Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Drug Cards
Caricato da
Michael LongsDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Drug Cards
Caricato da
Michael LongsCopyright:
Formati disponibili
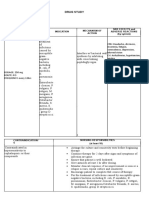
Oxycodone/Acetaminophen (Percocet, Endocet, Magnacet, Primalev, Roxicet, Roxilox, Tylox)
Classification: Opioid agonists, opioid agonists/nonopioid analgesic combinations
Schedule II drug/ Controlled substance must be locked up and counted before dispensing
Indication: Management of moderate to severe pain (give patients pain info)
Contraindications: (Do not give) If hypersensitivity to oxycodone/acetaminophen, Severe Hepatic/Renal disease,
OB, Lactation Use Cautiously: Head trauma, increased intracranial pressure, severe renal, hepatic pulmonary disease
Dosage Range: Oxycodone: PO Adults more than or equal to 50kg) 5-10 mg q 3-4 hr prn | PO Adults less than 50kg
or Children 6-12yr 1.25mg q6hr prn or 0.2mg/kg q3-4hr prn| PO children >12: 2.5mg q6hr prn | Rectally(Adults):
10-40mg 3-4 times daily prn
Available as: (Know which dose you are giving according to MD order)
Percocet 2.5/325 Percocet 5/325 Percocet 7.5/325 Percocet 7.5/500 Percocet 10/325 Percocet 10/650
Major Side Effects: Oxycodone: CNS: confusion, sedation, dizziness, dysphoria, euphoria, floating feeling,
hallucinations, headache, unusual dreams EENT: blurred vision, diplopia, miosis Respiratory Depression CV:
orthostatic hypotension GI: constipation, dry mouth, nausea, vomiting GU: urinary retention Skin: flushing,
sweating Misc: Physical/psychological dependence, tolerance
APAP Side Effects: Hepatic failure, Hepatotoxicity, renal failure (high doses) (4 G/ Day)
Nursing Implications: (Information Specific to your Patient) Always check for allergies
Assessment: assess type, location, and intensity of pain prior to and 1hr after administration.
ASESS: BP/ Pulse/ and Respirations before and periodically during admin.
Hold If respiratory rate is <10/min assess level of sedation ; Physical stimulation may be sufficient to prevent
significant hypoventilation. Assess bowel function routinely. Prevention of constipation should be instituted with
increased intake of fluids and bulk, and laxatives to minimize constipating effects. Stimulant laxatives should be
administered routinely if opioid use exceeds 2-3 days, unless contraindicated
LAB test: may increase plasma amylase and lipase levels.
Oxycodone/Aspirin (Percodan, Endodan)
Classification: Opioid agonists/ nonopioid analgesic combination
Schedule II drug/ Controlled substance ( must be locked up and counted before dispensing)
Indication: Management of moderate to severe pain (give pt pain info)
Contraindications: (Do not give) If hypersensitivity to oxycodone/aspirin, tartrazine, or other salicylates. Bleeding
disorders or thrombocytopenia. Children or adolescents w/ viral infections (reye’s syndrome) Severe Hepatic/Renal
disease, OB, Lactation Use Cautiously: Head trauma, increased intracranial pressure, severe renal, hepatic
pulmonary disease
Dosage Range: Oxycodone: PO Adults more than or equal to 50kg) 5-10 mg q 3-4 hr prn / PO Adults less than
50kg or Children 6-12yr 1.25mg q6hr prn or 0.2mg/kg q3-4hr prn / PO children >12: 2.5mg q6hr prn
Rectally(Adults): 10-40mg 3-4 times daily prn / Aspirin: do not exceed 4g/day
Available As: (know which dose you are giving according to MD order) 4.88mg oxycodone + 325mg
Major Side Effects: Oxycodone: CNS: confusion, sedation, dizziness, dysphoria, euphoria, floating feeling,
hallucinations, headache, unusual dreams EENT: blurred vision, diplopia, miosis Respiratory Depression CV:
orthostatic hypotension GI: constipation, dry mouth, nausea, vomiting GU: urinary retention Skin: flushing,
sweating Misc: Physical/psychological dependence, tolerance
Aspirin: GI: GI bleeding dyspepsia, epigastric distresss, nausea, abdominal pain, anorexia hepatotoxicity, vomiting
Exfoliative dermatitis, stevens-johnson syndrome, toxic epidermal necrolysis, anemia, hemolysis, increased
bleeding time
Nursing Implications: (Information Specific to your Patient) Always check for allergies.
