Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Irrational Use of Drug
Caricato da
sreedamDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Irrational Use of Drug
Caricato da
sreedamCopyright:
Formati disponibili
Irrational Use of Drug
Introduction:
Ineffective inappropriate and economically nonviable use of medicines is often observed in health care throughout the world. This is more often in the developing countries. The need for achieving quality use of medicines in the healthcare system is not only because of the financial reasons with which policy makers and administrators are usually most concerned. Appropriate use of drugs is also one essential element in achieving quality of health and medical care for patients and the community as a whole. WHO defined rational use of drug as Rational use of drugs requires that patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements for an adequate period of time, and the lowest cost to them and their community. (WHO, 1985) The definition implies that rational use of drugs, especially rational prescribing should meet following criterias: Appropriate indication: the decision to prescribe drug(s) is entirely based on medical rationale and that drug therapy is an effective and safe treatment. Appropriate drug: the selection of drugs is based on efficacy, safety, suitability and cost considerations. Appropriate patient: no contraindications exist and the likelihood of adverse reactions is minimal, and the drug is acceptable to the patient. Appropriate information: Patients should be provided with relevant, accurate, important and clear information regarding his or her condition and the medications that are prescribed. Appropriate monitoring: the anticipated and medications should be appropriately monitored. unexpected effects of
Factors Underlying Irrational Use of Drugs
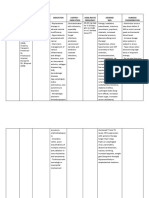
There are many different factors which affect the irrational use of drugs. In addition, different cultures view drugs in different ways, and this can affect the way drugs are used. in India this can therefore be a complex with multiple cultures , religions, dialects and castes. If one were to broadly classify the factors, they could be divided in to: those deriving from patients, chemists shop, prescribers, the workplace the supply system, industry influences, regulation, drug information and misinformation.
In each group, there can be various ways contributing to irrational use of drugs: v Patients: drug expectations. misinformation, misleading beliefs, patient demands /
v Prescribers: lack of education and training, inappropriate role models, patient pressures, lack of objective drug information, company incentives, limited experience, misleading beliefs about drug efficacy, competition. v Workplace: heavy patient load, pressure to prescribe, lack of adequate lab capacity, insufficient staffing. v Drug Supply System: unreliable suppliers drug shortages, limited budgets necessitating fixed choices, expired drug supplied. v Chemists Shops: patient pressures, profit motives, competition. v Drug Regulation: non essential drugs available, inefficient audit system, inadequate legal implementation, and no-formal procedures. v Industry: promotional activities, misleading claims, incentives. Impact of Irrational drug Use Irrational drug use can have various consequences, for the patient, the public, the health system and even the economy. A few important consequences are mentioned below: v Reduction in the quality f drug therapy- this can lead to increased morbidity and mortality. vWaste of resources- This can lead to reduced availability of other vital drugs and increased costs. v Increased risk of unwanted effect- adverse drug reactions and the emergence of drug resistance. v Psychosocial impacts-patients may believe that there is a pill for every ill A focused case of irrational drug use and its consequence- the antimicrobial misuse problem: The problem of antimicrobial resistance was one of the important issues brought up at the world health assembly (WHA) in 2005. The WHO says that antimicrobial resistance is one of the worlds most serious public health problems. A major reason is the irrational use of medicines According to WHO, worldwide, more than 50% of all medicines are prescribed, dispensed or sold inappropriately and 50% of patients fail to take them correctly. The consequence of this is seen directly with the misuse of antibiotics.
