Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
SLE Concept Map
Caricato da
adrienne cervantesCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
SLE Concept Map
Caricato da
adrienne cervantesCopyright:
Formati disponibili
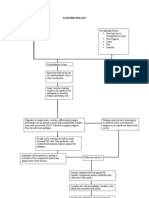
RISK FACTORS Cause of Lupus is unknown, A familial association suggests genetic predisposition.
Environmental factors, susceptibility to certain viruses, an immune system dysfunction with production of auto antibodies, Hormonal abnormality, Ultraviolet radiation, Drugs: hydralazine, hydrochloride ,procainamide hydrochloride, penicillin, isonicotinic acid hydrazide, chlorpromazine, phenytoin, and quinidine (can cause onset of lupus like symptoms and aggravate existing disease)
MEDICAL CONDITION A Systemic Lupus Erythemous/Anemia
ASSESSMENT DATA VS: T: 98.0 P: 54 RR: 18 BP: 128 / 78 Pain Num: 0/10 2 sat: 98% RBC: L 2.29 (4.0 5.90) m/cumm HGB: 7.9 L ( 13.8 16.9) LS Clear:LUQ, RUQ,LLQ,RLQ BS: active x 4 quads, No tenderness noted on liver or spleen upon palpation, Edema: R arm mild non pitting BLE: edema +2 pitting edema, minor ecchymosis on R wrist., No Skin rashes or lesions present, Active ROM , Hair loss, NO SLIV Total Urine output during shift: 650 Fluid intake: 480 Diet: renal ( pt ate 100%)
NURSING DIAGNOSIS Pain r/t Inflammation Alteration in comfort r/t edema and joint pain, peripheral nerve inflammation. PLANNING Pharmacologic therapy, adequate rest periods, PT program to maintain mobility, and ROM, observe pt for Renal failure
ETIOLOGY/PATHOPHYSIOLOGY Lupus Erythematosus is an auto immune disease that affects the connective tissue of the body. The course of the disease is variable and unpredictable, with episodes of remission and relapse. SLE is a multisystem inflammatory disease that affects any body system but primarily the Musculoskeletal, cutaneous, renal, nervous, and cardiovascular systems. The multi system nature of SLE places the patient at risk for multiple complications, and the disease is ultimately fatal. The survival or patients with SLE is about 90%@5 yrs. and 80% @ 10 years. The most common causes of death are renal failure and infections, followed by neurological and cardiovascular disorders. Therapy has reduced mortality for 20yr survival to 70% TEACHING Medication teaching Side effects Alternate forms of pain management Diet ROM exercises, mobility, freq rest periods, Use of protective skin barrier sunscreen, skin protection scalp Stress reduction Disease process Coping strategies Referral to support groups
MEDICATIONS Renagel 800mg P.O TID with meals Folic Acid 5mg P.O daily Cellcept 500mg P.O BID Lovenox 40 mg SC q Daily
INTERVENTIONS Analgesic administration, VS, Anxiety reduction, ROM exercises, Frequent rest periods, Pain assessment, Neuro checks, Pain management, Strict I&O, monitor lab values, Patient teaching, Assess patient for s/s of joint pain ,relaxation techniques, Amb with patient ad lib, Comfort measures to decrease pain: warm packs,
EVALUATION Pt had no c/o Pain r/t Inflammation Pt had no c/o Alteration in comfort r/t edema and joint pain, peripheral nerve inflammation.