Assessment: assess type, location, and intensity of pain prior to and 1hr after administration.
ASESS: BP/ Pulse/ and Respirations before and periodically during admin.
Hold If respiratory rate is <10/min assess level of sedation ; Physical stimulation may be sufficient to prevent
significant hypoventilation. Assess bowel function routinely. Prevention of constipation should be instituted with
increased intake of fluids and bulk, and laxatives to minimize constipating effects. Stimulant laxatives should be
administered routinely if opioid use exceeds 2-3 days, unless contraindicated
LAB test: may increase plasma amylase and lipase levels.
Omeprezole (Prilosec, Prilosec OTC) Classification: proton-pump inhibitors
Indication: GERD/maintenance of healing in erosive esophagitis. Duodenal ulcers (w/ or w/o anti-infectives for
Helicobacter pylori) Short term treatment of active benign gastric ulcer. Pathologic hypersecretory
conditions(Zollinger-Ellison syndrome) Reduction of risk of GI bleeding in critically ill pts. OTC: Heartburn
occurring more or equal to twice/week.
Dosage Range: PO(Adults): GERD/erosive esophagitis 20mg once daily. Duodenal ulcers ass. w/ H. Pylori 40mg
once daily in the morning w/ clarithromycin for 2wk then 20mg daily for 2wk or 20 mg twice daily w/
clarithromycin 500mg twice daily and amoxicillin 1000mg twice daily for 10 days(if ulcer present at beginning of
therapy, continue omeprazole 20 mg daily for 18 more days) gastric ulcer 40mg 1x/day for 4-6 wk.
PO (Children 1-16yr and 5-9kg) GERD 5mg daily PO (Children 1-16yr and 10-19kg): GERD 10mg 1x/day
PO (Children 1-16yr and equal to or more than 20kg) 20mg/day
Major Side Effects: CNS: dizziness, drowsiness, fatigue, headache, weakness CV: chest pain GI: abdominal pain,
acid regurgitation, constipation, diarrhea, flatulence, nausea, vomiting Skin: itching, rash Misc: allergic reactions.
Nursing Implications: Assess pt. routinely for epigastric or abdominal pain and frank or accult blood in the stool,
emesis, or gastric aspirate LAB Test: Monitor CBC w/ differential periodically during therapy, may increase AST,
ALT, alkaline phosphatase and bilrubin, may cause serum gastrin concentrations to increase first 1-2wk of therapy.
Monitor INR and prothrombin time in pt’s taking warfarin.
Give before meals preferable in the morning. Do not crush/chew capsule. Capsules may be sprinkled on cool
applesauce (ingest immediately & drink water) (do not store for future use)
Mylanta II, DS- Magnesium Hydroxide/aluminum hydroxide (Alamag, Gaviscon, Simethicone, Maalox, Mylanta
DS)
Classification: Antiacids
Indication: useful in a variety of GI complaints, including Hyperacidity, Indigestion, GERD, Heartburn,
excess gas (simethicone) (helps belching/ passing flatus)
Contraindications: (Do not give) severe abdominal pain of unknown cause, especially if accompanied by
fever; renal failure, (CrCl <30 ml/min)
Dosage Range: Magnesium/Aluminum Hydroxide: PO Adults & Children >12 yr 5-10ml or 1-2 tabs 1-3 hr
after meals and at bedtime.