There is increasing antimicrobial resistance, with resistance of up to 70-90 % to original first line antibiotics for dysentery (shigella), pneumonia (Pneumococcal), gonorrhea, and hospital infections (Staph. Aureus). A WHO policy paper on Containing antimicrobial resistance says that many of the microbes that cause infectious disease no longer respond to common antimicrobial drugs such as antibiotics, antiviral and antiprotozoal drugs. The problem has reached unprecedented proportions that unless concerted action is taken worldwide; we run the risk of returning to the preantibiotic era when many more children than now died of infectious diseases and major surgery was impossible due to the risk of infection. Fourteenth WHO model list of essential medicines (March 2005) contains only 18 approved drug combinations, whereas in India, there are innumerable examples of irrational drug combinations, which are available and can be bought without necessarily giving a prescription. Some irrational fixed dose combinations available in the Indian Market Sr. Combinations No. 1 Irrationality
Norfloxacin+ Metronidazole;Though claimed to be broad spectrum, Norfloxacin+Tindazole; combining (antiameobic) with fluroquinolone Norfloxacin+tindazole+Lopera (antibacterial) is irrational because patient mide; suffers only from one type of diarrhea. Using Norfloxacin+Tinidazole+Dicycl this combination adds to cost, adverse effects oamine; ad may encourage resistance. Norfloxacin+Ornidazole; Ciprofloxacin+Tinidazole; ofloxacin+Tinidazole; Ofloxacin+Metronidazole; Ofloxacin+Ornidazole; Gatifolxacin+Ornidazole.
Nimesulide+Diclofenac; Nimesulide is a controversial drug, has been Nimesulide+Dicycloamine+Si banned in many countries. It is a sorry state methicone; Nimesulide +of affairs that its combinations are readily Paracetamol; Nimesulide+available over the counter. Combining two Cetrizine + Pseudophedrine;NSAIDs may increase the side effects of both Nimesulide + Paracetamol+the NSAIDs. There is little documentary, Tizanidine. evidence that a preparation containing more than one analgesic is more effective than a single ingredient preparation.
Amoxycillin+ Cloxacillin.
Amoxycillin is inactive against staphylococcus as most strains produce lactamase and cloxacillin is not so active against streptococci. For any given, infection, one of the components is useless but adds to cost and adverse effect. Since amount of each drug is halved, efficacy is reduced and chances of selecting strains are increased.
Domperidine+ Domperidone Esomeprazole.
Rabeprazole;Increased incidence of rhabdomyolysis +
Simvastatin + Nicotinic acid;Probability of myopathy is increased Atrovastatin + Nicotinic acid Enalpril+ Losartan. Combining two drugs affecting the same pathway is irrational ; it doesnt add to efficacy aluminumAntacids raise the gastric pH and reduce the +aluminumabsorption of benzodiazepines
Diazepam+Dried hydroxide gel
glycinate + oxyphenonium; Diazepam+ Magaldrate + Oxyphenonium; Diazepam+ Dried alumininum hydroxide gel + magnesium trisilicate+ Dimethylpolysiloxane. 8 Cetrizine +Phenylpropanolamine is banned drug; yet its Phenylpropanolamine +a part of many cold remedies. Besides its Dextromethorpan; Cetrizine +potential to cause stroke (more so in Phenylpropanolamine hypertensive) , it can aggravate diabetes , +Paracetamol; Levocetrizine+glaucoma and prostate enlargement . Paracetamol+ Phenylpropanolamine. Cisapride+ Omeprazole;In patients with gastro esophageal reflux Mosapride+ Pantoprazole disease, the use of this combination has shown no benefit due to addition of prokinetic agents.
