Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ontario Municipalities Benchmarking Initiative - EMS
Caricato da
sebastienperthDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Ontario Municipalities Benchmarking Initiative - EMS
Caricato da
sebastienperthCopyright:
Formati disponibili
7.
EMERGENCY MEdICAL SERVICES
What is the Service?
Emergency Medical Services (EMS), often referred to as ambulance or paramedic services, provides emergency care to stabilize a patients condition, initiates rapid transport to hospitals, and facilitates both emergency and non-emergency transfers between medical facilities. Specific objectives include: All citizens should have equal access to ambulance service Ambulance services are an integrated part of the overall Emergency Health Care Services Closest available and appropriate ambulance responds to a patient regardless of political, administrative or other artificial boundaries Ambulance service operators are medically, operationally and financially accountable to provide service of the highest possible caliber Ambulance services must adapt to the changing health care, demographic, socio-economic and medical needs in their area
What should you consider when reviewing the results?
Each municipalitys results are influenced to varying degrees by a number of factors, including: Demographics Governance Hospital Delay Non Residents Specialized Services
Age and health status of the population has an impact on number and severity of calls. An older population can increase the demand for services, as can seasonal visitors and the inflow of workers from other communities during the day.
Budgeted resources, Local Response Times Standards or Deployment Plans are mandated by Council. Services face varying lengths of delays in the off-load of passengers at local hospitals, which can impact the resources required and availability to respond to calls. Visitors, workers, tourists and out of town hospital patients not reflected in the measures (population is that of municipality only). Tactical teams, multi-patient transport units, bike and marine teams are increasingly being provided by the larger municipalities. Also, costs can be impacted by higher wage rates of advanced care (ADP) vs. primary care (PCP) paramedics. Mix of urban versus rural geography can influence response time and cost factors. Congestion can make navigating roads more difficult, resulting in significant delays. Urban centres with taller buildings can impact response times, i.e. responses to high level apartment/condo units. Large rural geographic areas can make it challenging to provide cost-effective, timely emergency coverage. Services use a varying mixture of response vehicles which have differing levels of staffing.
Urban vs. Rural
Vehicle Mix
PARTNERING FOR SERVICE EXCELLENCE
31
EMERGENCY MEdICAL SERVICES What are the results?
Fig. 7.1 total eMS Responses Reponses per Fig. 7.1 - Total EMS per 1,000 Population 1,000 population
How many calls were responded to by EMS providers?
200 150
Fig. 7.1 - Total EMS Reponses per 1,000 population
50 200 0 150 DUR
84 83 87
100
HAL
63 65 63
HAM
121 123 127
LON
95 96 98
MUSK
85 89 72
NIAG
97 98 102
OTT
113 120 108
SUD
181 149 138
TBAY
167 175 183
TOR
112 107 115
WAT
65 67 65
WIND
116 116 119
YORK
64 62 62
MED
97 98 102
100 2008 50 2009
2010
0 Fig. 7.2 - EMS TO-2 Code 4, 90th Percentile Response Time (EMDS 419B and 419C)
Source: eMDS229 (Service Level)
DUR
HAL
HAM
LON
MUSK
NIAG
OTT
SUD
TBAY
TOR
WAT
WIND
YORK
MED
Fig. 7.2 - EMS TO-2 Code 4, 90th Percentile Response Time (EMDS 419B and 419C) 5:00
4:00 How long does it take to dispatch a call? 2:00 8:00 1:00 7:00 0:00 6:00 5:00 4:00 3:00 2:00 1:00 0:00 3:00 Fig. 7.2 eMS to-2 Code 4, 90th Percentile Response time (mm:ss)
Figure 7.1 illustrates how many calls the EMS provider is receiving per capita. The services in Sudbury and 8:00 Thunder Bay do more non-emergency patient transfers than the other services (which are generally done 7:00 by private contractors in other municipalities) which explains their much higher call volumes. Overall, EMS 6:00 responses have increased by 3.7% in the last year.