Potrebbero piacerti anche
- Systemic Lupus Erythematosus PathophysiologyDocumento8 pagineSystemic Lupus Erythematosus Pathophysiologykathy92% (24)
- (The Norton Library) Karen Horney - Feminine Psychology (1973, W W Norton & Co.)Documento276 pagine(The Norton Library) Karen Horney - Feminine Psychology (1973, W W Norton & Co.)daniela86% (7)
- pathoPHYSIOLOGY OF OSTEOMYELITIS (DIAGRAM)Documento1 paginapathoPHYSIOLOGY OF OSTEOMYELITIS (DIAGRAM)redhoney100% (5)
- Wilm's Tumor PathophysiologyDocumento2 pagineWilm's Tumor PathophysiologyJonalene Suarez100% (2)
- SLE PathophysiologyDocumento3 pagineSLE PathophysiologyRanela Kwinkee Pastor Salazar100% (7)
- Lung Cancer Pathophysio and NCPDocumento21 pagineLung Cancer Pathophysio and NCPApple Y.D.Nessuna valutazione finora
- Pathophysiology of Osteomyelitis DiagramDocumento1 paginaPathophysiology of Osteomyelitis DiagramKim Enrico JumarangNessuna valutazione finora
- Final Lung Cancer Concept MapDocumento3 pagineFinal Lung Cancer Concept MapKaycee TolingNessuna valutazione finora
- NCP Lung CancerDocumento4 pagineNCP Lung CancerShizuen Mn83% (12)
- Systemic Lupus Erythematosus Actual PathophysiologyDocumento1 paginaSystemic Lupus Erythematosus Actual PathophysiologyGhan Maria100% (2)
- Guillain Barre Syndrome PathophysiologyDocumento4 pagineGuillain Barre Syndrome Pathophysiologykathy100% (13)
- NCP-Esophageal Varices Pleural EffusionDocumento6 pagineNCP-Esophageal Varices Pleural Effusiontinatin98933% (3)
- Pathophysiology of Status EpilepticusDocumento6 paginePathophysiology of Status EpilepticusKysha Ruth SevillaNessuna valutazione finora
- Brain Cancer Concept MapDocumento3 pagineBrain Cancer Concept MapIced Coffee100% (4)
- Anatomy and Physiology SLEDocumento27 pagineAnatomy and Physiology SLEMoti Pagador100% (4)
- CellulitisDocumento39 pagineCellulitisMary Jhane Villanueva50% (4)
- Sinew Channels by J Yuen002Documento81 pagineSinew Channels by J Yuen002Jonathan100% (1)
- Lupus, SLEDocumento2 pagineLupus, SLEFrances Anne Pasiliao100% (2)
- Pa Tho Physiology and NCP Lung CancerDocumento2 paginePa Tho Physiology and NCP Lung CancerAlleizarg EuqorNessuna valutazione finora
- Breast Cancer Concept MapDocumento1 paginaBreast Cancer Concept MapKeepItSecret100% (1)
- Vii. Nursing Care Plan: Secretions in The AirwaysDocumento5 pagineVii. Nursing Care Plan: Secretions in The AirwaysJai - Ho100% (2)
- Lung CancerDocumento4 pagineLung CancerKrizia TepootNessuna valutazione finora
- NCP PainDocumento2 pagineNCP PainKarizza Reyes Mamaradlo100% (1)
- Nursing Care Plan Readiness For Enhanced HOPEDocumento3 pagineNursing Care Plan Readiness For Enhanced HOPEMr.GoneNessuna valutazione finora
- Diarrhea Care PlanDocumento2 pagineDiarrhea Care Planzepoli_zepoly6232100% (1)
- NCP - OsteosarcomaDocumento5 pagineNCP - OsteosarcomaNelson Lacsamana100% (1)
- Group 3 Pathophysiology-of-BREAST-CANCERDocumento1 paginaGroup 3 Pathophysiology-of-BREAST-CANCERArisa VijungcoNessuna valutazione finora
- Additional Nursing Care Plans - SchizophreniaDocumento26 pagineAdditional Nursing Care Plans - SchizophreniaJasmin Jacob100% (5)
- NCP BkaDocumento4 pagineNCP BkaKeeshia CesnerosNessuna valutazione finora
- Pathophysiology of Gastrointestinal Bleeding Secondary To Bleeding PolypsDocumento1 paginaPathophysiology of Gastrointestinal Bleeding Secondary To Bleeding PolypsGinoTevesNessuna valutazione finora
- Discharge PlanDocumento2 pagineDischarge PlanRoxanne_Buenaf_5285Nessuna valutazione finora
- Patho Pleural EffusionDocumento2 paginePatho Pleural EffusionJess Prodigo50% (2)
