Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Chapter 6 Marieb
Caricato da
mjhenkeDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Chapter 6 Marieb
Caricato da
mjhenkeCopyright:
Formati disponibili
Chapter 6 Skeletal System Functions of the skeletal system/bone 1.
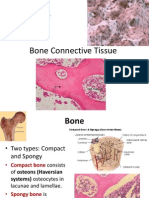
Support skeletal system is the internal framework of the body 2. Protection protects internal organs 3. Movement muscles & bones work together. muscles move bones as levers 4. Mineral storage bones are made up of minerals, especially calcium phosphate 5. Blood cell frmtn red marrow contains blood cells Bone is classified by How the tissue is organized Compact Bone This forms the outer surface of bone. Dense AKA: cortical bone Spongy Bone Network of interwoven spicules called trabeculae Lots of space Made of same stuff as compact bone, arranged differently
Bone shape (4 general shapes) Long Bones Most appendicular bones are long bones Femur, metacarpals, etc Flat Bones Short Bones Thin & flat, broad, curved Cranial bones, sternum, ribs, scapula Cuboidal, box-like Carpal & tarsal bones Includes sesamoid bones, which are bones that form within a tendon (where stress is on a tendon). These vary! Complex shape Vertebrae, os coax, maxilla, ethmoid, etc
Irregular Bones
Bone Structure LONG BONES form into a bone with distinct regionsthe DIAPHYSIS, EPIPHYSIS, METAPHYSIS and MEDULLARY CAVITY. The diaphysis is the shaft of the long bone, while the epiphyses are the rounded ends. The metaphysis is the area where the diaphysis and epiphyses meet. This region surrounds the epiphyseal plate, which is on the inside. The medullary cavity, located on the inside of the bone, runs at least along the
length of the diaphysis, but it can also go up into the epiphysis. It is lined by spongy bone and is hollow space. MEMBRANES surround every bone. The membrane is a double layer called the PERIOSTEUM, while the ENDOSTEUM lines the trabeculae of internal spongy bone. The periosteum is made up of two layersthe outer layer is made up of DICT so that tendons and ligaments can insert. The inner layer is made up of osteoblasts and osteoclasts. How does the periosteum bind to the bone? It uses perforating fibers! The periosteum is richly supplied with nerve fibers, blood vessels and lymphatic vessels. The ENDOSTEUM is not as dense as the periosteum and is made up of areolar CT. It also contains osteoblasts and osteoclasts. Structure of compact bone (pg 183) Compact bone is made up of OSTEONS, the functional unit of compact bone. Osteons are cylinders of bone tissue that run parallel to the long axis of a long bone. Each osteon surrounds a central canal (elevator shaft) that transmits blood vessels and nerve that serve the needs of the osteons cells. While the central canals go up and down, the perforating canals run perpendicular to the long axis, connecting the blood and nerve supply of the PERIOSTEUM to the central canal. Think of Willie Wonkas elevator system that would go up and down and sideways. These canals, like all other internal bone cavities, are lined with endosteum. The osteon up close! Each osteon is made up of concentric layers of matrix called lamellae. Think of a telescope! Running through this matrix are collagen fibersthe alternating direction of the collagen fibers in each layer of lamellae give the osteon greater strength! Osteocytes occupy spaces called lacunae (lac=hollow, una=little) at the junctions of the lamellae. Hairlike canals called canaliculi connect the lacunae to each other and to the central canal. This is how they get their nutrients. (page 183) What is an osteocyte? Mature bone cell Resides in the lacunae (lacuna, singular) The lacunae are between the lamellae
What about other lammalae? Osteons cant fill the whole space because they are round. Think of apples in a boxthere is lots of space around the apples! Something has to fill this space around the osteonswhat is it? Two types of lamellaecircumferential and interstitial. CIRCUMFERENTIAL LAMALLAE is deep to the periosteum and superficial to the medullary cavity. Circumferential lamellae look like the rings of a tree and surround the group of osteons on the circumference of the diaphysis.
