Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Chronic Cough Due To Chronic Bronchitis - AACP Guideline
Caricato da
Afian PrasetyoDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Chronic Cough Due To Chronic Bronchitis - AACP Guideline
Caricato da
Afian PrasetyoCopyright:
Formati disponibili
Chronic Cough Due to Chronic Bronchitis
ACCP Evidence-Based Clinical Practice Guidelines
1. Adults who have a history of chronic cough and sputum expectoration occurring on most days for at least 3 months and for at least 2 consecutive years should be given a diagnosis of chronic bronchitis when other respiratory or cardiac causes of chronic productive cough are ruled out. Level of evidence, low; net benefit, substantial; grade of recommendation, B 2. The evaluation of patients with chronic cough should include a complete history regarding exposures to respiratory irritants including cigarette, cigar, and pipe smoke; passive smoke exposures; and hazardous environments in the home and workplace. All are predisposing factors of chronic bronchitis. Level of evidence, low; net benefit, substantial; grade of recommendation, B 3. Smoke-free workplace and public place laws should be enacted in all communities. Level of evidence, expert opinion; net benefit, substantial; grade of recommendation, E/A 4. Stable patients with chronic bronchitis who have a sudden deterioration of symptoms with increased cough, sputum production, sputum purulence, and/or shortness of breath, which are often preceded by symptoms of an upper respiratory tract infection, should be considered to have an acute exacerbation of chronic bronchitis, as long as conditions other than acute tracheobronchitis are ruled out or are considered unlikely. Level of evidence, expert opinion; net benefit, substantial; grade of recommendation, E/A 5. In patients with chronic cough who have chronic exposure to respiratory irritants, such as personal tobacco use, passive smoke exposure, and workplace hazards, avoidance should always be recommended. It is the most effective means to improve or eliminate the cough of chronic bronchitis. Ninety percent of patients will have resolution of their cough after smoking cessation. Level of evidence, good; net benefit, substantial; grade of recommendation, A 6. In stable patients with chronic bronchitis, there is no role for long-term prophylactic therapy with antibiotics. Level of evidence, low; benefit, none; grade of recommendation, I 7. In patients with acute exacerbations of chronic bronchitis, the use of antibiotics is recommended; patients with severe exacerbations and those with more severe airflow obstruction at baseline are the most likely to benefit. Level of evidence, fair; net benefit, substantial; grade of recommendation, A 8. In stable patients with chronic bronchitis, the clinical benefits of postural drainage and chest percussion have not been proven, and they are not recommended. Level of evidence, fair; net benefit, conflicting; grade of recommendation, I 9. In patients with an acute exacerbation of chronic bronchitis, the clinical benefits of postural drainage and chest percussion have not been proven, and they are not recommended. Level of evidence, fair; net benefit, conflicting; grade of recommendation, I 10. a. In stable patients with chronic bronchitis, therapy with short-acting Beta agonists should be used to control bronchospasm and relieve dyspnea; in some patients, it may also reduce chronic cough. Level of evidence, good; net benefit, substantial; grade of recommendation, A b. In stable patients with chronic bronchitis, therapy with ipratropium bromide should be offered to improve cough. Level of evidence, fair; net benefit, substantial; grade of recommendation, A c. In stable patients with chronic bronchitis, treatment with theophylline should be considered to control chronic cough; careful monitoring for complications is necessary. Level of evidence, fair; net benefit, substantial; grade of recommendation, A 11. For patients with an acute exacerbation of chronic bronchitis, therapy with