Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Change in Flatfoot of Preschool-Aged Children - A 1-Year Follow-Up Study
Caricato da
mdwilliamsDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Change in Flatfoot of Preschool-Aged Children - A 1-Year Follow-Up Study
Caricato da
mdwilliamsCopyright:
Formati disponibili
Eur J Pediatr DOI 10.
1007/s00431-012-1884-4
ORIGINAL ARTICLE
Change in flatfoot of preschool-aged children: a 1-year follow-up study
Kun-Chung Chen & Li-Chen Tung & Chih-Jung Yeh & Jeng-Feng Yang & Jing-Fu Kuo & Chun-Hou Wang
Received: 26 August 2012 / Accepted: 23 October 2012 # Springer-Verlag Berlin Heidelberg 2012
Abstract The main purpose of this study is to investigate the changes in the signs of flatfoot of preschool-aged children in a 1-year follow-up study. This study performed follow-up on a total of 580 preschool-aged children (boys, 297 children; girls, 283 children) with a median age of 54 (range 3671 months), and the average follow-up period was 11.8 months. This study used the ChippauxSmirak index (CSI) of footprint as the assessment tool, and CSI>62.70 % was used as the standard for determining whether preschool-aged children suffered from flatfoot. The results showed that the signs of flatfoot of
K.-C. Chen : J.-F. Kuo : C.-H. Wang Physical Therapy Room, Chung Shan Medical University Hospital, No.110, Sec. 1, Jianguo N. Rd., Taichung City 402, Taiwan K.-C. Chen : C.-H. Wang (*) School of Physical Therapy, College of Medical Technology, Chung Shan Medical University, No.110, Sec. 1, Jianguo N. Rd., Taichung City 402, Taiwan e-mail: chwang@csmu.edu.tw L.-C. Tung Department of Physical Medicine and Rehabilitation, Chi Mei Medical Center, Liou Ying Campus, No.201, Taikang Village, Liou Ying Township, Tainan 736, Taiwan C.-J. Yeh School of Public Health, Chung Shan Medical University, No.110, Sec. 1, Jianguo N. Rd., Taichung City 402, Taiwan J.-F. Yang Department of Physical Therapy, Medical College, National Cheng Kung University, No.1, Ta-Hsueh Road, Tainan 701, Taiwan
preschool-aged children improved with increasing age. At the 1-year follow-up, the average CSI was 5.1 % lower, and the proportion of children with flatfoot was 14 % lower. The follow-up on the change in the signs of flatfoot showed that 37.6 % of the children originally with flatfoot had improved to normal, verifying that flatfoot indeed improves with increasing age. However, the results also showed that 9.9 % of the children who originally had normal feet had developed flatfoot with increasing age, which deserves subsequent investigation. The results of the follow-up also showed that children who were relatively younger, male, obese, and experiencing excessive joint laxity were more likely to experience the signs of flatfoot. Conclusion: The 1-year follow-up found that some preschool-aged children with flatfoot may develop normal feet, while children with normal feet may begin to experience the signs. Relevant factors affecting flatfoot in preschool-aged children continue to require further clarification. Keywords Cohort study . Flatfoot . Footprint . Preschool-aged children
Introduction Flatfoot, one of the most common foot problems experienced by preschool-aged children, refers to the phenomenon of the collapse or disappearance of the medial longitudinal arch [22]. The feet of infants are usually flat when they are born, and the arch will gradually develop as the child grows. The preschool stage is the main period in which the medial longitudinal arch develops [11, 24]. Flatfoot in children may easily lead to poor gait patterns at adulthood [1, 7]. One study indicated that the early treatment of flatfoot could prevent future prominent navicular or bunion development symptoms [13]. Therefore, it is necessary to understand the changes in the signs of flatfoot in children.