INTERSTITIAL LAMALLAE lie between the osteons. Essentially interstitial lamellae are incomplete osteons (old ones). RED MARROW contains hematopoetic tissue and is the site of blood cell production. The locations vary based on developmental stage. In infants, who need a greater level of blood cell production, the red marrow is in the medullary cavities of all long bones and in all areas of spongy bones. In adults the red marrow is located in the proximal heads of the humerus and femur and in the diploe of flat bones (the skull, os coxa and sternum). Diploe is the spongy bone of flat bone. So, what fills the remaining areas of the long bones? Yellow marrow (lipid), fills the space and it may revert to red marrow if needed due to blood loss. The Matrix The bone has both organic and inorganic components. The ORGANIC COMPONENT of the matrix is the OSTEOD. It comprises 1/3 of the matrix and is composed of ground substance and fibers. ground substance made up of proteoglycans and glycoproteins fibers collagen, which are secreted by osteoblasts value of osteod provides flexibility and tensile strength resists collage resists stretching The INORGANIC COMPONENT of the matrix are the mineral salts, which make up 2/3 of the matrix by mass. made up of primarily calcium phosphates which is tiny salt crystals packed tightly arnd collagen fibers value of mineral salts provides hardness of bone resists compression Bone Physiology Bone formation begins around the 8th week of development. At this stage, the skeletal elements are fibrous membranes and hyaline cartilage. There are two different methods of ossification, one for each type. The fibrous membrane will become bone via INTRAMENBRANEOUS OSSIFICATION, while the hyaline cartilage will become bone via ENDOCHONDRYL OSSIFICATION. With intramembraneous ossification, bone forms within the fibrous membrane. This is generally for skull bones and clavicles. With endochondryl ossification, bone forms from the cartilaginous model. This occurs in long bones, short bones, irregular bones)
Intramembraneous ossification (page 184) 1. Ossification center appears in the fibrous connective tissue membrane. It is formed when mesenchymal cells cluster near the center of the membrane and differentiate into osteoblasts. 2. Bone matrix (osteoid) is secreted within the fibrous membrane. In this stage, osteod gets laid down by the osteoblasts, which mineralizes within a few days. Trapped osteoblasts become osteocytes. 3. Vascularizationwoven bone and periosteum form in this stage. Blood vessels grow into the region and the matrix forms around the blood vessels, forming woven bone. The osteoid gets laid down in a random network of trabeculaethis is not the same as spongy bone. The periosteum forms as the vascularized mesenchyme condense on the external membrane faces. Not bone yet! 4. Remodeling..bony collar of compact bone forms and red marrow appears in this stage. The bony collar forms as the trebeculae deep to the periosteum thicken and merge. This is later replaced by mature lamellar compact bone. The spongy bone (diploe) forms when woven bone is replaced by mature trabeculaeits vascular tissue becomes red marrow. Endochondryl ossification (cartilage model) This process is more complex because the hyaline cartilage model must be broken down as ossification proceeds. It begins in the 2nd month of development and has 6 steps. 1. Periosteum formation. Blood vessels invade the perichondrium of the cartilage model and convert to periosteum. The inner mesenchymal cells become osteoblasts. 2. Bony collar formation. A bony collar forms around the diaphysis of the hyaline cartilage model. It is formed when osteoblasts in the periosteum lay down osteod along the diaphysis of the model. 3. Cartilage cavitation overlaps bony collar formation. In this stage, the primary ossification center forms at the center of the diaphysis. Chondrocytes grow larger (hypertrophy), and as they grow larger they start calcifying the cartilage around them. As they grow they require more nutrients which they do not get due to calcificationso they die, leaving behind cavities. However, the bony collar keeps the hyaline cartilage stable. 