Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
NCP Ineffective Cerebral Tissue Perfusion
Caricato da
Angelo ︻╦̵̵͇̿̿̿̿╤── BulacanDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
NCP Ineffective Cerebral Tissue Perfusion
Caricato da
Angelo ︻╦̵̵͇̿̿̿̿╤── BulacanCopyright:
Formati disponibili
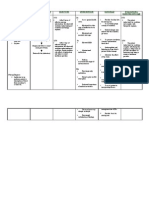
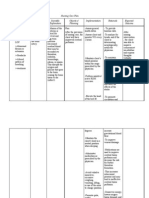
Admitting Diagnosis: Multiple Cerebral Infarction Assessment Subjective The client complained of slight difficulty of breathing Objective - The
patient appears lethargic -P: 8 am 57 bpm 12 pm 57 bpm -BP: 8 am 130/70 12 pm 140/80 -Speech abnormalities: slurred speech -Extremity weakness; pain and discomfort on lower extremities -Restless; Diagnosis Ineffective Cerebral Tissue Perfusion related to interruption of blood flow secondary to multiple cerebral infarctions as manifested by altered level of consciousness , changes in motor & sensory response, and language deficits Planning Goal The client will have an effective cerebral tissue perfusion after 2 to 3 weeks of proper nursing intervention Objectives 1. To assess contribut ing factors 2. To note degree of impairm ent 3. To maximiz e tissue perfusio n Implementation
Determine factors related to individual situation, decreased cerebral perfusion and potential for ICP.
Rationale
Influences choice of interventions. Deterioration in neurological signs and symptoms or failure to improve after initial insult may reflect decreased intracranial adaptive capacity, which requires that client be admitted to critical care area for monitoring of ICP and for specific therapies geared to maintaining ICP within a specified range. If the stroke is evolving, client can deteriorate quickly and require repeated assessment and progressive treatment. If the stroke is completed, the neurological deficit is nonprogressive, and treatment is geared toward rehabilitation and preventing recurrence. Assesses trends in LOC and potential for increased ICP and is useful in determining location, extent, and progression or resolution of CNS damage. Fluctuations in pressure may occur because of cerebral pressure or injury in vasomotor area of the brain. Hypertension or hypotension may have been a precipitating factor. Visual and sensory/motor changes/ involvement indicate safety concerns and influence the
Evaluation After 2-3 weeks of nursing intervention the client will be able to demonstrat e increased perfusionm( e.g., vital signs within normal range, alert/oriente d, free of pain/discom fort)
Monitor and document neurological status frequently and compare with baseline.
Monitor vital signs noting: Hypertens ion or hypotension
Keeps on calling out for his wife and son -facial weakness
Determine the presence of visual, sensory/motor change, headache, dizziness, altered mental status, personality changes Elevate HOB
choice of nursing intervention.
To promote circulation/venous drainage Some medications may be used to decrease edema
Administer medications (e.g. antihypertensives, diuretics)
Maintain bedrest, provide quiet environment, and restrict visitors or activities, as indicated. Provide rest periods between care activities, limiting duration of procedures.
Continual stimulation can increase ICP. Absolute rest and quiet may be needed to prevent recurrence of bleeding, in the case of hemorrhagic stroke.
Prevent straining at stool or holding breath.
Valsalvas maneuver increases ICP and potentiates risk of bleeding. Reduces hypoxemia.
Administer supplemental oxygen, as indicated.
