Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
NCP For FT, SGA
Caricato da
Jule SantoyaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
NCP For FT, SGA
Caricato da
Jule SantoyaCopyright:
Formati disponibili
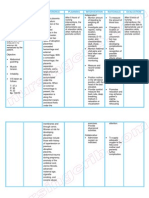
NCP for FullTerm, Small for Gestational Age
DEVIATIONS IN GROWTH PATTERNS Deviations in intrauterine growth patterns not only increase the risk of morbidity and mortality in the early newborn period, but may also have long-term implications for altered growth and development and for altered CNS function and learning disabilities in childhood. This general plan of care is designed to facilitate optimal nursing management of the infant with deviations in intrauterine growth and is to be used in conjunction with the CPs: The Neonate at Two Hours to Two Days of Age, and The Preterm Infant, as appropriate. Growth deviations are classified as SGA, intrauterine growth retardation/restriction (IUGR), and LGA. SGA/IUGR: Any newborn whose birth weight falls at or below the 10th percentile on classification charts, considering local factors (e.g., ethnicity, altitude). LGA/Macrosomic: Any newborn whose birth weight is at or above the 90th percentile on classification charts, considering local population at any week in gestation (with special attention to determining appropriate gestational age), or who at birth weighs more than 4000 g (8 lb 13 oz). DIAGNOSTIC STUDIES Dextrostix Glucose Estimations: Less than 40 mg/dl in LGA infant or 25 mg/dl in SGA infant during first 3 days indicates hypoglycemia. Serum Glucose: Verifies Dextrostix value <40 mg/dl in LGA infant ,25 mg/dl in SGA infant. Chest X-Ray and ABGs: Help determine cause/severity of respiratory distress if present, e.g., pneumonia, MAS, RDS. CBC: May reveal central venous Hct elevated above 65%; central venous Hb 20 g/dl associated with polycythemia/hyperviscosity. WBC Count: May be elevated or depressed. Platelet Count: May be depressed if mother was pre-eclamptic or if infant was born with a congenital viral infection. Coagulation Studies (prothrombin time [PT], partial thromboplastin time [PTT], fibrinogen, fibrin split products [FSP]): May indicate DIC, especially in the presence of polycythemia or asphyxia. Blood Type for ABO Group, Rh Factor, and Crossmatch: Plasma exchange may be necessary if Rh incompatibility exists. Serum Electrolytes (including ionized calcium): Assesses for hypocalcemia (level 7 mg/dl [3.5 mEq/L] or less in first 3 days of life); inappropriate antidiuretic hormone secretion, and instability related to metabolic complications. Bilirubin: May be elevated secondary to polycythemia and resorption of bleeding associated with birth injury, e.g., intracranial hemorrhage, cephalhematoma. Urinalysis on/after Second Voided Specimen, Including Specific Gravity and Sugar/Acetone: Assesses homeostasis, renal involvement. Bacterial and Viral Cultures: Rule out/diagnose infectious process. Electrocardiography (ECG), Echocardiography, Ultrasonography, Angiography, and Genetic Studies: As appropriate with suspected FAS, congenital defects, and/or complications. NURSING PRIORITIES 1. Maintain physiological homeostasis. 2. Prevent and/or treat complications. 3. Identify/minimize effects of birth trauma. 4. Provide family with appropriate information/strategies for meeting short- and long-term needs associated with growth deviation.