DUR
HAL
HAM
LON
MUSK
NIAG
OTT
SUD
TBAY
TOR
WAT
WIND
YORK
MED
DUR
02:15
HAL
02:43
HAM
03:09
LON
02:39
MUSK
07:35
NIAG
01:50
OTT
02:25
SUD
02:20
TBAY
02:05
TOR
03:24
WAT
03:33
WIND
03:35 03:37
YORK
02:37 02:43
MED
2:39 2:48
Fig. 7.3 -02:34 Revised T203:01 02:44 Percentile Response Time03:28 02:20 408, 408A) EMS 02:50 - 4 Code 4, 90 (EMDS 415A, 03:15 03:36 2010 01:51 02:46
Source: eMDS419B and eMDS419C (Customer Service)
2009
Fig. 7.3 - EMS Revised T2 - 4 Code 4, 90 Percentile Response Time (EMDS 415A, 408, 408A) 15:00
10:00 5:00 25:00 0:00 20:00 DUR HAL HAM LON MUSK NIAG OTT SUD TBAY TOR
Figure 7.2 shows the time from a phone call being received to the EMS unit being notified (dispatched) 25:00 for the highest priority calls (Code 4). The 90th percentile means that 90% of all calls of the service have a 20:00 dispatch time within the period reflected in the graph, thus limiting extreme situations.
15:00 10:00
WAT
WIND
YORK
MED
32
5:00 2010 PERFORMANCE BENCHMARKING REPORT 0:00 DUR HAL HAM LON MUSK NIAG OTT SUD TBAY TOR WAT WIND YORK MED
0:00
DUR
HAL
HAM
LON
MUSK
NIAG
OTT
SUD
TBAY
TOR
WAT
WIND
YORK
MED
How long does it take to respond to a dispatched call?
Fig. 7.3 eMS Revised t2-4 Code 4, 90th Percentile Response time (mm:ss)
EMERGENCY MEdICAL SERVICES Fig. 7.3 - EMS Revised T2 - 4 Code 4, 90 Percentile Response Time (EMDS 415A, 408, 408A)
25:00
20:00 Fig. 7.3 - EMS Revised T2 - 4 Code 4, 90 Percentile Response Time (EMDS 415A, 408, 408A) 15:00 10:00 25:00 5:00 20:00 0:00 15:00 10:00 1996 5:00 2009 0:00 2010
DUR
10:04 10:46
HAL
10:32 10:33 10:16
HAM
10:03 10:17
LON
9:29 9:10
MUSK
20:44 19:00
NIAG
10:48 09:37
OTT
12:33 11:51 10:59
SUD
12:12 10:23
TBAY
10:14 10:48
TOR
9:59 10:09
WAT
10:30 11:47
WIND
10:23 09:49
YORK
11:33 12:37
MED
10:30 10:33
Source: eMDS415A and eMDS408 and eMDS408A (Customer Service) (Response) Note: As set out by the Province, the 1996 information is considered to be the base year standard that service is expected to match.
DUR
10:43
HAL
HAM
10:15
LON
9:21
MUSK
19:00
NIAG
09:45
OTT
SUD
10:26
TBAY
11:33
TOR
10:38
WAT
12:02
WIND
09:45
YORK
12:52
MED
10:38
Fig. 7.4 - Percent of Ambulance Time Lost to Hospital Turnaround
Figure 7.3 indicates how long it takes from the time a call is received to when the EMS unit arrives on the scene for the highest priority calls (Code 4).