Eur J Pediatr
Of the few studies that have been conducted on flatfoot in preschool-aged children, some have indicated that the symptoms of flatfoot in preschool-aged children may be associated with various factors, such as age, gender, weight, and joint laxity [5, 8, 14, 16, 18, 23]. A study by Pfeiffer et al. [18] on 853 preschool-aged children indicated that the prevalence of flatfoot in preschool-aged children was approximately 44 %, and that this percentage decreased with increasing age. While many other studies obtained similar results [4, 14, 22]; they were cross-sectional studies, and there remains a lack of direct evidence from long-term clinical follow-ups for verification. The high reliability of the clinical use of footprints for measuring and determining flatfoot has been verified [6, 11, 12, 22]. Previous studies also verified that footprints are applicable to the screening of flatfoot in preschool-aged children, and it has been pointed out that the ChippauxSmirak index (CSI) is the most applicable measurement for the assessment of the medial longitudinal arch in preschool-aged children [4, 17]. One study found that the accuracy of the CSI for determining flatfoot in preschool-aged children was as high as 90 % [4]. Therefore, this index can be used for screening flatfoot [4]. The main purpose of this study was to use follow-up examinations to investigate the changes of flatfoot in preschool-aged children. A second purpose was to determine the factors affecting flatfoot in preschool-aged children in order to provide direct evidence as a reference for clinical workers.
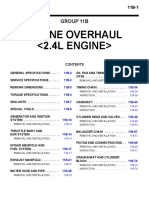
Measures Basic information, including age, height (in centimeters), and weight (to the nearest 0.1 kg), was collected. The body mass index (BMI) was calculated for every child by dividing the weight (in kilograms) by the square of the height (in square meters). The BMI of the children was used to classify them into four weight levelsunderweight, normal, overweight, and obeseaccording to the definitions of obesity for children and adolescents provided by the Food and Drug Administration, Department of Health, and the Executive Yuan of Taiwan [2, 5]. Generalized joint laxity was measured by Beighton score [20]; a Beighton score greater than 4 is indicative of generalized joint laxity [20]. The footprints of subjects were collected by a physical therapist. Subjects were requested to stand on the Harrisbath mat [19] on each foot in a 100 % weight-bearing position. Assessments were conducted using digital images, and the parameters of the footprints were measured and calculated using computer software. This study used the CSI to determine whether children exhibited the signs of flatfoot. The CSI is defined as the ratio of the minimum width of the midfoot arch region (B) to the maximum width of the metatarsus region (A) of the footprint (Fig. 1). Previous studies suggested that the appropriate criteria for determining flatfoot in preschool-aged children were CSI>62.70 % for flatfoot (positive) and CSI62.70 % for normal [4]. Because the objectives of this study were to investigate the changes in footprints in preschool-aged children, the right and left feet of the subjects were regarded as independent data for processing. A total of 1,160 footprints were collected for analysis. Statistical analysis The basic information of subjects was presented by median and range (minimummaximum), and paired-samples t test was used to examine the difference before and after the 1year follow-up. The independent t test and chi-square test were used to examine the differences between incomplete and complete follow-up groups. The results of flatfoot as determined by CSI were converted to percentages in order to illustrate the changes of flatfoot in children at different ages at 1-year followup. The subjects were divided into four groups according to the changes at the follow-up for investigation. Group A consisted of those whose footprints were originally determined as normal and remained normal at the 1year follow-up; group B was those whose footprints were originally determined as normal and had developed flatfoot by the 1-year follow-up; in group C were those whose footprints were originally determined as flatfoot and had become normal by the 1-year follow-up; and in
Methods Participants This cohort study collected the footprints of preschool-aged children from ages 3 to 5 years at kindergartens in central Taiwan and performed a follow-up check 1 year later. Details of the study procedure were presented, and informed consent was obtained from the parents or legal guardians before children were enrolled in the study. Exclusion criteria were (1) a history of musculoskeletal or neurological impairment which affected lower limb structure and movement and (2) inability to follow orders for measurement. Initially, the footprint data of 859 preschool-aged children were included in the study. At the 1-year follow-up, the data of 249 children could not be collected, as they had transferred to other schools or been admitted to elementary school early. Another 30 children who were undergoing corrective treatment including use of insoles and shoes for correction or received physical therapy were excluded from this study, leaving a total of 580 preschool-aged children for analysis. The overall follow-up completion rate was 67.5 %.