What needs to be done
Today, rational use of drug/ pharmaceutical is an issue of the at most importance. The growing concern is not only for promotion of appropriate use of pharmaceuticals in the health care delivery and its economic considerations but also to provide health related quality of life (HRQL) for a community. v The hit and trial method of combining drugs should be replaced by a rational and logical basis for bringing out a fixed dose drug formulation. Operational, statistical and mathematical models constitute a highly versatile framework for mechanism based modeling (pharmacokinetic/ pharmacodynamic) by taking signal transduction properties of the drug combination into account. Sound scientific research should underline the development and production of drug combinations. v There is a need to carefully monitor and censor misleading claims by the pharmaceutical industry. Some degree of irresponsibility on the part of the pharmaceutical industry and lack of vigilance of government agencies underlies the increased popularity of irrational drug combinations. Most advertisements in many of the medical journals published from India fail to mention important
details pertaining to correct usage of drug combinations. Clinical pharmacist can play an important role in guiding and imparting knowledge to the public. v There is a need to strengthen the mechanism for continuing professional development of practitioners to ensure that they have the necessary knowledge and skills to prescribe rationally. Perhaps the insistence that prescribers especially those in private practice should undergo a continuing medical education (CME) course once in year on newer combinations, new drug molecules introduced in to market and adverse drug reaction will go to a long way in curbing irrational prescribing. v Adverse drug reactions (ADR) reporting should be made mandatory as they are in developed countries. Pharmacovigilance should be more effective. v Hospitals should constitute drugs and therapeutics review committee to rationalize prescribing. v Finally, medical schools and postgraduate colleges must take the responsibility of training students and young doctors how to assess new drug combinations more logically. Unless we encourage our students to think rationally and independently this menace will continue to grow.
Conclusion
The effective interventions for improving rational use of drugs can be expected from all the members of the health care delivery team. There also needs a political will from decision makers so that these interventions are likely to be implemented on a countrywide basis so as to uplift the medical and all allied paramedical professions. The steps taken in this direction will be helpful to reduce morbidity and mortality rate associated with the drug use. It also will improve the allocation of the resources leading for better availability of necessary drugs with proper costs. At the receiving drug end, patients will be benefited with decreased risk of unwanted affects such as adverse drug reactions and the mergence of drug resistance. Promoting the rational use of drugs will finally results in improved quality, increased accessibility and better quality of life for the community. Health professional actively participate and involve in promoting rational drug use to achieve health related quality of life.
Irrational drug use is a very serious global public health problem and much more policy implementation is needed at national leveL.Many studies have been done to document drug use patterns, and indicate that overprescribing, multi-drug prescribing, misuse of drugs, use of unnecessary expensive drugs and overuse of antibiotics and injections are the most common problems of irrational drug use by prescribers as well as consumers. Medically inappropriate, ineffective, and economically inefficient use of pharmaceuticals is commonly observed in the health care system throughout the world especially in the developing countries. However, various forms of inappropriate prescribing often remain unnoticed by those who are involved in health sector decision making or delivery of health services. This problem will usually come to the attention of health decision makers or managers when there is an acute shortage of pharmaceutical budget and action for cost efficiency is required. As I notice during time period of my training in hospital there was the irrational use of pharmaceutical drugs, contributing to increasing resistance by microbes that cause infectious diseases to anti-microbial medicines, was one of the more interesting issues brought up at the World Health Assembly (WHA). The World Health Organisation says that anti-microbial resistance is one of the worlds most serious public health problems. A major cause is the wrong use of medicines. The study involved interviewing primary health care workers and observing the activities carried out by the health workers. Health workers with long service were more prone to over-diagnose malaria and ill-defined conditions and prescribe drugs not indicated, than those who had recently qualified. Over 60% of the health workers in the study areas prescribed drugs requested by patients. Traditional local beliefs on drug-use played a role in irrational drug usage. I notice some Common patterns of irrational prescribing, may, therefore be manifested in the following forms: The use of drugs when no drug therapy is indicated, e.g., antibiotics for viral upper respiratory infections, The use of the wrong drug for a specific condition requiring drug therapy, e.g., tetracycline in childhood diarrhea requiring ORS, The use of drugs with doubtful/unproven efficacy, e.g., the use of antimotility agents in acute diarrhea, The use of drugs of uncertain safety status, e.g., use of dipyrone (Baralgan, etc.),
Failure to provide available, safe, and effective drugs, e.g., failure to vaccinate against measles or tetanus, failure to prescribe ORS for acute diarrhea, The use of correct drugs with incorrect administration, dosages, and duration, e.g., the use of IV metronidazole when suppositories or oral formulations would be appropriate. The use of unnecessarily expensive drugs, e.g.the use of a third generation, broad spectrum antimicrobial when a first-line, narrow spectrum, agent is indicated. Some examples of commonly encountered inappropriate prescribing practices in many health care settings include:
Overuse of antibiotics and antidiarrheals for non-specific childhood diarrhea, Indiscriminate use of injections, e.g., in malaria treatment, Multiple drug prescriptions, Excessive use of antibiotics for treating minor ARI. Minerals and tonics for malnutrition. For Consumers this may have a very different perspective as what is rational.