NURSING DIAGNOSIS: NUTRITION: altered, less than body requirements May Be Related To: Decreased nutritional stores, increased insulin production and/or hyperplasia of the pancreatic beta cells Possibly Evidenced By: Weight deviation from expected; decreased muscle mass/fat stores, electrolyte imbalance DESIRED OUTCOMES/EVALUATION CRITERIANEONATE WILL: Ingest and digest adequate nutrients for weight gain (or to prevent weight loss of 2% or more). Display serum glucose >40 mg/ dl, and other associated laboratory studies WNL. PARENT(S) WILL: Identify/treat/prevent short- and long-term complications of malnutrition. ACTIONS/INTERVENTIONS: A.Independent 1. Compare weight in relation to gestational age and size. Document on growth chart. Weigh daily. 2. Maintain thermoneutral environment, including use of incubator/radiant warmer, as indicated. Monitor heat controls, temperature of infant and environment frequently, noting hypothermia/ hyperthermia. 3. Initiate early and frequent feedings and advance as tolerated. 4. Assess tolerance to feedings. Note stool color, consistency, and frequency; presence of reducing substances; abdominal girth; vomiting, and gastric residuals. 5. Monitor intake and output. Calculate daily caloric and electrolyte consumption. 6. Assess hydration level, noting fontanels, skin turgor, urine specific gravity, condition of mucous membranes, and weight fluctuations. 7. Monitor Dextrostix levels immediately after birth and routinely until serum glucose is stabilized. 8. Observe for signs of hypoglycemia, e.g., tachypnea and irregular respirations, apnea, lethargy, flaccidity, cyanosis, temperature fluctuations, diaphoresis, poor feeding, jitteriness, high-pitched cry, tremors, eye rolling, seizure activity. 9. Note signs of hypocalcemia, e.g., neuromuscular
irritability (tremors, twitching, seizing, clonus), hypotonia, vomiting, high-pitched cry, cyanosis, apnea, and cardiac dysrhythmias with prolonged Q-T interval. 10. Discuss long-term complications of malnutrition in SGA infant and obesity in LGA infant; review importance of protein during phase II of brain growth. B.Collaborative 1. Monitor laboratory studies as indicated: Serum glucose; 2. Calcium; 3. Sodium, potassium, chloride, phosphorus, and magnesium;
RATIONALE: 1. Identifies presence, degree, and risk of altered growth pattern. SGA infant may have already lost weight in utero or may suffer from reduced fat/glycogen stores. 2. The SGA infant does not have adequate adipose tissue for insulation and has a large body surface area compared to body weight. Brown adipose tissue stores may be inadequate to maintain thermoregulation. Both hypothermia and hyperthermia increase metabolic demands, necessitating increased intake in an already compromised infant. Note: Thermal instability may be iatrogenically induced by improperly operated heating equipment used to maintain thermogenesis in dysmature infant. 3. Assists in maintaining fluid/electrolyte balance and meeting caloric needs to support metabolic process. Helps prevent hypoglycemia associated with inadequate body stores in SGA infant or continued pancreatic secretion of insulin in IDM. 4. Advances in amount and caloric composition of feedings are dependent on tolerance. Evidence of reducing substances (increased glucose) in stool suggests inability to digest formula because of obstruction and/or disease process present. Note: Poor sucking reflex and recurrent vomiting or persistent regurgitation may be seen in FAS, requiring further evaluation/intervention. 5. Provides information about actual intake in relation to estimated needs for use in readjustment of dietary prescription.
6. Increased metabolic demands of the SGA infant may increase fluid requirements. Hyperglycemic states may produce diuresis in the infant. IV administration of fluids may be required to meet increased demands but must be conscientiously managed to avoid fluid excess. 7. Hypoglycemia may occur after birth because of limited glucose stores in the SGA infant. Symptoms in the SGA infant usually appear between 24 and 72 hr of age, but may begin as early as 3 hr or as late as 7 days; the IDM may be symptomatic within 13 hr of birth. Hyperglycemia may result from inappropriate infusion of solutions containing glucose. 8. Because glucose is a major source of fuel for the brain, deficits may cause permanent CNS damage. Hypoglycemia significantly increases morbidity and mortality rates, and severity of long-term effects is dependent on duration of such episodes. 9. Peak incidence of early hypocalcemia is during first 4872 hr of life and is often related to temporary abdominal distension, neonatal hypoparathyroidism in premature infant, or prenatal asphyxia in SGA infant or IDM. 10. Chronic protein deficiencies in the SGA infant make child prone to learning difficulties and cerebral dysfunction, characterized by short attention span, poor fine-motor coordination, hyperactivity behavior problems , and speech defects. Collaborative RATIONALE: 1. Hypoglycemia may occur as early as 13 hr after birth. In the SGA infant, glycogen reserves are quickly depleted and gluconeogenesis is inadequate because of reduced stores of muscle protein and fat, while the IDM has decreased ability to release glucagon and catecholamines needed to stimulate glucagon breakdown/facilitate release of glucose. 2. Frequency of screening is dependent on this risk group, i.e., IDM, intrapartal asphyxia, or preterm infants. Levels 7 mg/dl require further evaluation/intervention. 3. Electrolyte instability may be a consequence of deviations in growth, inadequate placental transfer, or altered maternal mineral balance. Note: Hypomagnesemia/hyperphosphatemia are usually associated with hypocalcemia.