Potrebbero piacerti anche
- Ineffective Cerebral Tissue PerfusionDocumento3 pagineIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- Nursing Care Plans - Ineffective Cerebral Tissue PerfusionDocumento3 pagineNursing Care Plans - Ineffective Cerebral Tissue PerfusionKate Cruz75% (8)
- NCP-Ineffective Cerebral Tissue PerfusionDocumento9 pagineNCP-Ineffective Cerebral Tissue PerfusionKarel LuNessuna valutazione finora
- Ineffective Tissue Perfusion NCPDocumento5 pagineIneffective Tissue Perfusion NCPJasmin Calata50% (2)
- NCP #1 Ineffective Cerebral Tissue PerfusionDocumento4 pagineNCP #1 Ineffective Cerebral Tissue PerfusionsteffiNessuna valutazione finora
- Ineffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Hemorrhage As Evidenced by GCS of 7Documento2 pagineIneffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Hemorrhage As Evidenced by GCS of 7dana100% (4)
- NCP Ineffective Cerebral Tissue Perfusion STROKEDocumento3 pagineNCP Ineffective Cerebral Tissue Perfusion STROKEMa. Elaine Carla TatingNessuna valutazione finora
- NCP 1: Ineffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Cerebrovascular AccidentDocumento14 pagineNCP 1: Ineffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Cerebrovascular AccidentKyle Jingco100% (2)
- NCP - Tissue Perfusion (Cerebral)Documento2 pagineNCP - Tissue Perfusion (Cerebral)moodlayers50% (6)
- CVA Activity IntoleranceDocumento1 paginaCVA Activity IntoleranceNursesLabs.com75% (4)
- Ineffective Tissue PerfusionDocumento1 paginaIneffective Tissue PerfusionRhae RaynogNessuna valutazione finora
- "Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient'sDocumento4 pagine"Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient'sAllisson BeckersNessuna valutazione finora
- NCP For Subarachnoid HemorrhageDocumento4 pagineNCP For Subarachnoid HemorrhageJoan Rose Rendon-Hung78% (18)
- Nursing Care Plan For Acute Head InjuryDocumento4 pagineNursing Care Plan For Acute Head InjuryAngie Mandeoya67% (3)
- NCP Ischemic StrokeDocumento3 pagineNCP Ischemic StrokeLP Benoza100% (3)
- NCP Cva Ineffective Tissue PerfusionDocumento1 paginaNCP Cva Ineffective Tissue Perfusionexcel21121Nessuna valutazione finora
- NCP - Ineffective Cerebral Tissue Perfusion R/T Space Occupying Lesion (Neuroblastoma On Frontal Lobe)Documento4 pagineNCP - Ineffective Cerebral Tissue Perfusion R/T Space Occupying Lesion (Neuroblastoma On Frontal Lobe)Carl Elexer Cuyugan Ano100% (4)
- Nursing Care Plan Hemorrhagic StrokeDocumento8 pagineNursing Care Plan Hemorrhagic StrokeJeffrey Dela Cruz50% (4)
- Nursing Care Plan: by The Wife During InterviewDocumento3 pagineNursing Care Plan: by The Wife During InterviewJayson SamonteNessuna valutazione finora
- NCP CvaDocumento4 pagineNCP CvamannyV1990100% (1)
- NCP For StrokeDocumento4 pagineNCP For StrokeJASON OGALESCONessuna valutazione finora
- Nursing Care Plan CVADocumento4 pagineNursing Care Plan CVAhermesdave175% (4)
- NCP Ineffective Tissue PerfusionDocumento2 pagineNCP Ineffective Tissue PerfusionRhoel John Bartolome92% (13)
- CVA NCPDocumento6 pagineCVA NCPErika Arboleras0% (1)
- NCP - Acute PainDocumento3 pagineNCP - Acute PainErine Emmanuelle Cawaling Hetrosa100% (1)
- III. Nursing Care Plan: Assessment Diagnosis Goal Intervention EvaluationDocumento4 pagineIII. Nursing Care Plan: Assessment Diagnosis Goal Intervention EvaluationSTEPHANIE JOSUENessuna valutazione finora
- Risk For Ineffective Tissue PerfusionDocumento5 pagineRisk For Ineffective Tissue PerfusionElle Oranza100% (1)