Notice some Factors Underlying Irrational Use of Drugs There are many different factors which affect the irrational use of drugs. In addition, different cultures view drugs in different ways, and this can affect the way drugs are used. The major forces can be categorized as those deriving from patients, prescribers, the workplace, the supply system including industry influences, regulation, drug information and misinformation, and combinations of these factors.
Patients drug misinformation misleading beliefs patient demands/expectations
inappropriate role modelslack of objective Prescribers lack of education and drug informationgeneralization of limited training experience misleading beliefs about drugs efficacy - pressure to prescribe- lack of adequate lab capacity - insufficient staffing unreliable drug shortages
Workplace heavy patient load
Drug
Supply
System
suppliers
expired drugs supplied
Drug Regulation non-essential drugs non-formal prescribers available lack of regulation enforcement Industry promotional activities misleading claims
Potrebbero piacerti anche
- 2000-WHO Drug Information Vol. 14 - No. 4 PDFDocumento79 pagine2000-WHO Drug Information Vol. 14 - No. 4 PDFAngela Castro RNessuna valutazione finora
- 10 Reasons To Legalize All DrugsDocumento2 pagine10 Reasons To Legalize All Drugsbebbydear123Nessuna valutazione finora
- DPA Fact Sheet Criminalization of Prescription Drug UseDocumento1 paginaDPA Fact Sheet Criminalization of Prescription Drug Usewebmaster@drugpolicy.orgNessuna valutazione finora
- Drugs Dilemmas and ChoicesDocumento304 pagineDrugs Dilemmas and ChoicesClément JanequinNessuna valutazione finora
- MASS Pharmacy Law 2014Documento313 pagineMASS Pharmacy Law 20147bostondrNessuna valutazione finora
- PEAC Prescription Drug MisuseDocumento25 paginePEAC Prescription Drug MisuseSdNessuna valutazione finora
- Drug Schedules and Prescription Writing Clifford M. Knapp, PH.DDocumento36 pagineDrug Schedules and Prescription Writing Clifford M. Knapp, PH.DEman ElzeftawyNessuna valutazione finora
- FDA-Drug Disposal GuidelineDocumento2 pagineFDA-Drug Disposal GuidelineDian PusNessuna valutazione finora
- Detox OverviewDocumento6 pagineDetox OverviewLauren ENessuna valutazione finora
- Pharmacist CV TemplateDocumento2 paginePharmacist CV TemplatevractivaNessuna valutazione finora
- Screening ADHDDocumento2 pagineScreening ADHDPsiholog Alina Mirela CraiuNessuna valutazione finora
- Prohibited DrugsDocumento3 pagineProhibited Drugswild girl100% (1)
- Critical Issues in Alcohol and Drugs of Abuse TestingDa EverandCritical Issues in Alcohol and Drugs of Abuse TestingNessuna valutazione finora
- Meditation For Kids - PDFDocumento18 pagineMeditation For Kids - PDFJamesNessuna valutazione finora
- SUD I - Opioid-Related Disorders Cheat Sheet: by ViaDocumento4 pagineSUD I - Opioid-Related Disorders Cheat Sheet: by ViaDonatella S.Nessuna valutazione finora
- Drug and Pharmacy Regulation ActDocumento12 pagineDrug and Pharmacy Regulation ActrajvirNessuna valutazione finora
- Implementation of Anti-Drug CampaignDocumento40 pagineImplementation of Anti-Drug Campaignjake beseraNessuna valutazione finora
- Language of Addiction MedicineDocumento16 pagineLanguage of Addiction MedicineChristopher CookNessuna valutazione finora