4. Periosteal bud invades the internal cavities and spongy bone forms. The periosteal bud is made up of arties, veins, lymphatics, red marrow elements, osteoblasts, osteoclasts and nerves. The entering osteoclasts partially erode the calcified cartilage matrix and the osteoblasts secrete osteoid around the remaining cartilage forming the earliest version of spongy bone. 5. The diaphysis elongates and a medullary cavity forms. In this stage osteoclasts erode the newly-formed spongy bone, forming a medullary cavity. The diaphysis continues to lengthen and cartilage cells in the epiphysis continue to grow. In this stage ossification chases cartilage formation along the length of the shaft. 6. Epiphyseal ossification occurs around birth. At this point the epiphysis start forming secondary ossification centers in the same way as the diaphysis, with two exceptions: no medullary cavity forms so the spongy bone is retained, and there is
no bony collar formation. The hyaline cartilage remains on the articular surface of the long bones (ends of long bones) and at the epiphyseal plate, which is temporary. Bone Growth (lengthening of bone) page 186-187. Bone growth occurs until the late teens/early 20s. It occurs at the epiphyseal plate. Bone growth takes place because cartilage on the epiphyseal plate continues to grow, pushing the epiphyses away from the diaphysis. The older chondrocytes hypertrophy and their lacunae erode and enlarge. Subsequently the surrounding cartilage matrix calicifies. Osteoclasts and osteoblasts convert cartilage to bone. Osteoclasts remove bone at diaphysis side extending the medullary cavity. Cartilage formation and replacement continue at the same rate and growth continues to occur. At the end of the growth, chondrocyte division slows and bone formation catches up. The epiphyseal plate closes. Bone Growth (widening of bone) The widening of bone does not involve cartilage. It is used to increase the diameter of bone, producing a thicker, stronger bone that is not too heavy. The osteoblasts in perosteum lay down a layer of bone on the external surface while the osteoclasts in endosteum remove bone from the internal surface. The result is the medullary cavity gets wider and the diameter increases. The thickness of the bone wall increases, due to the laying down activity of the osteoblasts outpacing that of the osteoclasts. Bone Growth Regulation Bone growth is regulated primarily by hormones. In childhood, growth is stimulated by the pituitary GROWTH HORMONE, while the THYROID GLAND modulates the effect of the growth hormone. Later, at the time of a growth spurt or at the end of it when the epiphyseal plate closes, SEX HORMONES regulate growth (estrogen and testosterone). Bone Remodeling For bone remodeling to occur, bone deposit and resorption occur at the same rate. What controls bone remodeling? HORMONAL MECHANISM maintains calcium homeostasis in the blood; and RESPONSE TO MECHANICAL STRESS keeps bones strong where stresses are acting (Wolffs Law). Some facts about bone remodeling: o Occurs throughout life o Constantly changing, the skeleton is replaced frequently o Spongy bone replaced every 3-4 years o Compact bone replaced every 10 years o Influencing factors o Mineral needs of the body o Stresses on bone Wolffs Law stipulates that a bone grows or remodels in response to the demands placed on it.
o Mechanisms o Hormonal (relates to mineral needs). PARATHYROID HORMONE (from the parathyroid gland) stimulates bone resportion by stimulating osteoclast activity. Calcium is released into the blood in response to low calcium levels. CALCITONIN (from the thyroid gland) stimulates bone deposition by stimulating osteoblast and inhibiting osteoclasts. Calcitonin activates in response to high blood calcium levels. It has a limited effect on adults. o Mechanical (relates to stresses). Bone is laid down in regions where forces are the greatest walls of shafts of long bones center of shaft more than the ends trabeculae form along lines of stress bony projections occur at muscle attachment
Potrebbero piacerti anche
- Anatomy and Physiology Musculoskeletal System Chap 6 - 2401Documento18 pagineAnatomy and Physiology Musculoskeletal System Chap 6 - 2401slyfoxkittyNessuna valutazione finora
- Chapter 14Documento15 pagineChapter 14missy23papNessuna valutazione finora
- Rounding Rules Bro WardDocumento1 paginaRounding Rules Bro Wardmissy23pap0% (1)
- ALVEOLAR BoneDocumento72 pagineALVEOLAR BoneArchana50% (2)
- The Skeletal SystemDocumento5 pagineThe Skeletal SystemCharlie CharlesNessuna valutazione finora