- Ineffective Tissue PerfusionDocumento2 pagineIneffective Tissue Perfusioniammkrissa33% (3)
- Nursing Care Plan SeizureDocumento2 pagineNursing Care Plan Seizuretimie_reyes100% (1)
- Decreased Cardiac Output Nursing Care PlanDocumento4 pagineDecreased Cardiac Output Nursing Care Planjudssalangsang86% (7)
- NCP - Decreased Intracranial Adaptive Capacity R/T Space - Occupying Lesion.Documento1 paginaNCP - Decreased Intracranial Adaptive Capacity R/T Space - Occupying Lesion.Carl Elexer Cuyugan Ano100% (6)
- Impaired Physical MobilityDocumento2 pagineImpaired Physical MobilityVhin Lim100% (2)
- Assessment Nursing Diagnosis Scientific Explanation Goal of Care Intervention Rationale EvaluationDocumento4 pagineAssessment Nursing Diagnosis Scientific Explanation Goal of Care Intervention Rationale EvaluationHowel CristobalNessuna valutazione finora
- NCP - Altered Tissue PerfusionDocumento2 pagineNCP - Altered Tissue PerfusionLeigh Kristel Andrion0% (1)
- Impaired Verbal CommunicationDocumento3 pagineImpaired Verbal CommunicationChenee Mabulay100% (1)
- Nursing Care PlanDocumento9 pagineNursing Care PlanJam AbantaoNessuna valutazione finora
- NCP For CVADocumento18 pagineNCP For CVAmolukas101100% (7)
- Decreased Cardiac OutputDocumento3 pagineDecreased Cardiac OutputTiffany Mathis100% (1)
- CVA-NCPDocumento7 pagineCVA-NCPAiza Oronce0% (1)
- Disturbed Sensory PerceptionDocumento2 pagineDisturbed Sensory Perceptionsuper ahga-once0% (1)
- Ineffective Tissue PerfusionDocumento1 paginaIneffective Tissue PerfusionEm Castillo50% (2)
- NCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)Documento2 pagineNCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)yanny0350% (2)
- NCP Ineffective Tissue PerfusionDocumento4 pagineNCP Ineffective Tissue PerfusionKristine Maghari83% (6)
- Transient Ischemic Attack: A Case StudyDocumento44 pagineTransient Ischemic Attack: A Case Studytinay100% (8)
- Nursing Care Plan Ineffective Tissue PerfusionDocumento1 paginaNursing Care Plan Ineffective Tissue Perfusionderic83% (29)
- Tissue PerfusionDocumento2 pagineTissue PerfusionMichael John LeandichoNessuna valutazione finora
- NCP 2 TrixieDocumento1 paginaNCP 2 TrixieMajkel Benche CustodioNessuna valutazione finora
- Pathophysiology of HydrocephalusDocumento8 paginePathophysiology of HydrocephalusAlden MendozaNessuna valutazione finora
- NCP CaseDocumento35 pagineNCP Caselicservernoida100% (1)
- Shortans QDocumento4 pagineShortans QJeff ZhouNessuna valutazione finora
- ScriptDocumento12 pagineScriptTrishia Nhicole HoNessuna valutazione finora
- NCP HeadDocumento11 pagineNCP Headann-lisel-manahan-7670100% (2)
- NCPDocumento3 pagineNCPKrizelle Abadesco Libo-on50% (2)
- NCP of CavDocumento3 pagineNCP of CavHenry Roque TagalagNessuna valutazione finora
- Ineffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)Documento6 pagineIneffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)Alba ArjunNessuna valutazione finora
- Ncps TetanyDocumento18 pagineNcps TetanyBob Joyce Dela PeñaNessuna valutazione finora
- NCP For CHF 3 Activity IntoleranceDocumento2 pagineNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNessuna valutazione finora
- Ineffective Tissue PerfusionDocumento3 pagineIneffective Tissue PerfusionStephanie Louisse Gallega Hisole100% (2)
- Traumatic Neurologic InjuriesDocumento27 pagineTraumatic Neurologic InjuriesDorothee GumisadNessuna valutazione finora
- NCM 118L/ 119L (Related Learning Experience) Day 3-ActivityDocumento4 pagineNCM 118L/ 119L (Related Learning Experience) Day 3-ActivityNicole Villanueva, BSN - Level 3ANessuna valutazione finora