- Ketamine For Opiate WithdrawalDocumento3 pagineKetamine For Opiate WithdrawalroboNessuna valutazione finora
- Gombos, Justin - Fooling The Bladder Cops - The Complete Drug Testing Guide PDFDocumento85 pagineGombos, Justin - Fooling The Bladder Cops - The Complete Drug Testing Guide PDFJózsa VilmosNessuna valutazione finora
- The Cancer of Our Society: DrugsDocumento14 pagineThe Cancer of Our Society: DrugsAman Maity100% (1)
- Treatment Approaches For Drug Addiction DrugfactsDocumento10 pagineTreatment Approaches For Drug Addiction DrugfactsMustafa AlmasoudiNessuna valutazione finora
- Pharmacogenetics and PharmacogenomicsDocumento25 paginePharmacogenetics and PharmacogenomicsBogdan CoșmanNessuna valutazione finora
- Yy Yyy Y Yy Y YYYDocumento64 pagineYy Yyy Y Yy Y YYYsreedam100% (1)
- CH 8. Laws Governing The Practice of PharmacyDocumento62 pagineCH 8. Laws Governing The Practice of Pharmacyaberhaneth1163Nessuna valutazione finora
- 150Documento68 pagine150Andrei Miguel RoqueNessuna valutazione finora
- Drug Information ResourcesDocumento34 pagineDrug Information ResourceslucaNessuna valutazione finora
- Substance Use Disorder - Manual For PhysiciansDocumento213 pagineSubstance Use Disorder - Manual For PhysiciansRoh JitenNessuna valutazione finora
- Medical History FormDocumento16 pagineMedical History FormSpreadsheetZONENessuna valutazione finora
- Study of Women Drug UsersDocumento177 pagineStudy of Women Drug UsersIrfan AhmadNessuna valutazione finora
- Modifiers-Table 122015 2Documento25 pagineModifiers-Table 122015 2khatNessuna valutazione finora
- IT 8 - MTK Drug AbuseDocumento223 pagineIT 8 - MTK Drug AbusedeviamufidazaharaNessuna valutazione finora
- Pharmaceutical CareDocumento114 paginePharmaceutical CareRisdaFitriaNessuna valutazione finora
- 8-22-16-Lecture Grand Rounds Drug Drug Interactions PDFDocumento44 pagine8-22-16-Lecture Grand Rounds Drug Drug Interactions PDFCastov LiubițaNessuna valutazione finora
- Impurity Profiling and Drug Characterization: Backdrop and ApproachDocumento17 pagineImpurity Profiling and Drug Characterization: Backdrop and ApproachBaru Chandrasekhar RaoNessuna valutazione finora
- Sources Drug InfoDocumento16 pagineSources Drug InfoAhmed ZakariaNessuna valutazione finora
- Professional Competencies For Canadian Pharmacy Technicians at Entry To PracticeDocumento26 pagineProfessional Competencies For Canadian Pharmacy Technicians at Entry To PracticeAnonymous jVZOuTNessuna valutazione finora
- Managing Clinical PracticeDocumento46 pagineManaging Clinical PracticeAhmad MakhloufNessuna valutazione finora
- Drug Approval & RegulationDocumento62 pagineDrug Approval & Regulationadni_wgNessuna valutazione finora
- 8 GCP R2 ICH TraduccionDocumento78 pagine8 GCP R2 ICH TraduccionGuillermo PocoviNessuna valutazione finora
- TriageDocumento40 pagineTriagerizka50% (2)
- Novel Drug Delivery Techniques-A Changing and Challenging Global ScenarioDocumento15 pagineNovel Drug Delivery Techniques-A Changing and Challenging Global ScenarioARUNKANTH KRISHNAKUMARNessuna valutazione finora
- Safety Data Sheet Quorum Red Ii: Section 1. Product and Company IdentificationDocumento11 pagineSafety Data Sheet Quorum Red Ii: Section 1. Product and Company IdentificationMauricio Camarena100% (1)
- Chapter 3 Rationality of DrugsDocumento56 pagineChapter 3 Rationality of DrugsS.Srinivasan ('Chinu'); Renu KhannaNessuna valutazione finora
