Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
GI Study Guide
Caricato da
NursingSchoolNotesDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
GI Study Guide
Caricato da
NursingSchoolNotesCopyright:
Formati disponibili
GI study guide.
Anatomy and physiology, Enzymes
1. Mouth: Buccal mucosa, Lips, hard Palate, Soft palate, teeth a. Salivary glands: secret amylase to breakdown carbohydrates 2. Esophagus: a. upper esophageal sphincter: at rest close to prevent air into esophagus b. Lower esophageal sphincter: at rest normally closed to prevent reflux 3. Stomach: a. parietal cells: hydrochloric acid, intrinsic factor b. chief cells: pepsinogen c. secretin: inhibits acid production 4. Pancreas: a. exocrine function: digestive enzymes such as Ductal cells and Acinar cells b. endocrine function: producing hormones such as insulin, glucagon, somatostatin 5. Liver a. storage of vitamins, minerals, iron magnesium, fat soluble vitamins A, D, E, K. b. Protective: Kupffer cells, engulfs harmful bacteria and anemic red cells, detoxifies blood c. metabolism: breakdown proteins removes ammonia (converts to urea) synthesis of plasma proteins: albulmin, prothrombin, and fibrinogen stores glycogen synthesizes, breaksdown, and stores fatty acids, triglycerides forms and secretes bile in response to gastrin, secretin, cholescystokinin 6. Gallbladder: Collects, concentrates, and stores bile. Is released when fat is present in duodenum 7. Small Intestines: movement, digestion, and absorption 8. Large Intestines: ascending, transverse, descending, sigmoid, rectum, anus a. blood supply: 20% total cardiac output Misc GI Diagnostics: 1. Prothrombin time: severe or acute liver disease leads to elevated prothrombin time 2. CBC: GI bleed is most common cause of anemia in adults 3. Calcium: is absorbed in GI tract, may detect malabsorption 4. Sodium, Potassium; absorbed in GI tract: vomiting and diarrhea may cause depletion 5. AST/ALT: enzymes found in liver. 6. Amylase, Lipase: elevations indicate pancreatitis 7. Ammonia: high levels indicate liver dysfunction 8. Bilirubin: pigment in bile. Elevations show impaired secretion from liver and bilary system 9. CA 19-9: diagnose GI cancer 10: Urine test: amylase, urobilinogen 11. Stool test:
a. fecal fat/steatorrhea: indicates malabsorption in small intestines b. clostridium difficile: toxin from bacteria causes severe diarrhea
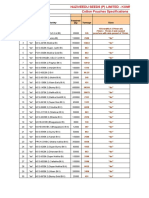
Some of the major enzymes to know, please note these are not all of them, only the ones mentioned on the power points. Name Salivary Glands Parietal cells Chief Cells Gastrin (hormone) Where it is released Mouth Stomach Stomach Stomach Enzyme or hormone Enzyme:Amylase Enzyme:Hydrochloric acid Enzyme: Intrinsic factor Enyzme: Pepsinogen Hormone Function Breaks down carbs Digestion Absorbs b12 Digests proteins Releases parietal/chief cells when stomach is stretched Produce bicarbonate Secretes into small intestine for digestion Stimulates acinar cells Inhibits acid production Inhibits secretory mechanisms Digestion of fats
Ductal Cells Acinar Cells
Pancreas Pancreas
Enzyme Enzyme
Cholescystokinin(CCK) Secretin
Pancreas/small intestine Pancreas/small intestine Pancreas/small intestine Pancreas
Enzyme Hormone
Somatostatin Lipase
Hormone Enzyme
Pharmacology:
1. Antacids: interacts with acids at chemical level to neutralize a. aluminum, calcium salts, magaldrate, magnesium salts, sodium bicarb 2. H2 antagonists: prevents gastrin from stimulating the release of hydrochloric acid