Fig. 7.4 - Percent of Ambulance Time Lost to Hospital Turnaround
20% What percent of time do ambulances spend at the hospital? 15% Fig. 7.4 Percent of Ambulance time Lost to Hospital turnaround 10% 30% 5% 25% 0% 20% 15% 10% 5% 0% DUR HAL HAM LON MUSK NIAG OTT SUD TBAY TOR WAT DUR HAL HAM LON MUSK NIAG OTT SUD TBAY TOR WAT
30% Muskoka results are noticeably higher primarily due to a very large geographical area with a relatively small population base, and they service a high volume of seasonal residents and visitors. 25%
WIND
YORK
MED
WIND
YORK
MED
Fig. 7.5 - EMS Actual Weighted Vehicle29.9% 8.3% 17.6% 23.8% 1,000 13.6% 20.6% 13.6% In-Service Hours per 17.7% population 2008 13.0% 13.1% 19.8% 13.5% 10.9% 12.4%
2009 800 15.5% 16.3% 14.1% 13.1% 20.7% 20.0% 13.4% 13.6% 5.7% 0.1% 12.2% 13.1% 27.2% 26.4% 8.6% 10.8% 19.3% 21.6% 21.1% 20.9% 18.3% 19.2% 14.4% 15.8% 19.8% 19.6% 15.5% 16.3%
600 Source: eMDS150 (Community Impact) 500 Fig. 7.5 - EMS Actual Weighted Vehicle In-Service Hours per 1,000 population 400 Figure 7.4 shows the percent of time ambulances are spending at the hospital. This includes the time it takes to300 transfer the patient, delays in transfer of care due to a lack of hospital resources (commonly referred to 800 200 as off-load delay), paperwork, and other activities. 700 100 600 The0significance of the time spent in the hospital is that the more time spent by paramedics in the hospital 500 process,DUR less time they are available onNIAG road to respondTBAY TOR WAT WIND YORK MED the HAL HAM LON MUSK the OTT SUD to emergency calls. 400 300 200 100 0 DUR HAL HAM LON MUSK NIAG OTT SUD TBAY TOR WAT In-Service MED Fig. 7.6 - EMS Actual Operating Cost per Actual Weighted Vehicle WIND YORK Hour
700 2010
PARTNERING FOR SERVICE EXCELLENCE
$250
33
0%
DUR
HAL
HAM
LON
MUSK
NIAG
OTT
SUD
TBAY
TOR
WAT
WIND
YORK
MED
EMERGENCY MEdICAL SERVICES
How many hours of ambulance service are provided in the community for every 1,000 people? Fig. 7.5 - EMS Actual Weighted Vehicle In-Service Hours per 1,000 population
Fig. 7.5 eMS Actual Weighted Vehicle In-Service Hours per 1,000 Population
Fig. 7.5 - EMS Actual Weighted Vehicle In-Service Hours per 1,000 population 800
700 800 600 700 500 600 400 500 300 400 200 300 100 200 0 100 0
DUR
306 DUR 297 303
HAL
250 HAL 251 249
HAM
363 HAM 349 368
LON
338 LON 343 349
MUSK
647 MUSK 638 628
NIAG
408 NIAG 399 438
OTT
290 OTT 307 326
SUD
628 SUD 644 652
TBAY
464 TBAY 462 450
TOR
266 TOR 244 248
WAT
194 WAT 196 193
WIND
425 WIND 410 412
YORK
238 YORK 264 263
MED
338 MED 343 349
2008 2009 2010
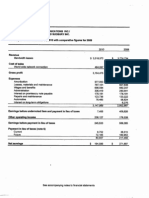
Fig. 7.6 - EMS Actual Operating Cost per Actual Weighted Vehicle In-Service Hour
Source: eMDS225A
Fig. 7.6 - EMS Actual Operating Cost per Actual Weighted Vehicle In-Service Hour
How much does it cost to provide one hour of ambulance service?
Fig. 7.6 eMS Actual operating Cost per Actual Weighted Vehicle In-Service Hour
$250
$200 $250 $150 $200 $100 $150 $50 $100 $0 $50 $0
2008 2009 2010
DUR DUR
$149 $160 $174
HAL HAL
$158 $164 $169
HAM HAM
$151 $168 $159
LON LON
$146 $146 $148
MUSK MUSK
$125 $147 $145
NIAG NIAG
$131 $149 $159
OTT OTT
$184 $196 $195
SUD SUD
$146 $154 $161
TBAY TBAY
$140 $147 $157
TOR TOR
$185 $205 $232
WAT WAT
$150 $159 $173
WIND WIND
$146 $175 $171
YORK YORK
$159 $163 $164
MED MED
$149 $160 $164
Source: eMDS305A (efficiency)
Figure 7.6 shows the cost per hour to have an EMS vehicle available to respond to patient calls. Although the full cost of the service including administrative costs, medical supply costs, building operating costs, supervision and overhead are included, only the hours that vehicles are available for service are used. As wages, fuel and other costs increase, this measure will also trend upwards.