Eur J Pediatr
Moreover, one-way analysis of variance was used to test the changes in the CSI value of subjects at different ages and to compare the differences between group A and group D at the 1-year follow-up. A level of p<0.05 was used to determine the statistical significance in this study, and calculations were performed with the statistical software SPSS 14.0 (SPSS Inc., Chicago, IL, USA).
Results A total of 859 preschool-aged children (449 boys and 410 girls) were included in this study. The average follow-up period was 11.8 months. A total of 279 children (152 boys and 127 girls) who were initially enrolled but failed to complete the follow-up was excluded, leaving a total of 580 children (297 boys and 283 girls) for analysis. The children who did not complete the followup did not differ significantly from the children who did (Table 1). According to Table 2, the CSI values of children at various ages at 1-year follow-up differed significantly (p<0.001). The CSI values fell by approximately 5.1 % after 1-year follow-up, and the prevalence of flatfoot fell by approximately 14 % in this study. We also found that the amount of change in CSI value was reduced with increasing age at the 1-year follow-up. The CSI value of 3-year-old children decreased by 22.9 % (from 68.2 to 45.3 %), while that of that 5-year-old children decreased by 5.0 % (from 37.8 % to 32.8 %) at 1-year follow-up. This study divided preschool-aged children into groups A, B, C, and D according to the type of change at follow-up in order to analyze and compare the results of each group. The results showed that 90.1 % (521/578) of the children who were initially determined as having normal feet remained normal after the 1-year follow-up. However,
Fig. 1 ChippauxSmirak index (CSI)0B / A100 %
group D were those whose footprints were originally determined as flatfoot which remained at 1-year follow-up.
Table 1 Characteristics of participants Incomplete (n0279) p Valuea
Complete follow-up (n0580) Initial Follow-up 297/283 66 (4682) 112.0 (93.0139.5) 20.0 (12.045.0) 15.8 (10.928.8) 2 (08) 57.6 (16.188.4)
p Valueb
Gender (boy/girl) Age (months) Body height (cm) Body weight (kg) Body mass index (kg/cm2) Beighton score ChippauxSmirak index (%)
152/127 54 (3769) 105.0 (89.0125.0) 17.4 (12.028.5) 15.9 (10.625.0) 2 (09) 62.0 (6.587.5)
0.369 0.765 0.518 0.418 0.577 0.078 0.114
297/283 54 (3671) 105.0 (88.0127.5) 18.0 (11.037.0) 16.0 (9.926.6) 2 (08) 62.8 (20.1117.7)
NA <0.001 <0.001 <0.001 0.748 <0.001 <0.001
Values in italics are given as median (range, minimummaximum) NA not available
a b
Incomplete versus complete follow-up initial Initial versus follow-up
Eur J Pediatr Table 2 Changes of Chippaux Smirak index (CSI) between different ages
Age of initial assessment 3 years (n0274) Initial CSI (%) Flatfoot (n (%)) Follow-up CSI (%) Flatfoot (n (%)) 4 years (n0624) 5 years (n0262)
Total (n01,160)
68.2 (28.5117.7) 187 (68.2) 61.3 (16.188.2) 124 (45.3)
62.2 (20.593.6) 296 (47.4) 56.7 (18.988.4) 210 (33.7)
59.7 (28.482.7) 99 (37.8) 55.3 (25.979.9) 86 (32.8)
62.8 (20.5117.7) 582 (50.2) 57.6 (16.188.4) 420 (36.2)
The values of CSI (in italics) are given as median (range, minimummaximum)
9.9 % (57/578) of the children who were initially determined as having normal feet were determined to have flatfoot at the 1-year follow-up; 37.6 % (219/582) of the children who were initially determined to have flatfoot were determined to have normal feet at the 1-year follow-up, and 62.4 % (363/582) of the children initially determined to have flatfoot still had flatfoot at the 1-year follow-up, as shown in Table 3. We further compared the differences between group A and group D. We found significant statistical differences (p<0.05) in age, gender, height, BMI, and Beighton score between the two groups. In group D, the average age was younger, the proportion of boys was higher (200/363, 55.1 %), the proportions of overweight and obese children were higher (28.9 %, 105/363), and the proportion of those experiencing excessive joint laxity children was higher (34.2 %), as shown in Table 4.