a. cimetadine, famotidine, nizatadine, ranitidine 3. Proton Pump Inhibitor: inhibits final step of acid production, lowers acid in stomach a. lanzoprazole, omeprazole, esomeprazole, pantoprazole, rabeprazole 4. Antipeptic agents:coats injured area of stomach to prevent further injury from acid,such as an ulcer a. sulcrafate 5. Prostaglandins: inhibits secretion of gastrin, protects lining of stomach a. misoprostol 6. Digestive enzymes: salivart, creon, pancrease
Oral Cancer
Facts: 1. Most common sites: lips, lateral aspects of tongue, floor of mouth 2. risk factors: smokeless tobacco, tobacco, alcohol 3. curable if discovered early Patho 1. Squamouse cell carcinoma: surface of epithelium, slow growing, dysplagia 2. Basal cell carcinoma: primarily on lips, ulcer with raised border Clincial Manifestations 1. early: few to none in early stages 2. late: painless sore/mass that does not heal a. progression to tenderness, difficulty chewing, swallowing/speaking, coughing up tinged sputum, enlarged cervical lymph nodes Diagnostics: Oral exam, cervical lymph nodes, biopsy, CT scan Medical Management: 1. surgical resection a. hemiglossectomy: tongue b. total glossectomy: whole tongue c. Neck dissection with reconstructive surgery, nursing care postop: maintain airway, wound flap, hemorrhage, pain management. 2. radiation 3.chemo More on neck dissection: 1. radical: all lymph nodes removed 2. modified radical: less severe 3. complications: a. chyle fistula: milk like drainage from thoracic duct
b. hemmorage c. nerve damage
Mandibular Fractures:
1. Lower jaw fracture: a. Close fractures 2. Medical Management: a. Rigid fixation b. Bone grafting 3. Nursing Management: a. wire cutters at bedside b. oral suction c. exposed wires d. liquid diet e. airway
Pancreatitis
Functions of pancreas: 1. endocrine: insulin, glucagon, somatostatin 2. exocrine: amylase (carbs), trypsin (protein), lipase (fats) Pancreatitis: 1. associated with escape of activated pancreatic enzymes into the pancreas and surrounding tissue (normally enzymes are inactive until it reaches the small intestine, see below for more patho) 2. enzymes cause fat necrosis (autodigestion) and produce fatty deposits in abdominal cavity 3. most cases are a result of gallstones and alcohol abuse Patho: Bilary obstruction: 1. gallstones occlude common duct 2. obstruct flow of secretions 3. reflux of pancreatic secretions back into pancreatic duct 4. enzymes are activated, leads to autodigestion, vasodilation, increased vascular permeability 5. fluid electrolyte disturbance leads to fluid shift to interstitial space, leads to hypovolemic, leads to shock Clinical Manifestations: 1. Constant, knife like pain in right upper quadrant radiating to back 2. abrupt onset, no relief with emesis 3. increased pain with food or lying down 4. nausea/vomiting 5. jaundice
6. rigid abdomen, bruising around flank Assessment and diagnosis: 1. history of abdominal pain, risk factors physical exam 2. increase in serum amylase and lipase 3. urinary amylase, BUN, creatinine 4. WBC elevated (above 16,000) 5. fall in H/H (fall below 10) 6. Peritoneal fluid 7. Steatorrhea 8. CT with contrast 9. X-ray 10. hypocalcemia (calcium gets caught in fat necrosis), (fall below 8) 11. fluid shift (greater than 6L) 12. ERCG: provides detailed anatomy and pancreas and pancreatic and bilary ducts (for chronic pancreatitis) Complications: 1. fluid shift: need IV hydration 2. hypocalcemia: supplement with calcium gluconate 3. hyperglycemia 4. hypoxemia 5. ileus; intestinal obstruction 6. DIC: treat with FFP 7. Infection: IV antibiotics 8. pseudocysts Medical Management: a. NPO b. NG sunction c. H2 antagonists, proton pump inhibitors: to decrease acid d. Pain management e. intensive care ( for hemodynamic monitoring) f. respiratory care g. biliary drainage: to reestablish drainage from pancreas h. surgical intervention i. relieve pain and discomfort j. steroids k. insulin for hyperglycemia
Pancreatic Cancer:
Facts: 1. 5th leading cause of cancer deaths in U.S. 2. Occurs most frequently in 5th to 7th decade 3. 2 5% survival rate at 5 yeras Risk Factors: smoking, high fat diet, meat, exposure to industrial chemicals/toxins. Clincial Manifestations: 1. Early: vague, non specific, rarely diagnosed early 2. Late: metastasis to other organs, symptoms of obstruction Diagnostics: 1. CEA19-9 tumor marker 2. amylase, lipase 3. CT scan 4. ERCP 5. biopsy 6. paracenesis. Medical Management: 1. Surgical resection 2. chemo/radiation 3. palliative care
Disorders of the liver:
Functions: see above in anatomy section for details 1. storage: iron, magnesium, minerals, fat soluble vit. ect. 2. protection: detoxifies drugs, phagocytes, ect. a. first pass effect: the break down medications as they are ingested. 3. metabolism: breaks down proteins into albumin, amino acids, ect. Hepatic dysfunction: causes: 1. primary liver disease a. acute or chronic 2. obstruction of bile flow 3. derangements of hepatic circulation: this is really part of primary disease Symptoms of liver disease: 1. jaundice: a. hemolytic: from destruction of RBCs
b. hepatocellular: inability of damaged liver cells to clear bilirubin from blood c. obstructive: occlusion of bile duct d. hyperbilirubinemia 2. portal hypertension: when blood cant get through the liver because of liver disease, pressure builds up in veins between gut and liver (kinda like pulmonary hypertentionkinda) a. two major consequences: ascites: increase in fluid in abdomen (see below) varices: veins are not designed to handle the pressure build up, dissection and aneurysms occur. (see below for more patho) 3. Ascites (see below) 4. Esophageal varices: (see below) Ascites: 1. patho a. obstruction in liver b. increased cap pressure c. loss of albumin (responsible for holding water into vascular space through osmotic pressure) d. fluid shift into intraperitoneal space 2. Clinical Manifestations: a. increased abdominal girth b. rapid weight gain 3. medical management: a. diet b. diuretics c. bedrest d. paracentesis: to remove fluid to mainly aid in breathing e. transjugular intrahepatic portosystemic shunt (TIPS): to relieve pressure build up within liver, the shunt bypasses the liver entirely 4. Nursing: a. I and O b. abdominal girth measurement c. daily weights d. labs: ammonium levels e. frequent rest periods f. small frequent meals Esophageal varices: 1. patho: a. dilated veins found in submucosa of lower esophagus b. the veins that are created for collateral circulation are not designed to handle increase in pressure
c. these veins can bleed easily d. patient will cough up tons of blood, (remember: GI responsible for 20% of cardiac output) 2. clinical manifestations: a. hematemesis: vomiting of blood b. melena: black stools c. shock d. mental physical deterioration 3. nursing: monitor H and H, transfuse as necessarily, monitor for bleeding 4. Diagnostics: a. endoscopy b. portal system pressures 5. medical management: a. vasopressin: causing vein constriction b. balloon tamponade: not as common, but this is be on the test. c. endoscopy d. surgury: TIPS procedure, portocaval shunt, splenorenal shunt, H-graft mesocaval shunt Cirrhosis of liver: chronic disease, normal liver tissue is replaced by fibrotic tissue, this disrupts liver function 1. Alcohol is primary cause 2. men more than women 3. three types of cirrhosis a. alcoholic: most common b. post necrotic: secondary to viral hepatitis, have intermittent function of the liver c. biliary: obstruction of bile ducts, this is usually acute, not chronic d. cryptogenic: idiopathic (we dont know what happens, yay!) 4. Compensated: early disease a. enlarged liver b. abdominal pain c. intermittent mild fever 5. decompensated: late disease a. ascites b. liver shrinks c. portal htn d. varicies e. wasting syndrome f. bruising g. high risk for infection 6. Diagnostics: a. labs: ALT, AST, Bilirubin,ammonium levels : all go up. HandH and Electrolytes go down b. liver biopsy: need to lie on right side on a pillow that provides pressure