SOURCE: http://www.scribd.com/doc/9658688/Deviations-in-Growth-Patterns
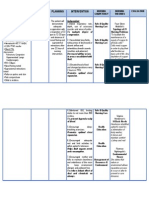
Small-for-gestational age Newborn (SGA)
Description
1. An SGA infant is one whose length, weight, and had circumference are below the 10th percentile of the normal variation for gestational age as determined by neonatal examination. 2. The SGA infant may be preterm, term, or post-term.
Etiology
1. Maternal conditions associated with SGA babies include: o Hypertension (chronic or pregnancy- induced) o Cardiac, pulmonary, or renal disease o Diabetes mellitus (classes D,E,F, and R) o Poor nutrition o Use of alcohol, tobacco, or drugs o Age o Multiple gestation o Placental insufficiency o Placental fetal abnormalities o Pregnancy occurred at high altitudes 2. Fetal conditions associated with SGA infants include: o Normal genetically small infant o Chromosomal abnormality o Malformations o Congenital infections, especially rubella and cytomegalovirus 3. The effect of these factors upon the fetus is dependent on the stage of fetal development. o Early gestation is a time of rapid cell proliferation. An insult at this time results in organs that contain normal size cells, but they are fewer in number. Infants are symmetrical (their heads and bodies grew proportionately) but their organs are smaller. Usually these infants have a poor prognosis and may never catch up. o Later in gestation, growth of the fetus results from an increase in cell size. An insult at this time results in organs with a normal number of cells that are smaller in size and causes asymmetric growth. These infants have appropriate-sized heads and body lengths, but their weight and organ sizes are decreased. These infants usually have a better prognosis since they have an adequate number of cells. Their growth catches up if they are provided with good nutrition postnatally.
Assessment Findings 1. Clinical manifestations
Soft tissue wasting and dysmaturity Loose, dry, and scaling skin Perinatal asphyxia (due to a small placenta that is less efficient in gas exchange) Plethora, respiratory distress, and central nervous system (CNS) aberrations (if the infant has polycythemia) Congenital anomalies (occurring in as many as 35% of SGA infants who suffered insults early in gestation)
2. Laboratory and diagnostic study findings
Glucose testing will reveal decreased glycogen stores, which increases the potential for hypothermia and hypoglycemia. Hematocrit level may be increased (65%), which indicates polycythemia as a result of chronic fetal hypoxia.