Discussion To the best of our knowledge, this is the first cohort study to follow up on changes of flatfoot in preschool-aged children. Few studies have focused on the prevalence of flatfoot in preschool-aged children. Staheli et al. [22] compared footprints by age and found a higher prevalence of flatfoot in preschool-aged children. Pfeiffer et al. [18] found that the prevalence of flatfoot was about 43.7 % in preschool-aged children, and that the proportion of flatfoot fell with increasing age. Other previous research also reported similar results [24, 9, 15], but all of those studies were cross-sectional. Our data showed that the prevalence of children with flatfoot decreased from 68.2 % in 3-year-old children to 37.8 % in 5-year-old children and that the CSI value decreased with increasing age, from 66.3 % in 3-year-old children to 58.7 %
Table 4 Comparison of group A with group D including relevant factors influencing flatfoot Table 3 Results of follow-up between different ages with footprint analysis Age of initial 3 years (n0274) Initial, normal Follow-up, normala (n (%)) Follow-up, flatfootb (n (%)) Initial, flatfoot Follow-up, normalc (n (%)) Follow-up, flatfootd (n (%))
a b c d
Group A (n0521)a Gender (boy/girl) Age of initial (months) Body height (cm) Body weight (kg) Body mass index Obesity status (underweight/ normal/ overweight/ obese) Joint laxityc (%) ChippauxSmirak index (%) 245/276 56 (3671) 106.0 (88.0127.5) 18.0 (11.232.0) 15.7 (9.921.6) 85/347/60/29
Group D (n0363)b 200/163 53 (3669)
p Value
Total (n01,160) 5 years (n0262) 163 147 (90.2) 16 (9.8) 99 29 (29.3) 70 (70.7) 578 521 (90.1) 57 (9.9) 582 219 (37.6) 363 (62.4)
4 years (n0624) 328 297 (90.5) 31 (9.5) 296 117 (39.5) 179 (60.5)
0.018 <0.001
87 77 (88.5) 10 (11.5) 187 73 (39.0) 114 (61.0)
104.3 (89.0122.0) <0.001 17.7 (11.037.0) 0.529 16.3 (10.026.6) <0.001 32/226/65/40 <0.001
22.8 52.5 (22.062.7)
34.2 73.0 (62.793.6)
<0.001 <0.001
Group A: initial as normal and follow-up as normal Group B: initial as normal and follow-up as flatfoot Group C: initial as flatfoot and follow-up as normal Group D: initial as flatfoot and follow-up as flatfoot
Values in italics are given as median (range: minimummaximum)
a b c
Group A: initial as normal and follow-up as normal Group D: initial as flatfoot and follow-up as flatfoot Beighton score of 4 is considered indicative of generalized joint laxity
Eur J Pediatr
in 5-year-old children. This result is consistent with that of a previous cross-sectional study [4]. The results further demonstrated that as the preschool-aged children grew 1 year older, the prevalence of flatfoot decreased by 14 %, and that at 1-year follow-up, the CSI value of 3-year-old children decreased by 7 %, while that of 5-year-old children decreased by 3.4 %. This finding verified that the prevalence of children with flatfoot is indeed reduced with increasing age and that the development of the arch is faster in younger children. The change in 3-year-old children was the most significant. Some scholars have suggested that it is common for preschool-aged children to experience the signs of flatfoot and that their feet will gradually become normal with increasing age [21, 25]. This study divided the subjects into four groups, A, B, C, and D, according to the changes at 1year follow-up in order to investigate the changes. The results showed that 37.6 % of the children who initially had flatfoot had developed normal feet after 1 year (group C), verifying that the signs of flatfoot in preschool-aged children may indeed disappear with increasing age. The research results also showed that 9.9 % of the children who were initially determined to have normal feet had developed flatfoot after 1 year (group B), indicating that some preschool-aged