- Detox of The Opiate Dependent Pain Patient and Ongoing Pain Control No Diag 12 13 08Documento14 pagineDetox of The Opiate Dependent Pain Patient and Ongoing Pain Control No Diag 12 13 08Rick Chavez, M.D.100% (1)
- Drug ScreenDocumento94 pagineDrug ScreenardodotNessuna valutazione finora
- Dawson Compton Grant 2010Documento10 pagineDawson Compton Grant 2010Francisco Porá TuzinkievichNessuna valutazione finora
- Medical Conditions HandoutDocumento19 pagineMedical Conditions HandoutMPPNessuna valutazione finora
- Alcohol and DrugsDocumento16 pagineAlcohol and DrugsPame RománNessuna valutazione finora
- 9b) Medical Complications of Drug TakingDocumento19 pagine9b) Medical Complications of Drug TakingDr. Zirwa AsimNessuna valutazione finora
- Health Article - Illicit Drugs and Drug InteractionsDocumento6 pagineHealth Article - Illicit Drugs and Drug Interactions733Nessuna valutazione finora
- Heroin Addiction PaperDocumento9 pagineHeroin Addiction Paperapi-400796139Nessuna valutazione finora
- Evans, D., 2013. The Economic Impacts of Marijuana Legalization.Documento39 pagineEvans, D., 2013. The Economic Impacts of Marijuana Legalization.maja0205Nessuna valutazione finora
- NDPS Saliet FeatyresDocumento63 pagineNDPS Saliet FeatyrespzohmingthangaNessuna valutazione finora
- Oklahoma's Low-THC LawDocumento1 paginaOklahoma's Low-THC LawMPPNessuna valutazione finora
- Psychopharmacologic Drugs: - Antipsychotic Agents - Antimanic Drugs - Antidepressant DrugsDocumento18 paginePsychopharmacologic Drugs: - Antipsychotic Agents - Antimanic Drugs - Antidepressant DrugsDrima EdiNessuna valutazione finora
- Safe, Legal Access To Marijuana Can Help Fight The Opioid EpidemicDocumento1 paginaSafe, Legal Access To Marijuana Can Help Fight The Opioid EpidemicMPPNessuna valutazione finora
- Irrational Drug CombiDocumento2 pagineIrrational Drug CombiabkinareNessuna valutazione finora
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceDa EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceValutazione: 3 su 5 stelle3/5 (1)
- Pharmacovigilance Ensuring The Safe Use of MedicinesDocumento18 paginePharmacovigilance Ensuring The Safe Use of MedicinespopadrianionutzNessuna valutazione finora
- Problems of Irrational Drug Use: Session GuideDocumento22 pagineProblems of Irrational Drug Use: Session Guidearyo aryoNessuna valutazione finora
- Poly PharmacyDocumento17 paginePoly PharmacyAubrey ManimtimNessuna valutazione finora
- RUM NewDocumento53 pagineRUM NewbennyNessuna valutazione finora
- Anatomyofthe Annexesofthe Digestive TractDocumento67 pagineAnatomyofthe Annexesofthe Digestive TractsreedamNessuna valutazione finora
- Dose AdjustmentDocumento30 pagineDose AdjustmentsreedamNessuna valutazione finora
- Barrons 333 High Freq Words With Meanings PDFDocumento8 pagineBarrons 333 High Freq Words With Meanings PDFahmedhussien1Nessuna valutazione finora
- Fundamentals of SalivaDocumento15 pagineFundamentals of SalivasreedamNessuna valutazione finora
- Scribe 4Documento4 pagineScribe 4sreedamNessuna valutazione finora
- Standard Treatment GuidelineDocumento261 pagineStandard Treatment GuidelineEmaNessuna valutazione finora
- Unit 5-Soil Science Soil FertilityDocumento20 pagineUnit 5-Soil Science Soil FertilitysreedamNessuna valutazione finora