- Motion of A Simple Pendulum in A FluidDocumento16 pagineMotion of A Simple Pendulum in A FluidGokul JeevaNessuna valutazione finora
- Geology and Mineralization of The Maggie Creek DistrictDocumento28 pagineGeology and Mineralization of The Maggie Creek DistrictRockstone Research Ltd.Nessuna valutazione finora
- An Overview of The IEEE Color BooksDocumento6 pagineAn Overview of The IEEE Color BooksOhm666Nessuna valutazione finora
- Production System: BY: Mallick MD Fahad Roll No. 16Documento36 pagineProduction System: BY: Mallick MD Fahad Roll No. 16Fahad SailorNessuna valutazione finora
- Biomaterials in Restorative Dentistry and Endodontics: An OverviewDocumento6 pagineBiomaterials in Restorative Dentistry and Endodontics: An Overviewmanzoor ul haq bukhariNessuna valutazione finora
- VIP45Documento92 pagineVIP45Román IsraelNessuna valutazione finora
- DLP MonsoonDocumento2 pagineDLP MonsoonjennifertariaoNessuna valutazione finora
- One - Touch Fittings: Series: WP2Documento12 pagineOne - Touch Fittings: Series: WP2PrashantNessuna valutazione finora
- Quran On GeologyDocumento10 pagineQuran On GeologyMM NabeelNessuna valutazione finora
- Academic Program Required Recommended Academic Program Required RecommendedDocumento1 paginaAcademic Program Required Recommended Academic Program Required Recommendedonur scribdNessuna valutazione finora
- Ground PlaneDocumento1 paginaGround Planeaeronautical rajasNessuna valutazione finora
- Consent For Diagnostic And/or Therapeutic ParacentesisDocumento2 pagineConsent For Diagnostic And/or Therapeutic ParacentesisnaveenNessuna valutazione finora
- Biology Unit 4Documento44 pagineBiology Unit 4Mohammad KhanNessuna valutazione finora
- 9 Daftar Pustaka VaricelaDocumento2 pagine9 Daftar Pustaka VaricelaAfrina FaziraNessuna valutazione finora
- Manual Bomba HLXDocumento16 pagineManual Bomba HLXVictor Manuel Hernandez GomezNessuna valutazione finora
- Power - Distribution Transformers @2020V2Documento34 paginePower - Distribution Transformers @2020V2Musfiqul AzadNessuna valutazione finora
- The Church of Kapnikarea in Athens - N. GkiolesDocumento13 pagineThe Church of Kapnikarea in Athens - N. GkiolesMaronasNessuna valutazione finora
- TamasDocumento180 pagineTamaslike 2Nessuna valutazione finora
- Book 1Documento1 paginaBook 1PES SAFETYNessuna valutazione finora
- Sander Protein SkimmersDocumento18 pagineSander Protein Skimmerslleimicojon100% (1)
- MalachiteDocumento2 pagineMalachiteAkhil KumarNessuna valutazione finora
- Electro-Mechanical SectorDocumento22 pagineElectro-Mechanical SectorKen LeeNessuna valutazione finora
- Manual For Noncommissioned Officers and Privates of Infantry of The Army of The United StatesDocumento250 pagineManual For Noncommissioned Officers and Privates of Infantry of The Army of The United StatesGutenberg.org100% (1)
- Emcoturn 365Documento362 pagineEmcoturn 365mikadoturkNessuna valutazione finora
- MHT-CET 2021 Question Paper: 25 September 2021Documento3 pagineMHT-CET 2021 Question Paper: 25 September 2021Sank DamNessuna valutazione finora
- Q3 Module 15Documento33 pagineQ3 Module 15jovielyn kathley manaloNessuna valutazione finora
- 159 SnackDocumento97 pagine159 SnackGuy PlaterNessuna valutazione finora
- RA No. 9514 Revised Fire CodeDocumento11 pagineRA No. 9514 Revised Fire Coderaegab100% (32)
- Bar Tending TerminologyDocumento3 pagineBar Tending TerminologySiska WangNessuna valutazione finora
- API 571 Quick ReviewDocumento32 pagineAPI 571 Quick ReviewMahmoud Hagag100% (1)