c. CT, MRI, ultrasound, radio-isotope liver scan 7. Medical management: a. treatment is symptomatic b. ETOH abstinence c. Medications: PPI, H2 blockers, antacids d. nutrition: low protein, high calorie diet Hepatic Encephalopathy: accumulation of ammonia and toxic metabolites in blood and brain, often associated with portal hypertension 1. patho: a. liver cells unable to convert to ammonia to urea b. causes brain dysfunction and damage c. by product of protein metabolism is ammonia 2. Clinical manifestations a. dementia type symptoms b. mood changes ect. c. asterixix: flapping tremor of hands 3. Assessment and diagnostics: a. ammonia level elevation b. EEG: shows generalized slowing c. fetor hepaticus: sweet slightly fecal odor to breath 4. Medical management; a. lactulose: promotes excretion of ammonia b. beomycin: suppress gi bacteria that produce ammonia c. avoid sedatives, tranquilizers, analgesics, tylenol, small frequent meals
Gastric cancer
Facts: 1. more men than women 2. diet of smoked foods, without fruits and vegs 3. chronic inflammation 4. poor prognosis, even at early stages 5. associated with pyloric obstruction, bleeding, severe pain, gastric perforation Patho: 1. adenocarcinoma most common, 86% occur in lining of stomach 2. can occur anywhere in stomach 3. tumor infiltrates surrounding mucosa Clinical manifestations 1. early: usually asymptomatic, pain relieved with antacids
2. late: dyspepsia (indigestion), anorexia, abdominal pain, constipation, anemia, weight loss, get full quickly from eating 3. commonly goes to liver, pancreas, esophagus, colon. Assessment and diagnostics: 1. EGD with biopsies, cytology 2. stools for occult blood 3. complete blood count Medical management: 1. surgery, removal of tumor a. complications: anastamosis leak, blood clots, bowel obstruction, B12 def, esophagitis, osteoporosis 2. pallative care common because the body loses the ability to absorb nutrients, and dumping/wasting syndrome develops Nursing care: 1. TPN post op, monitor electrolytes ect. a. high risk for infection due to high glucose of TPN b. need glucose checks 2. treatment of surgical wound
Colon cancer:
1. Patho: a. risking from lining of colon b. usually starts as benign polyp c. transforms to malignancy d. invades, destroys normal tissues 2. facts: a. third leading cause of cancer that is at primary site, not metastasized b. family history, chronic inflammation, high fat low fiber diets are all risk factors c. 95% adenocarcinoma 3. clinical manifestations: a. number one: change in bowel habits b. blood in stools c. unexplained anemia d. weight loss and fatigue e. right sided: dull abdominal pain, melana(black stools) f. left sided: associated with obstruction, abdominal pain, cramping, narrowing stools, constipation, distention, bright red blood. g. rectal lesion: painful straining at stool, rectal pain, feeling of incomplete evacuation
4. assessments/diagnostics a. stools for occult blood b. colonoscopy c. labs: CEA, usually done after cancer treatment to see if tumor has been eradicated 5. complications: obstruction, hemorrhage, perforation, sepsis, shock 6. Medical management: surgery is number one choice 7. Nursing management: a. nutrition: TPN or IVF until bowel function returns b. slow advancement of diet c. trail and error to find foods that control constipation or diarrhea 8. chart 38-10 on irrigating colostomy
Potrebbero piacerti anche