short-acting Beta agonists or anticholinergic bronchodilators should be administered during the acute exacerbation. If the patient does not show a prompt response, the other agent should be added after the first is administered at the maximal dose. Level of evidence, good; net benefit, substantial; grade of recommendation, A 12. For patients with an acute exacerbation of chronic bronchitis, theophylline should not be used for treatment. Level of evidence, good; net benefit, none; grade of recommendation, D 13. For stable patients with chronic bronchitis, there is no evidence that the currently available expectorants are effective and therefore they should not be used. Level of evidence, low; net benefit, none; grade of recommendation, I
14. In stable patients with chronic bronchitis, treatment with a long-acting Beta agonist when coupled with an inhaled corticosteroid should be offered to control chronic cough. Level of evidence, good; net benefit, substantial; grade of recommendation, A 15. For stable patients with chronic bronchitis and an FEV1 of < 50% predicted or for those patients with frequent exacerbations of chronic bronchitis, inhaled corticosteroid therapy should be offered. Level of evidence, good; net benefit, substantial; grade of recommendation, A 16. For stable patients with chronic bronchitis, long-term maintenance therapy with oral corticosteroids such as prednisone should not be used; there is no evidence that it improves cough and sputum production, and the risks of serious side effects are high. Level of evidence, expert opinion; net benefit, negative; grade of recommendation, E/D 17. For patients with an acute exacerbation of chronic bronchitis, there is no evidence that the currently available expectorants are effective, and therefore they should not be used. Level of evidence, low; net benefit, none; grade of recommendation, I 18. For patients with an acute exacerbation of chronic bronchitis, a short course (10 to 15 days) of systemic corticosteroid therapy should be given; IV therapy in hospitalized patients and oral therapy for ambulatory patients have both proven to be effective. Level of evidence, good; net benefit, substantial; grade of recommendation, A 19. In patients with chronic bronchitis, central cough suppressants such as codeine and dextromethorphan are recommended for short-term symptomatic relief of coughing. Level of evidence, fair; benefit, intermediate; grade of evidence, B
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- DexmedetomidineDocumento11 pagineDexmedetomidineAfian PrasetyoNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- List LaguDocumento3 pagineList LaguAfian PrasetyoNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Film Serial BaratDocumento31 pagineFilm Serial BaratAfian PrasetyoNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- Anestesia - Handbook of Regional Anesthesia - ESRA 2007Documento130 pagineAnestesia - Handbook of Regional Anesthesia - ESRA 2007Irene Cristina100% (3)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Film HDDocumento7 pagineFilm HDAfian PrasetyoNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Nobel Winners in MedicineDocumento10 pagineNobel Winners in MedicineAfian PrasetyoNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- 1 Mom 3 Dads and 90+ Other Popular K-DramasDocumento13 pagine1 Mom 3 Dads and 90+ Other Popular K-DramasAfian PrasetyoNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Belajar GitarDocumento6 pagineBelajar GitarAfian PrasetyoNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Nobel Winners in MedicineDocumento10 pagineNobel Winners in MedicineAfian PrasetyoNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- Circadian Rhythm - SleepafsDocumento4 pagineCircadian Rhythm - SleepafsAfian PrasetyoNessuna valutazione finora
- DM Dan CVD AfianDocumento22 pagineDM Dan CVD AfianAfian PrasetyoNessuna valutazione finora