34
2010 PERFORMANCE BENCHMARKING REPORT
Potrebbero piacerti anche
- Social Media To DatatelDocumento10 pagineSocial Media To DatatelsebastienperthNessuna valutazione finora
- Datamining LinkedInDocumento5 pagineDatamining LinkedInsebastienperthNessuna valutazione finora
- LU Alumni Web RedesignDocumento10 pagineLU Alumni Web RedesignsebastienperthNessuna valutazione finora
- Statement of Claim - Solid Gold and OntarioDocumento11 pagineStatement of Claim - Solid Gold and OntariosebastienperthNessuna valutazione finora
- Ontario Securities Commission PresentationDocumento36 pagineOntario Securities Commission PresentationsebastienperthNessuna valutazione finora
- Communications CalendarDocumento2 pagineCommunications CalendarsebastienperthNessuna valutazione finora
- Lazyone Catalogue 2014Documento112 pagineLazyone Catalogue 2014sebastienperthNessuna valutazione finora
- Ontario Statement of DefenceDocumento13 pagineOntario Statement of DefencesebastienperthNessuna valutazione finora
- Lazyone Cat 2012Documento100 pagineLazyone Cat 2012sebastienperthNessuna valutazione finora
- Lazy OneDocumento8 pagineLazy OnesebastienperthNessuna valutazione finora
- Cinefest Launch PresentationDocumento24 pagineCinefest Launch PresentationsebastienperthNessuna valutazione finora
- Agilis Networks Financial StatementsDocumento2 pagineAgilis Networks Financial StatementssebastienperthNessuna valutazione finora
- Herman Reich - AllegationsDocumento1 paginaHerman Reich - AllegationssebastienperthNessuna valutazione finora
- SudburyROCKS Relay ResultsDocumento4 pagineSudburyROCKS Relay ResultssebastienperthNessuna valutazione finora
- Royal LePage Recreational Property Report 2013Documento22 pagineRoyal LePage Recreational Property Report 2013sebastienperthNessuna valutazione finora
- Council Office Expenses 2010Documento20 pagineCouncil Office Expenses 2010sebastienperthNessuna valutazione finora
- Letter From OPP After Transit Ticket InvestigationDocumento2 pagineLetter From OPP After Transit Ticket InvestigationsebastienperthNessuna valutazione finora
- SudburyROCKS Marathon ResultsDocumento3 pagineSudburyROCKS Marathon ResultssebastienperthNessuna valutazione finora
- Ombudsman Statement On SudburyDocumento1 paginaOmbudsman Statement On SudburysebastienperthNessuna valutazione finora
- Errington-Vermillion Fact SheetDocumento4 pagineErrington-Vermillion Fact SheetsebastienperthNessuna valutazione finora
- Transition Metals Fact SheetDocumento4 pagineTransition Metals Fact SheetsebastienperthNessuna valutazione finora
- SudburyROCKS Half-Marathon ResultsDocumento9 pagineSudburyROCKS Half-Marathon ResultssebastienperthNessuna valutazione finora
- Ombudsman Response To April 3 LetterDocumento2 pagineOmbudsman Response To April 3 LettersebastienperthNessuna valutazione finora
- Council Office Expenses 2011Documento39 pagineCouncil Office Expenses 2011sebastienperthNessuna valutazione finora
- Council Emails About OmbudsmanDocumento6 pagineCouncil Emails About OmbudsmansebastienperthNessuna valutazione finora
- Contract Award To IBI GroupDocumento3 pagineContract Award To IBI GroupsebastienperthNessuna valutazione finora
- Subdivision Activity MapsDocumento9 pagineSubdivision Activity MapssebastienperthNessuna valutazione finora
- OMB Appeal South EndDocumento1 paginaOMB Appeal South EndsebastienperthNessuna valutazione finora
- OLG Press ReleaseDocumento2 pagineOLG Press ReleasesebastienperthNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Nigeria - List of Medical Facilities - GOV - UKDocumento12 pagineNigeria - List of Medical Facilities - GOV - UKqueenieth amuzieNessuna valutazione finora
