habitrol (Nivartis Consumer)
Transdermal therapeutic system providing continuous release systemic delivery of nicotine to aid smoking cessation. Patched somewhat vary in nicotine content and dosing schedules.
Nicoderm CQ (SmithKline Beecham Consumer)
Multilayer rectangular patch: (a) Occlusive backing of aluminum, polyester, ethylene-vinyl acetate copolymer (b) Reservoir of nicotine in ethylene-vinyl acetate copolymer matrix (c) Rate-controlling polyethylene membrane (d) Polyisobutylene liner, removed prior to application Multilayer rectangular patch:
Nicotrol
(McNeil Consumer)
(a) Outer backing of laminated polyester film (b) Rate-controlling adhesive nonwoven material, nicotine (c) Disposable liner, removed prior to use Multilayer round patch: (a) Beige foam tape acrylate adhesive (b) Backing foil gelatin low density polyethylene coating (c) Nicotine gel matrix (d) Protective foil with well (e) Release liner removed prior to use Three-layer system: (a) Covering foil (b) Nitroglycerin matrix with polyisobutylene adhesive, plasticizer, release membrane (c) Protective foil, removed prior to use Nitroglycerin in gel like matrix of glycerin water , lactose polyvinyl alcohol, povidone, sodium citrate sealed in polyester, foil, polyethylene laminate Four-layer patch: (a) Backing layer of aluminized plastic (b) Reservoir of nitroglycerin absorbed on lactose, colloidal silicone dioxide, ilicone medical fluid (c) Ethylene-vinyl acetate copolymer membrane (d) Silicone adhesive Four Layer patch: (a) Backing layer of aluminized polyester film (b) Reservoir of scopolamine, mineral oil, polyisobutylene (c) Microporous polypropylene membrane for rate delivery of scopolamine (d) Adhesive of polyisobutylene, mineral oil, scopolamine Three-layer patch: (a) Backing layer of polyethylene terephthalate (b) Matrix film layer of testosterone, ethylene-vinyl actetate copolymer (c) Adhesive strips of polyisobulylene, colloidal silicone dioxide Five-layer patch: (a) Backing film of ethylene-vinyl acetate copolymer, polyester laminate (b) Reservoir of testosterone, ,alcohol, glycerin, glyceryl monoleate, methyl laureate gelled with acrylic acid copolymer (c) Microporous polyethylene membrane (d) Acrylic adhesive (e) Adhesive polyester laminate
Prostep (Lederie)
Nitroglycerin
Deponit (Schwarz Pharma)
Nitroglycerin
Nitro- Dur (Key)
Nitroglycerin
TransdermNitro (Novartis)
Scopolamine
Transderm Scop (Novartis Consumer)
Testosterone
Testoderm (Alza)
Continuous release of drugs over 3 days to prevent nausea, vomiting of motion sickness. Patch is placed behind ear. For repeated administration, first patch is removed and second placed behind other ear. Also approved to prevent nausea of certain anesthetics and analgesics during surgery. Patch is placed on scrotum in treatment of testosterone deficiency
Adroderm (SmithKline Beecham)
Patch is placed on back, abdomen, upper arms, or thighs for treatment of testosterone deficiency
Potrebbero piacerti anche
- Carbohydrates InfoDocumento5 pagineCarbohydrates Infokaukau4everNessuna valutazione finora
- TANNINS CompleteDocumento61 pagineTANNINS Completekaukau4everNessuna valutazione finora
- Practical Exam PicsDocumento3 paginePractical Exam Picskaukau4everNessuna valutazione finora
- Glycosides For Practical PDFDocumento2 pagineGlycosides For Practical PDFkaukau4everNessuna valutazione finora
- Suha / Lukban: Citrus Grandis RutaceaeDocumento12 pagineSuha / Lukban: Citrus Grandis Rutaceaekaukau4everNessuna valutazione finora