children may gradually develop flatfoot with increasing age. This phenomenon has never been reported by previous studies and is worthy of further investigation in the future. Previous studies have indicated that the symptoms of flatfoot of preschool-aged children may be associated with various factors, such as age, gender, weight, and joint laxity [5, 8, 14, 16, 18, 23]. This study further analyzed and compared group A with group D and found that in group D, the average age was younger, the proportion of boys was higher (200/363, 55.1 %), the proportions of obesity levels of overweight and obese were higher (65/363, 17.9 %; 40/ 363, 11.0 %), and the proportion of excessive joint laxity was higher (124/239, 34.2 %). This result is consistent with those of previous studies [5, 8, 14, 16, 18, 23]; however, those studies were cross-sectional studies. This study used the cohort follow-up approach to verify that preschool-aged children who are younger, male, obese, and experiencing excessive joint laxity are more likely to experience the signs of flatfoot. To our knowledge, the effects of treatments for flatfoot remain controversial. Footwear, stretching exercises, or orthoses were usually used for treating flatfoot, but studies have failed to prove their effectiveness [21, 25]. Our data showed that the sign of flatfoot in preschool-aged children improves with age, but still some may develop flatfoot with increasing age. Flatfoot should be assessed on the basis of symptoms and morphologic development. Our study did not state the symptoms of these children, but we agreed with
Evans [10] and recommend that the symptomatic flatfoot of preschool-aged children should be treated and asymptomatic flatfoot just needs to be monitored for development. This study used 1-year follow-up to investigate changes in the signs of flatfoot of preschool-aged children with increasing age. However, owing to restrictions of labor and funding, the follow-up was only 1-year period and performed on children aged 3 to 5 years and restricted geographically. In the future, more long-term follow-up studies until growth arrest may be conducted on the changes in signs of children with flatfoot, and different factors will be taken into account in order to investigate their effects on the signs of flatfoot.
Acknowledgments The authors thank all participants in this study and the physical therapists, Pei-Shan Tsai and Yi-Ying Tsai, who kindly provided assistance with data collection. This study was supported by research grants from the National Science Council, Taiwan (NSC99-2314-B-040-004-MY3). Conflict of interest No party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated. All authors state that they do not keep any commercial, financial, or personal relationships that may lead to a conflict of interest that could inappropriately influence (bias) their work.
Ethical Board Review statement Each author certifies that his institution approved the human protocol for this investigation that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained (CSMUH No.: CS09114).
References
1. Cappello T, Song KM (1998) Determining treatment of flatfeet in children. Curr Opin Pediatr 10:7781 2. Chang JH, Wang SH, Kuo CL, Shen HC, Hong YW, Lin LC (2010) Prevalence of flexible flatfoot in Taiwanese school-aged children in relation to obesity, gender, and age. Eur J Pediatr 169:447452 3. Chen JP, Chung MJ, Wang MJ (2009) Flatfoot prevalence and foot dimensions of 5- to 13-year-old children in Taiwan. Foot Ankle Int 30:326332 4. Chen KC, Yeh CJ, Kuo JF, Hsieh CL, Yang SF, Wang CH (2011) Footprint analysis of flatfoot in preschool-aged children. Eur J Pediatr 170:611617 5. Chen KC, Yeh CJ, Tung LC, Yang JF, Yang SF, Wang CH (2011) Relevant factors influencing flatfoot in preschool-aged children. Eur J Pediatr 170:931936 6. Clarke HH (1933) An objective method of measuring the height of the longitudinal arch in foot examinations. Res Q 4:99107 7. Cohen-Sobel E, Giorgini R, Velez Z (1995) Combined technique for surgical correction of pediatric severe flexible flatfoot. J Foot Ankle Surg 34:183194 8. Dowling AM, Steele JR, Baur LA (2001) Does obesity influence foot structure and plantar pressure patterns in prepubescent children? Int J Obes Relat Metab Disord 25:845852