- Nursing Care Plan Process Analysis Planning and ImplementationDocumento2 pagineNursing Care Plan Process Analysis Planning and ImplementationVanessa Prieto100% (2)
- Lung CancerDocumento2 pagineLung CancerCarla Mae Guillermo Navarro50% (2)
- NCP For CTTDocumento1 paginaNCP For CTTJen Rhae LimNessuna valutazione finora
- Cva NCPDocumento2 pagineCva NCPAkima Mulok0% (1)
- NCP PainDocumento2 pagineNCP PainJun TangonanNessuna valutazione finora
- Sle Concept Map Part 1Documento1 paginaSle Concept Map Part 1Vane UcatNessuna valutazione finora
- NCP For Bladder CaDocumento4 pagineNCP For Bladder CaChris Tine CaccamNessuna valutazione finora
- Lung Cancer (Nursing Care)Documento5 pagineLung Cancer (Nursing Care)heiyuNessuna valutazione finora
- Risk For InfectionDocumento5 pagineRisk For InfectionRochelle Corneta JoreNessuna valutazione finora
- Systemic Lupus Erythematosus PathophysiologyDocumento8 pagineSystemic Lupus Erythematosus PathophysiologyAnonymous OU6w8lX9Nessuna valutazione finora
- Lung Cancer Concept Map-Group 2Documento2 pagineLung Cancer Concept Map-Group 2Maria Cristina100% (2)
- NCP Acute Pain RT CancerDocumento3 pagineNCP Acute Pain RT CancerCharissa Magistrado De LeonNessuna valutazione finora
- Ampicillin Sulbactam 1Documento2 pagineAmpicillin Sulbactam 1Queenie Gallardo Angeles100% (1)
- NCP Patient 3 Cervical CADocumento8 pagineNCP Patient 3 Cervical CAFatima LabaoNessuna valutazione finora
- Liver Cancer Pathophysiology: Predisposing FactorDocumento3 pagineLiver Cancer Pathophysiology: Predisposing FactorTarantado100% (2)
- ALL PathophysiologyDocumento2 pagineALL PathophysiologyDeo Michael Rivera LlamasNessuna valutazione finora
- Pathophysiology of AppendicitisDocumento3 paginePathophysiology of AppendicitisArvin Ian Penaflor100% (3)
- Pathophysiology of BREAST CANCERDocumento1 paginaPathophysiology of BREAST CANCEREggy Pascual100% (1)
- NAPREXDocumento2 pagineNAPREXKarl EdemNessuna valutazione finora
- Lupus ErythematosusDocumento5 pagineLupus ErythematosusAditya DarmawanNessuna valutazione finora
- Portofolio SHDocumento22 paginePortofolio SHDini Jatiya AnggrainiNessuna valutazione finora
- Systemic Lupus Erythematosus and Neuropsychiatric DiseaseDocumento56 pagineSystemic Lupus Erythematosus and Neuropsychiatric DiseaseHerry HendrayadiNessuna valutazione finora
- Cornell Notes: TopicDocumento4 pagineCornell Notes: TopicLeahCongrehillaNessuna valutazione finora
- Lupus: Sigit Widyatmoko Fakultas Kedokteran UMSDocumento52 pagineLupus: Sigit Widyatmoko Fakultas Kedokteran UMSAim AimmaNessuna valutazione finora
- Cutaneous Lupus Erythematosus: SGD B3Documento41 pagineCutaneous Lupus Erythematosus: SGD B3Che Haniff100% (2)
- Systemic Lupus Erythematosus: Harrison's ClubDocumento60 pagineSystemic Lupus Erythematosus: Harrison's ClubOrchid Limoso LozanoNessuna valutazione finora
- Referat SLEDocumento24 pagineReferat SLENihayatulHusniaNessuna valutazione finora
- DR - Nadrizal - Sle Dan RaDocumento24 pagineDR - Nadrizal - Sle Dan RaPutri Sari SeptirianiNessuna valutazione finora
- Systemic Lupus Erythematosus - An Overview: - Dr. Parvez KhanDocumento68 pagineSystemic Lupus Erythematosus - An Overview: - Dr. Parvez KhanMohammad Sadiq AzamNessuna valutazione finora
- Histiocytic Disorders Diagnosis and Treatment: Resident Education Lecture SeriesDocumento41 pagineHistiocytic Disorders Diagnosis and Treatment: Resident Education Lecture SeriesChetan SekhriNessuna valutazione finora
- The Good and Bad Effects of TV On ChildrenDocumento4 pagineThe Good and Bad Effects of TV On Childrenapi-206219067100% (1)