- Volatile OilDocumento38 pagineVolatile Oilkaukau4everNessuna valutazione finora
- Tannins & LipidsDocumento46 pagineTannins & Lipidskaukau4ever100% (1)
- TanninsDocumento61 pagineTanninskaukau4everNessuna valutazione finora
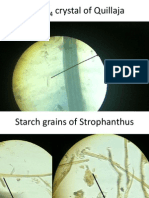
- Cac O Crystal of QuillajaDocumento22 pagineCac O Crystal of Quillajakaukau4everNessuna valutazione finora
- Resins (Practical Exam 8)Documento93 pagineResins (Practical Exam 8)kaukau4everNessuna valutazione finora
- Boards GlycosidesDocumento11 pagineBoards Glycosideskaukau4everNessuna valutazione finora
- Volatile OilDocumento38 pagineVolatile Oilkaukau4everNessuna valutazione finora
- Dosage Form Design Pharmaceutical and Formulation ConsiderationsDocumento103 pagineDosage Form Design Pharmaceutical and Formulation Considerationsprinceamit67% (3)
- AlkaloidsDocumento4 pagineAlkaloidskaukau4everNessuna valutazione finora
- Alkaloids SummaryDocumento1 paginaAlkaloids Summarykaukau4everNessuna valutazione finora
- Module 2 - Topic 1 - Protein Structure & Function Cont.Documento65 pagineModule 2 - Topic 1 - Protein Structure & Function Cont.kaukau4everNessuna valutazione finora
- Glycosides LecDocumento5 pagineGlycosides Leckaukau4everNessuna valutazione finora
- Module 1 - Topic 1 - The Chemistry of LifeDocumento142 pagineModule 1 - Topic 1 - The Chemistry of Lifekaukau4everNessuna valutazione finora
- Amino Acids TutorialDocumento9 pagineAmino Acids Tutorialkaukau4everNessuna valutazione finora
- AATableDocumento2 pagineAATablekaukau4everNessuna valutazione finora
- Amino AcidDocumento29 pagineAmino Acidmjzapant09Nessuna valutazione finora
- Dosage - Chapter 2 and Chapter 5Documento13 pagineDosage - Chapter 2 and Chapter 5Kim ManlangitNessuna valutazione finora
- Dosage - Chapter 13 (2d Half)Documento7 pagineDosage - Chapter 13 (2d Half)kaukau4everNessuna valutazione finora
- Dosage - Chapter 15Documento67 pagineDosage - Chapter 15Kim ManlangitNessuna valutazione finora
- Suppositories and InsertsDocumento5 pagineSuppositories and InsertsKim ManlangitNessuna valutazione finora
- Special Application SolutionsDocumento41 pagineSpecial Application SolutionsKim Manlangit100% (1)
- Dosage - Chapter 6Documento6 pagineDosage - Chapter 6kaukau4ever100% (3)
- Dosage - Chapter 14Documento57 pagineDosage - Chapter 14kaukau4ever100% (1)
- Dosage - Chapter 7Documento6 pagineDosage - Chapter 7kaukau4everNessuna valutazione finora
- Dosage - Chapter 9Documento5 pagineDosage - Chapter 9kaukau4everNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Quiz #1 Questions A&P 1Documento14 pagineQuiz #1 Questions A&P 1trick49Nessuna valutazione finora
- 2007, Vol.25, Issues 4, Cutaneous Receptors - Clinical Implications and Therapeutic RelevanceDocumento202 pagine2007, Vol.25, Issues 4, Cutaneous Receptors - Clinical Implications and Therapeutic RelevanceRizweta DestinNessuna valutazione finora
- Burn Case StudyDocumento76 pagineBurn Case StudyJoshua Agawin100% (1)
- Dermatology Revision E6.5 'Documento35 pagineDermatology Revision E6.5 'Riya SharmaNessuna valutazione finora
- Vdoc - Pub Clear Skin CookbookDocumento166 pagineVdoc - Pub Clear Skin CookbookAnca OanaNessuna valutazione finora
- 176 Anatomy Integumentary SystemDocumento29 pagine176 Anatomy Integumentary SystemJoana Mae PortezaNessuna valutazione finora
- The Integumentary System: Powerpoint Lecture Slides Prepared by Meg Flemming Austin Community CollegeDocumento62 pagineThe Integumentary System: Powerpoint Lecture Slides Prepared by Meg Flemming Austin Community CollegetanarNessuna valutazione finora