Major Side Effects: GI: Constipation, diarrhea, hypermagnesemia, hypophosphatemia
Nursing Implications: Assess for heartburn and indigestion as well as location, duration, character, and
precipitating factors of gastric pain
LAB Test Considerations: Monitor Serum phosphate, potassium, and calcium levels periodically during
chronic use. May cause increased serum calcium and decreased serum phosphate concentrations
Potrebbero piacerti anche
- Drug Study ColestipolDocumento3 pagineDrug Study ColestipolAbby AngNessuna valutazione finora
- MorphineDocumento1 paginaMorphineCassie100% (3)
- CEPHALOSPORINSDocumento18 pagineCEPHALOSPORINSVikas SharmaNessuna valutazione finora
- DRUG STUDY - Docx Grand CaseDocumento10 pagineDRUG STUDY - Docx Grand CaseAntonette PereyraNessuna valutazione finora
- Ketessee FCT Dexketoprofen Jul 2012Documento8 pagineKetessee FCT Dexketoprofen Jul 2012Dhurai OnelyNessuna valutazione finora
- DRUGS Study OrigDocumento17 pagineDRUGS Study OrigKiersten Karen Policarpio Verina100% (1)
- Drug Study - CaseDocumento9 pagineDrug Study - CaseMay EvelynNessuna valutazione finora
- NCP & Drug Study (Tondo Med)Documento5 pagineNCP & Drug Study (Tondo Med)Kevin_Remollo_2431Nessuna valutazione finora
- Docusate Sodium (Colace)Documento2 pagineDocusate Sodium (Colace)E100% (1)
- Drug Study - AmlodipineDocumento1 paginaDrug Study - AmlodipineDanielle Marie SamblacenoNessuna valutazione finora
- DS (Calcium + Vit. D)Documento6 pagineDS (Calcium + Vit. D)Mary April MendezNessuna valutazione finora
- Combizar Drug StudyDocumento6 pagineCombizar Drug StudymrnmrsllNessuna valutazione finora
- Brand Name: Generic Name: Drug ClassificationDocumento2 pagineBrand Name: Generic Name: Drug ClassificationChristine Pialan SalimbagatNessuna valutazione finora
- SalbutamolDocumento1 paginaSalbutamolFranz Ervas BinasNessuna valutazione finora
- Sennosides (Senokot)Documento1 paginaSennosides (Senokot)E100% (1)
- Drug MetronidazoleDocumento1 paginaDrug MetronidazoleSrkocherNessuna valutazione finora
- Generic NameDocumento2 pagineGeneric NamePerdie Branden ReizNessuna valutazione finora
- Chloral Hydrate (Drug Study)Documento3 pagineChloral Hydrate (Drug Study)Franz.thenurse6888Nessuna valutazione finora
- Activity 6 - Drug StudyDocumento14 pagineActivity 6 - Drug StudyAl-Mujib TanogNessuna valutazione finora
- Methyldopa, Losartan K, Ascorbic AcidDocumento4 pagineMethyldopa, Losartan K, Ascorbic AcidRico Mae ValenciaNessuna valutazione finora
- Bisacodyl (Dulcolax)Documento1 paginaBisacodyl (Dulcolax)ENessuna valutazione finora
- Atropine Sulfate Indications: Adverse Effects: CNS: Headache, Ataxia, Contraindication: Assessment & Drug EffectsDocumento4 pagineAtropine Sulfate Indications: Adverse Effects: CNS: Headache, Ataxia, Contraindication: Assessment & Drug EffectsMarie Kris Chua AbelleraNessuna valutazione finora
- Bisacodyl DulcolaxDocumento1 paginaBisacodyl DulcolaxENessuna valutazione finora
- Pregabalin An Anticonvulsant DrugDocumento2 paginePregabalin An Anticonvulsant DrugmeimeiliuNessuna valutazione finora
- Famotidine (Pepcid)Documento1 paginaFamotidine (Pepcid)E100% (1)
- Duphaston PDFDocumento4 pagineDuphaston PDFmarcusjanaNessuna valutazione finora