Eur J Pediatr 9. Echarri JJ, Forriol F (2003) The development in footprint morphology in 1851 Congolese children from urban and rural areas, and the relationship between this and wearing shoes. J Pediatr Orthop B 12:141146 10. Evans AM (2008) The flat-footed childto treat or not to treat: what is the clinician to do? J Am Podiatr Med Assoc 98:386393 11. Forriol F, Pascual J (1990) Footprint analysis between three and seventeen years of age. Foot Ankle 11:101104 12. Irwin LW (1937) A study of the tendency of school children to develop flat-footedness. Res Q 8:4653 13. King DM, Toolan BC (2004) Associated deformities and hypermobility in hallux valgus: an investigation with weightbearing radiographs. Foot Ankle Int 25:251255 14. Lin CJ, Lai KA, Kuan TS, Chou YL (2001) Correlating factors and clinical significance of flexible flatfoot in preschool children. J Pediatr Orthop 21:378382 15. Mickle KJ, Steele JR, Munro BJ (2006) The feet of overweight and obese young children: are they flat or fat? Obesity (Silver Spring) 14:19491953 16. Mickle KJ, Steele JR, Munro BJ (2008) Is the foot structure of preschool children moderated by gender? J Pediatr Orthop 28:593596 17. Onodera AN, Sacco IC, Morioka EH, Souza PS, de Sa MR, Amadio AC (2008) What is the best method for child longitudinal plantar arch assessment and when does arch maturation occur? Foot (Edinb) 18:142149 Pfeiffer M, Kotz R, Ledl T, Hauser G, Sluga M (2006) Prevalence of flat foot in preschool-aged children. Pediatrics 118:634639 Shores M (1980) Footprint analysis in gait documentation. An instructional sheet format. Phys Ther 60:11631167 Simpson MR (2006) Benign joint hypermobility syndrome: evaluation, diagnosis, and management. J Am Osteopath Assoc 106:531536 Staheli LT (1999) Planovalgus foot deformity. Current status. J Am Podiatr Med Assoc 89:9499 Staheli LT, Chew DE, Corbett M (1987) The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am 69:426428 Villarroya MA, Esquivel JM, Tomas C, Moreno LA, Buenafe A, Bueno G (2009) Assessment of the medial longitudinal arch in children and adolescents with obesity: footprints and radiographic study. Eur J Pediatr 168:559567 Volpon JB (1994) Footprint analysis during the growth period. J Pediatr Orthop 14:8385 Wenger DR, Mauldin D, Speck G, Morgan D, Lieber RL (1989) Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. J Bone Joint Surg Am 71:800810
18. 19. 20.
21. 22.
23.
24. 25.
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Engine Overhaul : Group 11BDocumento80 pagineEngine Overhaul : Group 11BДмитрий100% (1)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Advanced MultisimDocumento146 pagineAdvanced MultisimHec Itou75% (4)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- PL-SQL FunctionsDocumento130 paginePL-SQL Functionswasim ahmed100% (1)
- Pre Stressed Concrete Solved ProblemsDocumento17 paginePre Stressed Concrete Solved ProblemsJefferson T. Ignacio75% (28)
- The Role of Cutoffs in Integrated Reservoir StudiesDocumento15 pagineThe Role of Cutoffs in Integrated Reservoir StudiesAhmed M. Saad100% (1)
- Steel and Timber Structures Part Two:: Design of Structural Steel MembersDocumento28 pagineSteel and Timber Structures Part Two:: Design of Structural Steel MembersDhinesh KalaimaranNessuna valutazione finora