Nursing Management
1. Provide adequate fluid and electrolytes and nutrition. o Provide a high calorie formula for feeding (more than 20 calories per ounce) to promote steady weight gain (15 to 30 grams per day growth plotted on curves shows a normal growth rate). o If the infant is breast feeding, add human milk fortifier to expressed breast milk. 2. Decrease metabolic demands when possible. o Provide small frequent feedings. o Provide gavage feedings if the infant does not have a steady weight gain. o Provide a neutral thermal environment. o Decrease iatrogenic stimuli. 3. Prevent hypoglycemia o Monitor glucose screening. o Provide early feedings. o Provide frequent feedings (every 2 to 3 hours) o Administer IV glucose if blood sugar does not normalize with oral feedings. 4. Maintain a neutral thermal environment. 5. Monitor serum hematocrit (normal is 45% to 65%). o If an initial high hematocrit was obtained by heel stick capillary sample, a follow-up sample should be done by venipuncture. o Observe for signs, symptoms, and complications of polycythemia o Ruddy appearance Cyanosis Lethargy, jitteriness, and seizures Jaundice
Provide adequate hydration to prevent hyperviscosity
6. Assess the prenatal history for possible toxoplasmosis, rubella, cytomegalovirus, and herpes simplex infections during pregnancy. Assess maternal and infant antibody titers. Use isolation precautions when congenital infections are suspected. 7. Provide education and emotional support. o o o Explain the possible causes of intrauterine growth retardation. Inform parents of the infants goal weight for discharge. Provide instruction on managing the infant at home. Explain how to prepare a higher calorie formula or breast feeding. Explain the importance of follow-up with a developmental specialist who will screen for milestone achievements.
SOURCE: http://www.rnpedia.com/home/notes/maternal-child-nursing-notes/small-for-gestational-age-newborn-sga
Potrebbero piacerti anche
- Infection NCPDocumento1 paginaInfection NCPMsOrangeNessuna valutazione finora
- Nursing Care Plan JaudiceDocumento3 pagineNursing Care Plan Jaudicepapadaad100% (1)
- SDL1 NCP Case2Documento3 pagineSDL1 NCP Case2Alec AnonNessuna valutazione finora
- OB Nursing Care PlanDocumento3 pagineOB Nursing Care PlanLiza Marie Cayetano AdarneNessuna valutazione finora
- Fetal DistressDocumento5 pagineFetal DistressRonnie Portillo Cruz100% (1)
- Nursing Diagnosis and Nursing Interventions For HirschsprungDocumento5 pagineNursing Diagnosis and Nursing Interventions For HirschsprungAhmed Altrafe100% (2)
- Newborn Hypothermia and Hyperthermia (Final Copy)Documento30 pagineNewborn Hypothermia and Hyperthermia (Final Copy)Shizuka Marycris Amane67% (3)
- Precipitous Labor/Delivery or Unplanned/Out-of-Hospital DeliveryDocumento7 paginePrecipitous Labor/Delivery or Unplanned/Out-of-Hospital DeliveryLei Ortega100% (1)
- NCP Pain - OBDocumento5 pagineNCP Pain - OBSandra Guimaray50% (2)
- NCP Less Than Body Req.Documento2 pagineNCP Less Than Body Req.Mary Ann Contreras100% (1)
- NB Nursing DiagnosisDocumento2 pagineNB Nursing Diagnosisnursingmvd92% (13)
- Date Cues Nursing Diagnosis Scientific Basis Goal of Care Nutsing Interventi ON Rationale EvaluationDocumento5 pagineDate Cues Nursing Diagnosis Scientific Basis Goal of Care Nutsing Interventi ON Rationale EvaluationNathalie kate petallarNessuna valutazione finora