- Dermatopathology Diagnosis by First Impression 3rd Edition Ebook PDFDocumento57 pagineDermatopathology Diagnosis by First Impression 3rd Edition Ebook PDFmario.becker252100% (37)
- Campus Collusio N: Review Questions For Test PreparationDocumento3 pagineCampus Collusio N: Review Questions For Test PreparationGenna LedesmaNessuna valutazione finora
- His To Logical Changes in Radial Forearm Skin Flaps in The Oral Cavity - DR Darwish Badran - Medics Index MemberDocumento6 pagineHis To Logical Changes in Radial Forearm Skin Flaps in The Oral Cavity - DR Darwish Badran - Medics Index MemberMedicsindex Telepin Slidecase100% (1)
- Well Differentiated Squamous Cell Carcinoma, Keratoacanthoma Type. Three Cases. DR Sarma's DermpathDocumento17 pagineWell Differentiated Squamous Cell Carcinoma, Keratoacanthoma Type. Three Cases. DR Sarma's DermpathDeba P SarmaNessuna valutazione finora
- ANAPHY 1st ExamDocumento12 pagineANAPHY 1st ExamVine OrtegaNessuna valutazione finora
- Clinical, Dermoscopic and Histhopatological Findings in Diagnosis of Nevus SpilusDocumento7 pagineClinical, Dermoscopic and Histhopatological Findings in Diagnosis of Nevus SpilusYeni PuspitasariNessuna valutazione finora
- Diabetic Foot Ulcer Case StudyDocumento38 pagineDiabetic Foot Ulcer Case StudySanti Moore100% (1)
- Science6 q2 Mod1 Lesson1-2 Human Body System v1Documento32 pagineScience6 q2 Mod1 Lesson1-2 Human Body System v1HONEYLENE ORNOSNessuna valutazione finora
- Dermatologic Disorders PDFDocumento48 pagineDermatologic Disorders PDFWilda Hanim100% (1)
- Randyr Integumentary System WorksheetDocumento9 pagineRandyr Integumentary System WorksheetRandy ReynosoNessuna valutazione finora
- Geriatric DermatologyDocumento30 pagineGeriatric DermatologyMudsa Iing IletoNessuna valutazione finora
- Case Study Scarlet Fever Repaired)Documento34 pagineCase Study Scarlet Fever Repaired)Reimark RabanalNessuna valutazione finora
- SkinDocumento38 pagineSkinrodelagapito100% (1)
- eng - план разработка 7 2021Documento11 pagineeng - план разработка 7 2021НургулNessuna valutazione finora
- Microbiome and Skin Biology: ReviewDocumento6 pagineMicrobiome and Skin Biology: ReviewLinhNguyeNessuna valutazione finora
- The Integumentary System: Structure and FunctionsDocumento9 pagineThe Integumentary System: Structure and FunctionsJohn Paul ArcillaNessuna valutazione finora
- Unit VI Lecture NotesDocumento5 pagineUnit VI Lecture NotesSteve Sullivan100% (1)
- DR SARMA'S DERMPATH: Acantholytic Seborrheic Keratosis. The Internet Journal of Dermatology 2008: Volume 6 Number 2Documento4 pagineDR SARMA'S DERMPATH: Acantholytic Seborrheic Keratosis. The Internet Journal of Dermatology 2008: Volume 6 Number 2Deba P SarmaNessuna valutazione finora
- Caps HTMLDocumento152 pagineCaps HTMLUchy Luph'milimiLy0% (1)
- The Integumentary System: Skin, Hair, and NailsDocumento55 pagineThe Integumentary System: Skin, Hair, and NailsSandy CaliguiaNessuna valutazione finora
- RenovHyal Anti-Ageing Ingredient Reinforces Skin BarrierDocumento8 pagineRenovHyal Anti-Ageing Ingredient Reinforces Skin BarrierMaritaNetoNessuna valutazione finora
- Who Guidelines Hand Hygiene PDFDocumento170 pagineWho Guidelines Hand Hygiene PDFKomite PpiNessuna valutazione finora
- Activity 2B Integumentary System LOPEZ 1.0Documento3 pagineActivity 2B Integumentary System LOPEZ 1.0Ma. Joanna Catherine LopezNessuna valutazione finora