- Quiz Questions TD 1Documento6 pagineQuiz Questions TD 1Susmita PandaNessuna valutazione finora
- Pulse Oximetry ReviewDocumento26 paginePulse Oximetry ReviewmdwilliamsNessuna valutazione finora
- Has The Hospital Become The Place Not To Be For Infants With BronchiolitisDocumento2 pagineHas The Hospital Become The Place Not To Be For Infants With BronchiolitismdwilliamsNessuna valutazione finora
- Hair Tourniquet SyndromeDocumento1 paginaHair Tourniquet SyndromemdwilliamsNessuna valutazione finora
- Therapy in Pediatric StrokeDocumento9 pagineTherapy in Pediatric StrokemdwilliamsNessuna valutazione finora
- Process Control Plan Excel TemplateDocumento13 pagineProcess Control Plan Excel TemplateTalal NajeebNessuna valutazione finora
- When Bad Things Happen To Good MissilesDocumento9 pagineWhen Bad Things Happen To Good Missilesmykingboody2156Nessuna valutazione finora
- Excel VBA To Interact With Other ApplicationsDocumento7 pagineExcel VBA To Interact With Other ApplicationsgirirajNessuna valutazione finora
- Sag 38 2 12 0709 2Documento7 pagineSag 38 2 12 0709 2Yoselin GomezNessuna valutazione finora
- WPH04 01 Que 20160118Documento28 pagineWPH04 01 Que 20160118josekadaNessuna valutazione finora
- Design, Development, Fabrication and Testing of Small Vertical Axis Wind TurbinevDocumento4 pagineDesign, Development, Fabrication and Testing of Small Vertical Axis Wind TurbinevEditor IJTSRDNessuna valutazione finora
- EO Gaddis Java Chapter 06 6e-ClassesObjectsPart2Documento48 pagineEO Gaddis Java Chapter 06 6e-ClassesObjectsPart2nyle90009Nessuna valutazione finora
- Ak98 Preset ListDocumento21 pagineAk98 Preset ListHichem NaghmouchiNessuna valutazione finora
- Application SMS MD720-3 DOKU V2 1 enDocumento52 pagineApplication SMS MD720-3 DOKU V2 1 enerendira77Nessuna valutazione finora
- Exemplar Gr1 Maths Diagnostic Assessment - Term 2 - 2021Documento4 pagineExemplar Gr1 Maths Diagnostic Assessment - Term 2 - 2021Liandra'Lulu'VdMerweNessuna valutazione finora
- Homework # 4:: Hazard Analysis, Groundmotion, Response Spectrum and Nonlinear ResponseDocumento2 pagineHomework # 4:: Hazard Analysis, Groundmotion, Response Spectrum and Nonlinear ResponseAbhinavNessuna valutazione finora
- Switchgear and Protection May 2022Documento1 paginaSwitchgear and Protection May 2022Sanapala RAJENDRA PRASADNessuna valutazione finora
- Dosing Technology: eco-CONTROL EC200-KDocumento2 pagineDosing Technology: eco-CONTROL EC200-KMario Vargas VegaNessuna valutazione finora
- 10 Detection of Signals in NoiseDocumento20 pagine10 Detection of Signals in NoisekirankumarrathNessuna valutazione finora
- Tesis de Pared de BloquesDocumento230 pagineTesis de Pared de BloquesRobert FinqNessuna valutazione finora
- Working With Files and Directories: Chapter 11Documento62 pagineWorking With Files and Directories: Chapter 11Abdelahad SatourNessuna valutazione finora
- B.pharmacy Project SD of GlimepirideDocumento12 pagineB.pharmacy Project SD of Glimepiridemanvitha varmaNessuna valutazione finora
- Cad and Dog 2Documento5 pagineCad and Dog 2Muhammad RifaiNessuna valutazione finora
- Experiment 6Documento11 pagineExperiment 6CarlosLorenzoSaninNessuna valutazione finora
- 2003 831 01 - Fiber Optic AttenuatorDocumento51 pagine2003 831 01 - Fiber Optic AttenuatorchopanalvarezNessuna valutazione finora
- Fork LiftDocumento4 pagineFork Lifttamer goudaNessuna valutazione finora
- 4-DatAdvantage Advanced Installation For Microsoft Platforms 8.6 - M365 PatchDocumento158 pagine4-DatAdvantage Advanced Installation For Microsoft Platforms 8.6 - M365 PatchyaritzaNessuna valutazione finora
- Appendix 59.docx Inventory Custodian SlipDocumento2 pagineAppendix 59.docx Inventory Custodian SlipJimmy CootNessuna valutazione finora