- CHAPTER 6 - Skeletal SystemDocumento4 pagineCHAPTER 6 - Skeletal SystemArlen Joy V. AMPARONessuna valutazione finora
- Skeletal System More On ProcessDocumento4 pagineSkeletal System More On Processsayie potatoNessuna valutazione finora
- BONEDocumento48 pagineBONEnivethaseshaNessuna valutazione finora
- Skeletal - System AnatomyDocumento89 pagineSkeletal - System AnatomysanayaNessuna valutazione finora
- Introduction To Skeletal 1Documento196 pagineIntroduction To Skeletal 1Earl TrinidadNessuna valutazione finora
- Chapter 6 Bone Tissue 2304Documento37 pagineChapter 6 Bone Tissue 2304Sav Oli100% (1)
- Skeletal SystemDocumento3 pagineSkeletal SystemCristina AdolfoNessuna valutazione finora
- Musculoskeletal Anatomy and Physiology 4Documento67 pagineMusculoskeletal Anatomy and Physiology 4Dennis Nabor Muñoz, RN,RM100% (1)
- Osteomalacia, Bones Are Mineral-Deficient and Easily DeformedDocumento16 pagineOsteomalacia, Bones Are Mineral-Deficient and Easily DeformedVarel JoanNessuna valutazione finora
- Reading Material Skeletal SystemDocumento32 pagineReading Material Skeletal SystemShamel CurrayNessuna valutazione finora
- (W9) The Skeletal SystemDocumento9 pagine(W9) The Skeletal SystemReign Heart HayahayNessuna valutazione finora
- BC (H) - IV-Human Physiology-Bone Structure and Formation-2 & 3Documento32 pagineBC (H) - IV-Human Physiology-Bone Structure and Formation-2 & 3Starco ForeverNessuna valutazione finora
- Chapter 6 Content Review Questions 1-8Documento3 pagineChapter 6 Content Review Questions 1-8Rhonique MorganNessuna valutazione finora
- Intoduction To The Skeletal SystemDocumento23 pagineIntoduction To The Skeletal SystemDenise AngelNessuna valutazione finora
- Reviewer Zoo LecDocumento27 pagineReviewer Zoo LecayeyedumpNessuna valutazione finora
- Anaphy AnalysisDocumento6 pagineAnaphy AnalysisLuna ScorpiusNessuna valutazione finora
- Skeletal SystemDocumento5 pagineSkeletal SystemArra BeatrizNessuna valutazione finora
- The Skeletal SystemDocumento52 pagineThe Skeletal SystemrizzamaearancesNessuna valutazione finora
- Relationship To Other Organ SystemsDocumento11 pagineRelationship To Other Organ SystemsVern NuquiNessuna valutazione finora
- Skeletal SystemDocumento27 pagineSkeletal SystemAlliyah SalindoNessuna valutazione finora
- SKELETAL SYSTEM ReviewerDocumento7 pagineSKELETAL SYSTEM ReviewerKrize Colene dela CruzNessuna valutazione finora
- O Is Composed of Bones, Cartilage, and Ligaments o CartilageDocumento13 pagineO Is Composed of Bones, Cartilage, and Ligaments o CartilageVarel JoanNessuna valutazione finora
- Functions of The Skeletal System TopicDocumento21 pagineFunctions of The Skeletal System TopicTUNGCALING ACNessuna valutazione finora
- Unit 2-4 Anatomy and Human Physiology NotesDocumento90 pagineUnit 2-4 Anatomy and Human Physiology NotesAbi .JNessuna valutazione finora
- Skeletal SystemDocumento200 pagineSkeletal SystemJB AriasdcNessuna valutazione finora
- THE SKELETAL SYSTEM I - Bone TissueDocumento2 pagineTHE SKELETAL SYSTEM I - Bone TissueAmirah AnfNessuna valutazione finora
- m5 Skeletal SystemDocumento33 paginem5 Skeletal Systemapi-464344582Nessuna valutazione finora
- Unit Three: General Anatomy of The of Skeletal System (Osteology)Documento78 pagineUnit Three: General Anatomy of The of Skeletal System (Osteology)Gifti DemisseNessuna valutazione finora
- Bone Physiology: Structure and FunctionsDocumento75 pagineBone Physiology: Structure and FunctionsAnalhaq ShaikhNessuna valutazione finora
- Bone TissueDocumento66 pagineBone TissueFunikawati Baldiyah100% (1)
- Anaphy Exercise 5 - SKELETAL AND ARTICULAR SYSTEMDocumento12 pagineAnaphy Exercise 5 - SKELETAL AND ARTICULAR SYSTEMKenzoNessuna valutazione finora
- HANDOUTS Prelim CH 6Documento40 pagineHANDOUTS Prelim CH 6Abia Annieson A. LorenzoNessuna valutazione finora
- Chapter 6 Cartilage and BoneDocumento5 pagineChapter 6 Cartilage and BoneSuperjunior8Nessuna valutazione finora
- Bone Connective Tissue Structure (40Documento53 pagineBone Connective Tissue Structure (40galaxyduck100% (1)
- The Skeletal SystemDocumento7 pagineThe Skeletal Systemnichole2anne2rodriguNessuna valutazione finora
- Bone MetastasisDocumento8 pagineBone MetastasisRonak PatelNessuna valutazione finora
- Skeletal SystemDocumento15 pagineSkeletal SystemRaven LacsonNessuna valutazione finora