- Altered Parent Infant NCP PDFDocumento3 pagineAltered Parent Infant NCP PDFAebee AlcarazNessuna valutazione finora
- Nursing Care Plan: Cues Objectives Interventions Rationale EvaluationDocumento1 paginaNursing Care Plan: Cues Objectives Interventions Rationale EvaluationlaehaaaNessuna valutazione finora
- Case PresentationDocumento39 pagineCase PresentationJOSHUA DICHOSONessuna valutazione finora
- Teaching Plan On Newborn ScreeningDocumento5 pagineTeaching Plan On Newborn ScreeningKramSenarevolNessuna valutazione finora
- Rle 107 Maternal and Child Health Nursing: University of The Assumption College of Nursing and PharmacyDocumento6 pagineRle 107 Maternal and Child Health Nursing: University of The Assumption College of Nursing and PharmacyEvangeline Anne Macanas100% (2)
- NCP: Labor Stage 1 Transition Phase (Deceleration)Documento7 pagineNCP: Labor Stage 1 Transition Phase (Deceleration)JavieNessuna valutazione finora
- First TrimesterDocumento18 pagineFirst Trimesternursereview100% (9)
- Altered Tissue Perfusion UteroplacentalDocumento4 pagineAltered Tissue Perfusion UteroplacentalAlyNessuna valutazione finora
- Nursing Care Plan 3 Risk For Altered ParentingDocumento7 pagineNursing Care Plan 3 Risk For Altered Parentingdbryant010178% (9)
- Assessment Nursing Diagnoses Planning Implementation Rationale Evaluation Subjective Data: Short-Term GoalDocumento2 pagineAssessment Nursing Diagnoses Planning Implementation Rationale Evaluation Subjective Data: Short-Term GoalMark oliver Gonzales100% (1)
- Care Plan Redo For NeonateDocumento2 pagineCare Plan Redo For NeonateIris Lopez100% (6)
- NCP - BreastfeedingDocumento1 paginaNCP - Breastfeedingheather tbwn100% (1)
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocumento1 paginaNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNessuna valutazione finora
- Family Nursing Care Plan SeizuresDocumento3 pagineFamily Nursing Care Plan SeizuresClaire AlcantaraNessuna valutazione finora
- Bronchopneumonia Care PlanDocumento6 pagineBronchopneumonia Care PlanAbhijit Soundade0% (1)
- NCP PregnantDocumento4 pagineNCP PregnantSophia Caisip0% (1)
- NCPDocumento6 pagineNCPFerreze AnnNessuna valutazione finora
- Case Analysis CHN2Documento3 pagineCase Analysis CHN2Nicxx GamingNessuna valutazione finora
- Scabies Case Study NCPDocumento6 pagineScabies Case Study NCPEmeEmekaNessuna valutazione finora
- NSO - Adam's Forward Bend TestDocumento2 pagineNSO - Adam's Forward Bend TestMaha AmilNessuna valutazione finora
- Nursing Care Plan: IndependentDocumento2 pagineNursing Care Plan: IndependentAdhaNessuna valutazione finora
- NCP OB Ward - Imbalanced NutritionDocumento2 pagineNCP OB Ward - Imbalanced NutritionCk JosueNessuna valutazione finora
- Nursing Care Plan Abruptio PlacentaeDocumento2 pagineNursing Care Plan Abruptio PlacentaeWann WannNessuna valutazione finora
- Case NCPDocumento25 pagineCase NCPJoher Bolante Mendez100% (1)
- NCP SepsisDocumento6 pagineNCP SepsisgopscharanNessuna valutazione finora
- NCP For Postpartum DiscomfortsDocumento3 pagineNCP For Postpartum DiscomfortsCamille Maluenda - Tan0% (1)
- Hyperthermia (Thurs)Documento1 paginaHyperthermia (Thurs)Christine Esguerra OrozcoNessuna valutazione finora
- Newborn Careplan 9-15-2011Documento17 pagineNewborn Careplan 9-15-2011Brittany Wood100% (1)