- Fundamentals of NursingDocumento8 pagineFundamentals of NursingFreeNursingNotes92% (13)
- Acute Renal Failure-Student-Rapid ReasoningDocumento4 pagineAcute Renal Failure-Student-Rapid Reasoningapi-268403950Nessuna valutazione finora
- Gastrointestinal DiseasesDocumento11 pagineGastrointestinal DiseasesFreeNursingNotes100% (1)
- Endocrine NursingDocumento2 pagineEndocrine NursingUnclePorkchop94% (34)
- Handout Medical-Surgical Nursing Fluid and ElectrolyteDocumento13 pagineHandout Medical-Surgical Nursing Fluid and ElectrolytePaul Christian P. Santos, RN100% (10)
- Physical Assessment Charting For NursingDocumento7 paginePhysical Assessment Charting For NursingChristine Schroeder92% (13)
- Cardiac Med ChartsDocumento6 pagineCardiac Med ChartsNursingSchoolNotes100% (15)
- Jesus Hold My Hand EbDocumento2 pagineJesus Hold My Hand EbGregg100% (3)
- Gastrointestinal NursingDocumento8 pagineGastrointestinal Nursingohsnapitslei90% (10)
- Peds 2301 Exam #1Documento72 paginePeds 2301 Exam #1Jenni100% (3)
- Medication Calculation - Commonly Used FormulasDocumento1 paginaMedication Calculation - Commonly Used FormulasAaron AntonioNessuna valutazione finora
- Chart of Neuro DisordersDocumento1 paginaChart of Neuro DisordersNursingSchoolNotes100% (2)
- Fluid and ElectrolytesDocumento13 pagineFluid and ElectrolytesHenry Philip93% (15)
- GI NursingDocumento14 pagineGI NursingKarl Bayonito100% (5)
- Endocrine System Review NotesDocumento8 pagineEndocrine System Review Notesjeshema100% (1)
- Gastrointestinal DisordersDocumento12 pagineGastrointestinal Disorderssophia yemane100% (4)
- Pharm - Understanding Common GI Drugs (NURSING)Documento2 paginePharm - Understanding Common GI Drugs (NURSING)Linsey Bowen100% (4)
- Med Surge 2 - RESP SYSTEM NOTESDocumento26 pagineMed Surge 2 - RESP SYSTEM NOTESlorrainenxumalo75% (4)
- Nursing Cheat SheetDocumento1 paginaNursing Cheat Sheetabardwell100% (85)
- Chapter 16: Fluid, Electrolyte, and Acid-Base Imbalances Harding: Lewis's Medical-Surgical Nursing, 11th EditionDocumento13 pagineChapter 16: Fluid, Electrolyte, and Acid-Base Imbalances Harding: Lewis's Medical-Surgical Nursing, 11th EditionKrishna RamaNessuna valutazione finora
- Medical Surgical Nursing 64 PagsDocumento64 pagineMedical Surgical Nursing 64 Pagstanya nNessuna valutazione finora
- Unit 8 Med Surg Study Guide NursingDocumento5 pagineUnit 8 Med Surg Study Guide Nursingatl_nurse_student100% (7)
- Chart of Neuro DisordersDocumento1 paginaChart of Neuro DisordersNursingSchoolNotes100% (2)
- Chapter 14 Fluid and Electrolytes ChartsDocumento7 pagineChapter 14 Fluid and Electrolytes ChartsBNA_RN100% (3)
- Gastro Intestinal SystemDocumento9 pagineGastro Intestinal SystemJe Lyn100% (1)
- 3.26.12 Treatment of GI DisordersDocumento6 pagine3.26.12 Treatment of GI DisordersDiana Hylton100% (4)
- Fundamentals of Nursing PDocumento31 pagineFundamentals of Nursing Papi-26587879100% (4)
- Ignatavicius Renal QuestionsDocumento9 pagineIgnatavicius Renal Questionsboogie02100% (5)
- Iggy Med Surg Test Bank Chapter 007Documento10 pagineIggy Med Surg Test Bank Chapter 007Tracy Bartell100% (5)
- Gastrointestinal System and Nutrition Drug ChartsDocumento3 pagineGastrointestinal System and Nutrition Drug ChartsNursingSchoolNotesNessuna valutazione finora
- Med-Surg LEWIS 47 Final Foofed UpDocumento10 pagineMed-Surg LEWIS 47 Final Foofed Uphariniliaankhen100% (1)
- The GastroDocumento25 pagineThe Gastroangel_maui100% (7)
- Neuro Study GuideDocumento11 pagineNeuro Study GuideEllen Hennings100% (1)
- Med SurgDocumento82 pagineMed SurgRam Nik100% (4)
- Pediatric Nursing: Immediate Care For Newborn (OLD)Documento8 paginePediatric Nursing: Immediate Care For Newborn (OLD)KristaRicaAbayabayNessuna valutazione finora
- Handout OB MidtermsDocumento3 pagineHandout OB Midtermsaidan valin100% (7)