- Cardiac Surgery in The Adult - 24-41Documento18 pagineCardiac Surgery in The Adult - 24-41Nicola AlkhorayNessuna valutazione finora
- Frontal Sinus FX Slides 070117Documento48 pagineFrontal Sinus FX Slides 070117Andre WaaniNessuna valutazione finora
- School-Based Play Therapy: Second EditionDocumento12 pagineSchool-Based Play Therapy: Second EditionWuDennisNessuna valutazione finora
- Indicative Term Sheet Bank Islami Pakistan Limited Akbar Chowk Branch, LahoreDocumento6 pagineIndicative Term Sheet Bank Islami Pakistan Limited Akbar Chowk Branch, LahoreSaadatNessuna valutazione finora
- 14 WartsprotocolDocumento9 pagine14 WartsprotocolLakshmi Deepak INessuna valutazione finora
- Alcohol and Drug Abuse Flow ChartDocumento1 paginaAlcohol and Drug Abuse Flow Chartboen jaymeNessuna valutazione finora
- ATI DRUG TABLES Module4 Respiratory Glucocorticoids InhalationDocumento1 paginaATI DRUG TABLES Module4 Respiratory Glucocorticoids InhalationnoeyeshaveseenNessuna valutazione finora
- BIO 100 Discoveries in Biology Lecture:09 Autoimmune DisordersDocumento29 pagineBIO 100 Discoveries in Biology Lecture:09 Autoimmune DisordersIsmail Hossen RajuNessuna valutazione finora
- 04 21 HealthDocumento16 pagine04 21 HealthMoga RazvanNessuna valutazione finora
- Behavior Therapy: Mr. Jayesh PatidarDocumento21 pagineBehavior Therapy: Mr. Jayesh PatidarDr. Jayesh Patidar100% (2)
- 02-HK Products AllDocumento154 pagine02-HK Products AllHari SetiawanNessuna valutazione finora
- Article in Press: Neuroscience and Biobehavioral ReviewsDocumento10 pagineArticle in Press: Neuroscience and Biobehavioral ReviewsSahrul FajarNessuna valutazione finora
- Seminar HD-RSUD Sleman 2019Documento36 pagineSeminar HD-RSUD Sleman 2019herkamaya100% (1)
- Single DentureDocumento37 pagineSingle DentureDentist Dina SamyNessuna valutazione finora
- Topical Steroids (Sep 19) PDFDocumento7 pagineTopical Steroids (Sep 19) PDF1234chocoNessuna valutazione finora
- Mental Health ServicesDocumento6 pagineMental Health Servicesapi-494539289Nessuna valutazione finora
- JCI-Sentinel Event AlertDocumento3 pagineJCI-Sentinel Event AlertDewi Ratna SariNessuna valutazione finora
- Healthy LifestyleDocumento2 pagineHealthy LifestyleEmmalyn Cabillan SereñoNessuna valutazione finora
- Pharm - Chapter - 15 - Antiparkinson DrugsDocumento44 paginePharm - Chapter - 15 - Antiparkinson DrugsFeliciaDorghamNessuna valutazione finora
- Physical Therapy Management of Congenital Muscular.2Documento47 paginePhysical Therapy Management of Congenital Muscular.2Katherine Valeska Sánchez MuñozNessuna valutazione finora
- Gonzales Cannon 2012 Fall Sports PreviewDocumento28 pagineGonzales Cannon 2012 Fall Sports PreviewGonzales CannonNessuna valutazione finora
- Iron Deficiency Anemia 2012Documento41 pagineIron Deficiency Anemia 2012peanadssNessuna valutazione finora
- Dewitt 2007Documento6 pagineDewitt 2007Bagus Putra KurniawanNessuna valutazione finora
- Introduction To Environmental EngineeringDocumento41 pagineIntroduction To Environmental EngineeringPaul Santos NonatNessuna valutazione finora
- Reflexology and DementiaDocumento8 pagineReflexology and DementiaNatalie Stubbs100% (1)
- Drug De-Addiction Programme (DDAP) Ministry of Health and Family Welfare (MOH&FW), Government of IndiaDocumento19 pagineDrug De-Addiction Programme (DDAP) Ministry of Health and Family Welfare (MOH&FW), Government of IndiaHari BabooNessuna valutazione finora
- West Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityDocumento7 pagineWest Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityRegine Marie EspañaNessuna valutazione finora