- Macronutrients-Carbohydrates: NCM 105A Nutrition and Diet Therapy Laborator YDocumento3 pagineMacronutrients-Carbohydrates: NCM 105A Nutrition and Diet Therapy Laborator YArriane Desepeda100% (1)
- Nursing Care PlanDocumento3 pagineNursing Care PlanArvan James Cabugayan TalboNessuna valutazione finora
- Case Pres With NCP at PNPDocumento33 pagineCase Pres With NCP at PNPsitaw80% (10)
- Discharge PlanningDocumento3 pagineDischarge PlanningAlex Marie100% (2)
- Problem PrioritizationDocumento2 pagineProblem PrioritizationRegie GonzagaNessuna valutazione finora
- NCP Imbalanced NutritionDocumento4 pagineNCP Imbalanced NutritionChelsea Wu100% (2)
- Cleft Lip Palate NCPDocumento2 pagineCleft Lip Palate NCPLerma PagcaliwanganNessuna valutazione finora
- OB Nursing Care PlanDocumento3 pagineOB Nursing Care PlanChristine V. Fernandez100% (3)
- NCP On Postpartum MotherDocumento9 pagineNCP On Postpartum MotherM.S.H Tube100% (1)
- Labor Nursing Care PlansDocumento58 pagineLabor Nursing Care PlansMuhamad AriNessuna valutazione finora
- NCP BleedingDocumento3 pagineNCP Bleedingapi-316491996Nessuna valutazione finora
- NCP Diabetes Mellitus Prepregnancy GestationalDocumento12 pagineNCP Diabetes Mellitus Prepregnancy GestationalRichson BacayNessuna valutazione finora
- Colegio de Sta. Lourdes of Leyte Foundation, Inc. College of Nursing Tabontabon, LeyteDocumento3 pagineColegio de Sta. Lourdes of Leyte Foundation, Inc. College of Nursing Tabontabon, LeyteHassen ZabalaNessuna valutazione finora
- Yusuf Transientpersistenthypoglycemia 140620152304 Phpapp01Documento53 pagineYusuf Transientpersistenthypoglycemia 140620152304 Phpapp01Brotherhood of KryptonianNessuna valutazione finora
- Neonatal HypoglycemiaDocumento14 pagineNeonatal HypoglycemiaAkankshaNessuna valutazione finora
- NCP - Diabetes Mellitus Prepregnancy/GestationalDocumento13 pagineNCP - Diabetes Mellitus Prepregnancy/GestationalClaudine Christophe100% (1)
- FTTDocumento7 pagineFTTmemopolkadotsNessuna valutazione finora
- Neonatal Hypoglycemia APNECDocumento26 pagineNeonatal Hypoglycemia APNECyumicheongNessuna valutazione finora
- Practice Essentials: Neonatal HypoglycemiaDocumento15 paginePractice Essentials: Neonatal HypoglycemianadiancupNessuna valutazione finora
- India Journal of Pediatrics HypoglicemiaDocumento6 pagineIndia Journal of Pediatrics HypoglicemiaJermaine Marlon RVNessuna valutazione finora
- Drug Study - Metronidazole (Flagyl)Documento1 paginaDrug Study - Metronidazole (Flagyl)Jule SantoyaNessuna valutazione finora
- Dopamine HydrochlorideDocumento1 paginaDopamine HydrochlorideJoannes SanchezNessuna valutazione finora
- Health Teaching For B.P.U.D.Documento10 pagineHealth Teaching For B.P.U.D.Jule SantoyaNessuna valutazione finora
- Vit. ADocumento3 pagineVit. AJule Santoya100% (1)
- Community Acquired PneumoniaDocumento9 pagineCommunity Acquired PneumoniaJule SantoyaNessuna valutazione finora
- First Prenatal VisitDocumento29 pagineFirst Prenatal VisitLucas Phi100% (1)
- Neonatal Birth InjuriesDocumento22 pagineNeonatal Birth InjuriesPauli Monsálvez ElissaldeNessuna valutazione finora
- Perinatal AsphyxiaDocumento44 paginePerinatal AsphyxiaJan Kirstin EgalinNessuna valutazione finora
- Placenta Previa AbruptioDocumento44 paginePlacenta Previa AbruptiopipitNessuna valutazione finora
- CPG Preterm Labor PDFDocumento90 pagineCPG Preterm Labor PDFJeffrey Arboleda100% (2)