- Endocrine NursingDocumento8 pagineEndocrine NursingBunny Bonny100% (5)
- Blue Print Final Class Med Surg IIDocumento9 pagineBlue Print Final Class Med Surg IIbaconhater100% (1)
- Upper GI Disorders Study GuideDocumento10 pagineUpper GI Disorders Study Guidemelpietrowski100% (1)
- Maternity Nursing ReviewDocumento54 pagineMaternity Nursing ReviewJr Robis100% (6)
- GI Ch.44-47Documento40 pagineGI Ch.44-47W11795800% (1)
- Peds Final Exam Study GuideDocumento47 paginePeds Final Exam Study GuideSammy Levuong100% (1)
- Pediatric Nursing Reviewer CardiovascularDocumento4 paginePediatric Nursing Reviewer CardiovascularJemy Lorane TemporalNessuna valutazione finora
- Gastrointestinal Nclex Questions Part 2Documento11 pagineGastrointestinal Nclex Questions Part 2Manilyn Delos Reyes Patlunag100% (1)
- Vitamin Chart 2Documento3 pagineVitamin Chart 2surviving nursing schoolNessuna valutazione finora
- MH AtiDocumento2 pagineMH Atitotodile2395% (19)
- Pediatric Nursing Reviewer - NurseslabsDocumento5 paginePediatric Nursing Reviewer - NurseslabsDyanne BautistaNessuna valutazione finora
- Endocrine Disorders (Study Notes)Documento11 pagineEndocrine Disorders (Study Notes)Danelle Harrison, RN90% (10)
- Medical Surgical Nursing LOWER GIDocumento4 pagineMedical Surgical Nursing LOWER GIgeanie100% (2)
- Pharmacology For Nursing. Richard A. LehneDocumento62 paginePharmacology For Nursing. Richard A. LehneJC Ortiz-Carrillo50% (2)
- Med Surg BulletsDocumento35 pagineMed Surg Bulletscfournier1982Nessuna valutazione finora
- Thorax, Skin, Hair, Nails ObjectivesDocumento3 pagineThorax, Skin, Hair, Nails Objectivesctramel001100% (1)
- ATI Capstone Content Review Tips of The Week 3Documento16 pagineATI Capstone Content Review Tips of The Week 3nicki schefflerNessuna valutazione finora
- Pediatric Nursing Review NleDocumento56 paginePediatric Nursing Review Nlemarygrace canoNessuna valutazione finora
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDa EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNessuna valutazione finora
- MATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideDa EverandMATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideNessuna valutazione finora
- CLINICAL SPECIALIST IN MEDICAL-SURGICAL NURSING: Passbooks Study GuideDa EverandCLINICAL SPECIALIST IN MEDICAL-SURGICAL NURSING: Passbooks Study GuideValutazione: 4 su 5 stelle4/5 (1)
- Dimensional Analysis For Nursing StudentsDa EverandDimensional Analysis For Nursing StudentsNessuna valutazione finora
- CRITICAL THINKING IN CLINICAL NURSING PRACTICE (RN): Passbooks Study GuideDa EverandCRITICAL THINKING IN CLINICAL NURSING PRACTICE (RN): Passbooks Study GuideNessuna valutazione finora
- Resp Lecture NotesDocumento17 pagineResp Lecture NotesNursingSchoolNotes100% (3)
- Neuro Study GuideDocumento7 pagineNeuro Study GuideNursingSchoolNotes100% (2)
- ECG StripsDocumento5 pagineECG StripsNursingSchoolNotes100% (1)
- Pain Med ChartsDocumento4 paginePain Med ChartsNursingSchoolNotesNessuna valutazione finora
- Endocrine Study GuideDocumento4 pagineEndocrine Study GuideNursingSchoolNotes100% (1)
- Adult III Cardiac Study GuideDocumento15 pagineAdult III Cardiac Study GuideNursingSchoolNotes100% (6)
- Psych Med ChartsDocumento5 paginePsych Med ChartsNursingSchoolNotes100% (5)
- OB Drug ChartsDocumento2 pagineOB Drug ChartsNursingSchoolNotesNessuna valutazione finora
- Unit 4 Study Guide Part 2Documento7 pagineUnit 4 Study Guide Part 2NursingSchoolNotesNessuna valutazione finora
- Gastrointestinal System and Nutrition Drug ChartsDocumento3 pagineGastrointestinal System and Nutrition Drug ChartsNursingSchoolNotesNessuna valutazione finora
- Cardiac Stuff That You Have To MemorizeDocumento1 paginaCardiac Stuff That You Have To MemorizeNursingSchoolNotes100% (1)