- Josh Moulin - Covert Entry TacticsDocumento5 pagineJosh Moulin - Covert Entry TacticsJosh MoulinNessuna valutazione finora
- Json Definitivo Label RXDocumento3 pagineJson Definitivo Label RXAnderson Manuel Marquez NuñezNessuna valutazione finora
- AssignmentDocumento5 pagineAssignmentClaire ChiuNessuna valutazione finora
- Study Material Powerpoint EbpDocumento15 pagineStudy Material Powerpoint EbpGLORY MI SHANLEY CARUMBANessuna valutazione finora
- Pressure Ulcers Project - EditedDocumento6 paginePressure Ulcers Project - EditedZeera MohamadNessuna valutazione finora
- 1916 PDFDocumento244 pagine1916 PDFAvijit PorelNessuna valutazione finora
- MQ Mop-Up Notification MBBS Course 2021Documento3 pagineMQ Mop-Up Notification MBBS Course 2021Feroz FerozNessuna valutazione finora
- Home Healthcare PlanDocumento6 pagineHome Healthcare PlanAhmedNessuna valutazione finora
- Timetable 21074 X4-T4Documento8 pagineTimetable 21074 X4-T4Gabriel MerriwetherNessuna valutazione finora
- Test BankDocumento6 pagineTest BankKazama SmithNessuna valutazione finora
- Street Address in Ghana - Google Search PDFDocumento1 paginaStreet Address in Ghana - Google Search PDFCollins SmithNessuna valutazione finora
- Korean Around TownDocumento2 pagineKorean Around Townxd아우로라Nessuna valutazione finora
- Oasis Cable Pvt. LTD.: Floor Batra Complex, 19 Civil Lines ROORKEE Floor Rohini Plaza DheradunDocumento4 pagineOasis Cable Pvt. LTD.: Floor Batra Complex, 19 Civil Lines ROORKEE Floor Rohini Plaza DheradunSumit ChoudharyNessuna valutazione finora
- Assignment 2 Richa MaamDocumento3 pagineAssignment 2 Richa MaamBrandon WaikhomNessuna valutazione finora
- External Query LetterDocumento2 pagineExternal Query LetterRohan RedkarNessuna valutazione finora
- Leveraging FSM To Close The Urban Sanitation Loop in KampalaDocumento15 pagineLeveraging FSM To Close The Urban Sanitation Loop in KampalaLego EdrisaNessuna valutazione finora
- Case Study ThreeDocumento18 pagineCase Study ThreeHsuan-Yen HuangNessuna valutazione finora
- Format For Listing Empaneled Providers For Uploading in State/UT WebsiteDocumento17 pagineFormat For Listing Empaneled Providers For Uploading in State/UT WebsiteSpace HR100% (1)
- Roehampton Hospital Case Study - Part 2Documento2 pagineRoehampton Hospital Case Study - Part 2akhil paulNessuna valutazione finora
- Barangay Council Approves Disaster Risk Reduction CommitteeDocumento5 pagineBarangay Council Approves Disaster Risk Reduction CommitteeALDINNessuna valutazione finora
- Merit List PMMGDocumento84 pagineMerit List PMMGNayaaNessuna valutazione finora
- Alejandra Resume2Documento2 pagineAlejandra Resume2api-669170011Nessuna valutazione finora
- Test Bank Pharmacotherapy Principles and Practice 4th EditionDocumento24 pagineTest Bank Pharmacotherapy Principles and Practice 4th EditionMrWayneCollierDVMibep100% (32)
- HDFC Claims FAQDocumento3 pagineHDFC Claims FAQPrashanth NairNessuna valutazione finora
- STP Ex BestindoDocumento3 pagineSTP Ex BestindoAlvin Novandi Ega PradanaNessuna valutazione finora
- Patient Profile: MSC Clinical PharmacyDocumento2 paginePatient Profile: MSC Clinical PharmacyWu TracyNessuna valutazione finora
- List of Government Hospital.: 1st Main RD, Govindaraja NagarDocumento2 pagineList of Government Hospital.: 1st Main RD, Govindaraja NagarShamanth MNessuna valutazione finora
- Introduction 1Documento17 pagineIntroduction 1Ahmed UburiNessuna valutazione finora
- AssessmentDocumento2 pagineAssessmentelishaNessuna valutazione finora