- The Skeletal System: Comia, Joshua Cyryll Habacon, Gabrielle AnneDocumento56 pagineThe Skeletal System: Comia, Joshua Cyryll Habacon, Gabrielle Annegian habaconNessuna valutazione finora
- Intramembranous and endochondral ossification processesDocumento8 pagineIntramembranous and endochondral ossification processesMuhammad SaifullohNessuna valutazione finora
- The Skeletal SystemDocumento19 pagineThe Skeletal SystemMatthew YoungNessuna valutazione finora
- Topic 6 Skeletal SystemDocumento8 pagineTopic 6 Skeletal SystemMary Ann Morillo TenederoNessuna valutazione finora
- Anatomy and PhysiologyDocumento63 pagineAnatomy and Physiologykathleen.cuyaNessuna valutazione finora
- Module-5-The Skeletal SystemDocumento13 pagineModule-5-The Skeletal SystemMARIA CORAZON CONTANTENessuna valutazione finora
- Bone Structure and ClassificationDocumento5 pagineBone Structure and ClassificationEmmalyn PeridaNessuna valutazione finora
- Bone As A Living Dynamic TissueDocumento14 pagineBone As A Living Dynamic TissueSuraj_Subedi100% (6)
- Ch. 6 - Osseous Tissue Bone StructureDocumento54 pagineCh. 6 - Osseous Tissue Bone StructureHilary OliverioNessuna valutazione finora
- Muscloskeletal SystemDocumento154 pagineMuscloskeletal SystemAbera AberaNessuna valutazione finora
- Histology of BoneDocumento20 pagineHistology of Boneyudha anantha khaerul putraNessuna valutazione finora
- Anaphys SKELETAL SYSTEMDocumento39 pagineAnaphys SKELETAL SYSTEMBEATRICE MAE MAGDALESNessuna valutazione finora
- The Skeletal System HDocumento23 pagineThe Skeletal System HRajorshi MishraNessuna valutazione finora
- Skeletal System Anatomy and PhysiologyDocumento29 pagineSkeletal System Anatomy and PhysiologyKBD100% (1)
- 1.2 Cartilage and BoneDocumento27 pagine1.2 Cartilage and BonePema GaleyNessuna valutazione finora
- Skeletal System: CartilageDocumento20 pagineSkeletal System: CartilageGrace PascualNessuna valutazione finora
- Skeletal System Functions and Bone ClassificationDocumento7 pagineSkeletal System Functions and Bone ClassificationKathleenJoyGalAlmasinNessuna valutazione finora
- Skeletal SystemDocumento104 pagineSkeletal Systemsyafi zulNessuna valutazione finora
- Advanced farriery knowledge: A study guide and AWCF theory course companionDa EverandAdvanced farriery knowledge: A study guide and AWCF theory course companionNessuna valutazione finora
- Chapter 17Documento11 pagineChapter 17missy23papNessuna valutazione finora
- 3m Accessory KitDocumento2 pagine3m Accessory KitByron DubowNessuna valutazione finora
- Chapter 18Documento11 pagineChapter 18missy23pap100% (1)
- Chapter 16Documento10 pagineChapter 16missy23pap50% (2)
- Black & Hawks: Medical-Surgical Nursing, 8 Edition: Test Bank Chapter 18: Clients With Wounds Multiple ChoiceDocumento11 pagineBlack & Hawks: Medical-Surgical Nursing, 8 Edition: Test Bank Chapter 18: Clients With Wounds Multiple Choicemissy23papNessuna valutazione finora
- Nclex Question ExamplesDocumento4 pagineNclex Question Examplesmissy23pap100% (1)
- Chapter 19Documento16 pagineChapter 19missy23pap100% (1)
- Chapter 2Documento6 pagineChapter 2missy23papNessuna valutazione finora
- Osborn Ch04 Tif Step6 RevDocumento34 pagineOsborn Ch04 Tif Step6 Revmissy23papNessuna valutazione finora
- Chapter - 10 & 12Documento5 pagineChapter - 10 & 12missy23papNessuna valutazione finora
- Chap 1Documento18 pagineChap 1missy23papNessuna valutazione finora
- Drug Calculations: Making It EasyDocumento26 pagineDrug Calculations: Making It EasyShaells JoshiNessuna valutazione finora
- Applied Technology: Level 6Documento112 pagineApplied Technology: Level 6missy23papNessuna valutazione finora
- ©2011 by Pearson Education, Inc. Adams/Holland, Test Bank For Pharmacology For Nurses, 3eDocumento7 pagine©2011 by Pearson Education, Inc. Adams/Holland, Test Bank For Pharmacology For Nurses, 3emissy23papNessuna valutazione finora
- Chapter 4Documento25 pagineChapter 4missy23pap100% (1)
- ch45 NCP Sleep 1180-1181Documento2 paginech45 NCP Sleep 1180-1181missy23papNessuna valutazione finora
- Chapter 16Documento4 pagineChapter 16missy23papNessuna valutazione finora
- PegDocumento13 paginePegmissy23papNessuna valutazione finora
- Potter & Perry: Fundamentals of Nursing, 7 EditionDocumento11 paginePotter & Perry: Fundamentals of Nursing, 7 Editionmissy23pap100% (1)
- Emergency DrugsDocumento17 pagineEmergency Drugsapi-3853350100% (12)