- Dental ProductsDocumento13 pagineDental ProductssreedamNessuna valutazione finora
- Thompson & Thompson Genetics in Medicine Genetik EthicDocumento21 pagineThompson & Thompson Genetics in Medicine Genetik EthickartalxyusufNessuna valutazione finora
- UntitledDocumento6 pagineUntitledPriscilla GabanamotseNessuna valutazione finora
- Medical Treatment Recuperation Convalescence With HomoeopathyDocumento4 pagineMedical Treatment Recuperation Convalescence With HomoeopathyEditor IJTSRDNessuna valutazione finora
- PPT Referat Syok Argia AnjaniDocumento34 paginePPT Referat Syok Argia Anjanidhana2395Nessuna valutazione finora
- FluidDocumento190 pagineFluidAndrias OzNessuna valutazione finora
- Module 5 MGCQ Edition The Physical and Sexual SelfDocumento28 pagineModule 5 MGCQ Edition The Physical and Sexual SelfRan Dy MangosingNessuna valutazione finora
- Guide Questions For NCM 107Documento4 pagineGuide Questions For NCM 107Miguel LigasNessuna valutazione finora
- Homework PaperDocumento12 pagineHomework Paperapi-509662228Nessuna valutazione finora
- Regulatory Bodies of Nursing in India: Dr. Maheswari JaikumarDocumento75 pagineRegulatory Bodies of Nursing in India: Dr. Maheswari Jaikumarkalla sharonNessuna valutazione finora
- GMC Handwara Recruitment 2023Documento4 pagineGMC Handwara Recruitment 2023Ummar WaniNessuna valutazione finora
- The Early Trauma Inventory Self Report-Short FormDocumento8 pagineThe Early Trauma Inventory Self Report-Short FormMiguel Angel Alemany NaveirasNessuna valutazione finora
- InBody 270Documento27 pagineInBody 270lee CeeNessuna valutazione finora
- Physical Fitness TestDocumento5 paginePhysical Fitness TestJhona Nodado RiveraNessuna valutazione finora
- Mo2vate Issue 15 - March 2022Documento74 pagineMo2vate Issue 15 - March 2022Mo2vate MagazineNessuna valutazione finora
- Reflection 1Documento5 pagineReflection 1api-400554289Nessuna valutazione finora
- Product Monograph of TelmisartanDocumento8 pagineProduct Monograph of Telmisartandini hanifaNessuna valutazione finora
- Himachal StatsDocumento115 pagineHimachal StatsVikrant ChaudharyNessuna valutazione finora
- 10 Physical and Mental Benefits of BasketballDocumento4 pagine10 Physical and Mental Benefits of BasketballJohn Kenzo NavatoNessuna valutazione finora
- Ab Respiratory Assessment NPG GuidelinesDocumento10 pagineAb Respiratory Assessment NPG GuidelinesSuhaila NajibNessuna valutazione finora
- FARC-01 - Senior First Aid (Occupational First Aid Course OFAC)Documento2 pagineFARC-01 - Senior First Aid (Occupational First Aid Course OFAC)Ewien Vars SianturieNessuna valutazione finora
- Burning Mouth SyndromeDocumento28 pagineBurning Mouth SyndromeMelissa KanggrianiNessuna valutazione finora
- STROBE Case-Control Study PDFDocumento3 pagineSTROBE Case-Control Study PDFLuis Gabriel Parra LaraNessuna valutazione finora
- Nifedipine and Prednisone Drug StudyDocumento4 pagineNifedipine and Prednisone Drug StudyJomer GonzalesNessuna valutazione finora
- Supporting Young Children's Emotional Well-Being: Cumbria County CouncilDocumento32 pagineSupporting Young Children's Emotional Well-Being: Cumbria County CouncilAlbina ScutaruNessuna valutazione finora
- Bacteria and Viruses PDFDocumento1 paginaBacteria and Viruses PDFSchöne Frau TapiaNessuna valutazione finora