- Defense MechanismDocumento3 pagineDefense MechanismAfian PrasetyoNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Chronic Cough Due To Chronic Bronchitis - AACP GuidelineDocumento2 pagineChronic Cough Due To Chronic Bronchitis - AACP GuidelineAfian PrasetyoNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Ejsr 72 3 04Documento9 pagineEjsr 72 3 04Khalifa BakkarNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Crystalloid and Colloid TherapyDocumento11 pagineCrystalloid and Colloid TherapyAlexa UGNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Nursing Grand Rounds Reviewer PDFDocumento17 pagineNursing Grand Rounds Reviewer PDFAlyssa Jade GolezNessuna valutazione finora
- Addiction CaseDocumento4 pagineAddiction CasePooja VarmaNessuna valutazione finora
- Dr. Noel Casumpang vs. Cortejo G.R. No. 171127, March 11, 2015Documento29 pagineDr. Noel Casumpang vs. Cortejo G.R. No. 171127, March 11, 2015FD BalitaNessuna valutazione finora
- AMRI Hospital TariffDocumento42 pagineAMRI Hospital TariffsandeepNessuna valutazione finora
- TTTTDocumento26 pagineTTTTMoataz TrabehNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Cpe Common Diagnoses 6-4-2021Documento9 pagineCpe Common Diagnoses 6-4-2021Shubham HarishNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Gen EpidemiologyDocumento88 pagineGen EpidemiologyShibu Sebastian100% (1)
- Power of The Pinch Pinch Lower Lid BlepharoplastyDocumento6 paginePower of The Pinch Pinch Lower Lid BlepharoplastyBFF BotoxNessuna valutazione finora
- Diagnosis and Treatment of Limb Fractures Associated With Acute Peripheral IschemiaDocumento6 pagineDiagnosis and Treatment of Limb Fractures Associated With Acute Peripheral IschemiaramadhaniandaNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- SRG Test BiologyDocumento156 pagineSRG Test Biologypranayallen2006Nessuna valutazione finora
- Human Sexuality and Sexual DisordersDocumento42 pagineHuman Sexuality and Sexual DisordersAbdul Gafoor FahmyNessuna valutazione finora
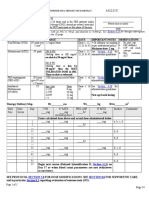
- EHAQ 4th Cycle Audit Tool Final Feb.10-2022Documento51 pagineEHAQ 4th Cycle Audit Tool Final Feb.10-2022Michael Gebreamlak100% (1)
- Opsonin Pharma ListDocumento14 pagineOpsonin Pharma ListDelegate Tech100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Nephrotic Syndrome and Hypertension Nahla I. A L. Gabban Essam Ahmed Abdullah Haider Nadhim Abd FicmsDocumento6 pagineNephrotic Syndrome and Hypertension Nahla I. A L. Gabban Essam Ahmed Abdullah Haider Nadhim Abd FicmsMarcelita DuwiriNessuna valutazione finora
- Cardiovascular Pathology: Risks, Heart Failure, AMIDocumento5 pagineCardiovascular Pathology: Risks, Heart Failure, AMIbmhsh100% (2)
- Becozyme AmpDocumento1 paginaBecozyme AmpMohammed IbrahimNessuna valutazione finora
- Cinnarizine A Contemporary ReviewDocumento9 pagineCinnarizine A Contemporary ReviewprimaNessuna valutazione finora
- TMG Versus DMGDocumento3 pagineTMG Versus DMGKevin-QNessuna valutazione finora
- Frequency, Severity, and Distress of Dialysis-Related Symptoms Reported by Patients On HemodialysisDocumento1 paginaFrequency, Severity, and Distress of Dialysis-Related Symptoms Reported by Patients On HemodialysisHelvia RahayuNessuna valutazione finora
- Power Point Dr. ShintaDocumento11 paginePower Point Dr. ShintaAnonymous fOz6ToNessuna valutazione finora
- Institute nephro-urology rate listDocumento9 pagineInstitute nephro-urology rate listVertika VermaNessuna valutazione finora
- High Risk B-Precursor Acute Lymphoblastic Leukemia Interim Maintenance IIDocumento1 paginaHigh Risk B-Precursor Acute Lymphoblastic Leukemia Interim Maintenance IIRitush MadanNessuna valutazione finora
- SepanskiDocumento13 pagineSepanskiTammy Utami DewiNessuna valutazione finora
- 12Documento1 pagina12SuryaAtmajayaNessuna valutazione finora
- Quiz Hospital DocumentationDocumento5 pagineQuiz Hospital DocumentationJessica EdiosNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Pathoma Female Genital TractDocumento7 paginePathoma Female Genital TractVinNessuna valutazione finora
- AEBA QUESTIONS-WPS OfficeDocumento2 pagineAEBA QUESTIONS-WPS OfficeMarj Castor LisondraNessuna valutazione finora
- 2007 MCQDocumento67 pagine2007 MCQTiffani Gutierrez100% (1)