- Pulmonary Med Charts Part 2Documento2 paginePulmonary Med Charts Part 2NursingSchoolNotes100% (3)
- Haryana at A Glance: Geographical AreaDocumento1 paginaHaryana at A Glance: Geographical AreasonuNessuna valutazione finora
- Bike Chasis DesignDocumento7 pagineBike Chasis Designparth sarthyNessuna valutazione finora
- Project Report Devki Nandan Sharma AmulDocumento79 pagineProject Report Devki Nandan Sharma AmulAvaneesh KaushikNessuna valutazione finora
- Listening Fill in The Gaps and ExercisesDocumento4 pagineListening Fill in The Gaps and ExercisesAdriano CamargoNessuna valutazione finora
- National Healthy Lifestyle ProgramDocumento6 pagineNational Healthy Lifestyle Programmale nurseNessuna valutazione finora
- Agitha Diva Winampi - Childhood MemoriesDocumento2 pagineAgitha Diva Winampi - Childhood MemoriesAgitha Diva WinampiNessuna valutazione finora
- Orchestral Tools - The Orchestral Grands ManualDocumento12 pagineOrchestral Tools - The Orchestral Grands ManualPiotr Weisthor RóżyckiNessuna valutazione finora
- AFI 90-901 Operational Risk ManagementDocumento7 pagineAFI 90-901 Operational Risk ManagementJohan Lai100% (1)
- Cotton Pouches SpecificationsDocumento2 pagineCotton Pouches SpecificationspunnareddytNessuna valutazione finora
- Cooking Oils and Smoke Points - What To Know and How To Choose The Right Cooking Oil - 2020 - MasterClassDocumento7 pagineCooking Oils and Smoke Points - What To Know and How To Choose The Right Cooking Oil - 2020 - MasterClasschumbefredNessuna valutazione finora
- Directory of Schools For The Deaf in The PhilippinesDocumento6 pagineDirectory of Schools For The Deaf in The PhilippinesVERA Files100% (1)
- A Mercy Guided StudyDocumento23 pagineA Mercy Guided StudyAnas HudsonNessuna valutazione finora
- DB - Empirically Based TheoriesDocumento3 pagineDB - Empirically Based TheoriesKayliah BaskervilleNessuna valutazione finora
- 6977 - Read and Answer The WorksheetDocumento1 pagina6977 - Read and Answer The Worksheetmohamad aliNessuna valutazione finora
- Economic Survey 2023 2Documento510 pagineEconomic Survey 2023 2esr47Nessuna valutazione finora
- Latvian Adjectives+Documento6 pagineLatvian Adjectives+sherin PeckalNessuna valutazione finora
- PDF - Unpacking LRC and LIC Calculations For PC InsurersDocumento14 paginePDF - Unpacking LRC and LIC Calculations For PC Insurersnod32_1206Nessuna valutazione finora
- Peptic UlcerDocumento48 paginePeptic Ulcerscribd225Nessuna valutazione finora
- 2nd Quarter Exam All Source g12Documento314 pagine2nd Quarter Exam All Source g12Bobo Ka100% (1)
- 06 Ankit Jain - Current Scenario of Venture CapitalDocumento38 pagine06 Ankit Jain - Current Scenario of Venture CapitalSanjay KashyapNessuna valutazione finora
- أثر البحث والتطوير على النمو الاقتصادي - دراسة قياسية لحالة الجزائر (1990 -2014)Documento17 pagineأثر البحث والتطوير على النمو الاقتصادي - دراسة قياسية لحالة الجزائر (1990 -2014)Star FleurNessuna valutazione finora
- Divorced Women RightsDocumento41 pagineDivorced Women RightsAnindita HajraNessuna valutazione finora
- TG - Health 3 - Q3Documento29 pagineTG - Health 3 - Q3LouieNessuna valutazione finora
- COSL Brochure 2023Documento18 pagineCOSL Brochure 2023DaniloNessuna valutazione finora
- 1 3 Quest-Answer 2014Documento8 pagine1 3 Quest-Answer 2014api-246595728Nessuna valutazione finora
- Pre-Boarding Announcement Skill Focus: ListeningDocumento5 paginePre-Boarding Announcement Skill Focus: ListeningJony SPdNessuna valutazione finora
- Surge Protectionfor ACMachineryDocumento8 pagineSurge Protectionfor ACMachineryvyroreiNessuna valutazione finora
- The Trial of Jesus ChristDocumento10 pagineThe Trial of Jesus ChristTomaso Vialardi di Sandigliano100% (2)