- OB Test 2 Study GuideDocumento21 pagineOB Test 2 Study GuideJaclyn FugateNessuna valutazione finora
- Necrotizing EnterocolitisDocumento43 pagineNecrotizing EnterocolitisRajender SinghNessuna valutazione finora
- Do Early Intervention Programmes Improve Cognitive and Motor Outcomes For Preterm Infants After Discharge A Systematic ReviewDocumento9 pagineDo Early Intervention Programmes Improve Cognitive and Motor Outcomes For Preterm Infants After Discharge A Systematic ReviewJuan Carlos Jiménez FosadoNessuna valutazione finora
- ANC OB and GYN HISTORY Taking SampleDocumento43 pagineANC OB and GYN HISTORY Taking SampleGebremichael Reta100% (3)
- Induction of Labor With Oxytocin - UpToDateDocumento37 pagineInduction of Labor With Oxytocin - UpToDateMerjem DautiNessuna valutazione finora
- Abnormal Lie in PregnancyDocumento2 pagineAbnormal Lie in PregnancyAlexander EnnesNessuna valutazione finora
- Standard Growth ChartsDocumento2 pagineStandard Growth ChartsIsmiralda PratiwiNessuna valutazione finora
- MCN Reviewer: Basic ConceptsDocumento22 pagineMCN Reviewer: Basic ConceptsPanJan BalNessuna valutazione finora
- NS 1 Quiz 3Documento7 pagineNS 1 Quiz 3Marah PacioNessuna valutazione finora
- Problem With The PowersDocumento9 pagineProblem With The PowersNicole Claire LegaspiNessuna valutazione finora
- Drugs Producing Uterine CONTRACTIONS (Oxytocic Drugs) : Oxytocin Ergot Alkaloids ProstaglandinsDocumento9 pagineDrugs Producing Uterine CONTRACTIONS (Oxytocic Drugs) : Oxytocin Ergot Alkaloids ProstaglandinsFaris Jamal Abu Za'nounehNessuna valutazione finora
- Tandabui Institute of Health and Allied ScienceDocumento30 pagineTandabui Institute of Health and Allied ScienceJames MasomeNessuna valutazione finora
- Mother-to-Child Transmission of HIV: Pathogenesis, Mechanisms and PathwaysDocumento18 pagineMother-to-Child Transmission of HIV: Pathogenesis, Mechanisms and Pathwaysnegara ipdNessuna valutazione finora
- DR Johnson On Neonatal Resuscitation Guidelines 041707Documento44 pagineDR Johnson On Neonatal Resuscitation Guidelines 041707sameerarswNessuna valutazione finora
- Adolescent Preeclampsia Pathological Drivers and Clinical PreventionDocumento13 pagineAdolescent Preeclampsia Pathological Drivers and Clinical PreventionEmmanuel Guevara HernándezNessuna valutazione finora
- Prenatal Care and Role of Pediatric NurseDocumento40 paginePrenatal Care and Role of Pediatric NurseMANEESH MANI67% (3)
- Augmentation and IOLDocumento24 pagineAugmentation and IOLBlessy MadhuriNessuna valutazione finora
- Pemotongan Tali PusatDocumento58 paginePemotongan Tali PusatNi Putu ElindaNessuna valutazione finora
- Midwife Prometric Test1Documento17 pagineMidwife Prometric Test1Nesrine TrabelsiNessuna valutazione finora
- Antenatal Guidelines KemhDocumento54 pagineAntenatal Guidelines KemhqurbanNessuna valutazione finora
- Multiple Pregnancy NOR PosterDocumento1 paginaMultiple Pregnancy NOR PosterbigbossNessuna valutazione finora
- Ojsadmin, 993Documento6 pagineOjsadmin, 993pondyNessuna valutazione finora
- Antidote M4 Tcon Union'22Documento68 pagineAntidote M4 Tcon Union'22FeelNessuna valutazione finora
- اسئله نسائيه)Documento47 pagineاسئله نسائيه)ملك عيسىNessuna valutazione finora
- Tissue Pathway For Histopathological Examination of The PlacentaDocumento18 pagineTissue Pathway For Histopathological Examination of The PlacentaArifah Azizah ArifinNessuna valutazione finora