- PlasilDocumento1 paginaPlasilernestjohnNessuna valutazione finora
- LortabDocumento1 paginaLortabSheri490Nessuna valutazione finora
- SalmeterolDocumento2 pagineSalmeterolapi-3797941Nessuna valutazione finora
- Cefazolin (Ancef)Documento1 paginaCefazolin (Ancef)Adrianne BazoNessuna valutazione finora
- COLCHICINE pptx1800128929Documento15 pagineCOLCHICINE pptx1800128929April Mergelle LapuzNessuna valutazione finora
- SalbutamolDocumento2 pagineSalbutamolMarck Vincent Garcia OngNessuna valutazione finora
- New DS3Documento3 pagineNew DS3dakieNessuna valutazione finora
- Irbesartan (Avapro)Documento1 paginaIrbesartan (Avapro)ENessuna valutazione finora
- Drug StudyDocumento3 pagineDrug StudyStephannie MirandaNessuna valutazione finora
- Tramadol, Paracetamol, Calmoseptine, B12Documento5 pagineTramadol, Paracetamol, Calmoseptine, B12Denise EspinosaNessuna valutazione finora
- DuphalacDocumento2 pagineDuphalacianecunarNessuna valutazione finora
- Drug PrilosecDocumento1 paginaDrug PrilosecSrkocher100% (1)
- Lopressor (Metoprolol) IVDocumento2 pagineLopressor (Metoprolol) IVAdrianne Bazo100% (1)
- IBSDocumento1 paginaIBSIris MambuayNessuna valutazione finora
- Drug Card PradaxaDocumento2 pagineDrug Card PradaxaBen0% (1)
- Antimalarial DrugsDocumento7 pagineAntimalarial DrugsHilmanNessuna valutazione finora
- AnastrozoleDocumento2 pagineAnastrozoleAnonymous FgT04krgymNessuna valutazione finora
- AmbroxolDocumento1 paginaAmbroxolPrecious CarmelaNessuna valutazione finora
- ETOPOSIDEDocumento4 pagineETOPOSIDEkajal guptaNessuna valutazione finora
- Dynastat: What Is in This LeafletDocumento4 pagineDynastat: What Is in This LeafletBenj GilbuenaNessuna valutazione finora
- Drug Study FinalDocumento5 pagineDrug Study FinalJackie Ann Marie DapatNessuna valutazione finora
- Drug StudyDocumento2 pagineDrug StudyAlesandra MocorroNessuna valutazione finora
- Alendronate SodiumDocumento3 pagineAlendronate SodiumGLen Caniedo100% (1)
- ARCOXIADocumento22 pagineARCOXIATeresa JunioNessuna valutazione finora
- Drug Card SennaDocumento1 paginaDrug Card SennaAdrianne Bazo100% (1)
- Methylprednisolone Solu MedrolDocumento1 paginaMethylprednisolone Solu MedrolTrixie_Anne_Jh_9038Nessuna valutazione finora
- DrugmedsDocumento52 pagineDrugmedsshirleyNessuna valutazione finora
- Medications: Medication Name Generic/Trade Classification Pregnancy CategoryDocumento8 pagineMedications: Medication Name Generic/Trade Classification Pregnancy CategoryapalestiNessuna valutazione finora
- Drug StudyDocumento13 pagineDrug StudyClarkEstacioNessuna valutazione finora
- Assignment: ON AntilipidemicsDocumento15 pagineAssignment: ON AntilipidemicsMansi DabolaNessuna valutazione finora
- Generic Name: Acetaminophen Brand Name: Tylenol: ActionDocumento22 pagineGeneric Name: Acetaminophen Brand Name: Tylenol: Actionp_dawg100% (14)
- Lovenox Anticoagulant Prevent Thrombus Formation: VTE Prophylaxis Following Abdominal Surgery - 40Documento8 pagineLovenox Anticoagulant Prevent Thrombus Formation: VTE Prophylaxis Following Abdominal Surgery - 40Joanie BNessuna valutazione finora
- ATORVASTATINDocumento2 pagineATORVASTATINAubrey Unique EvangelistaNessuna valutazione finora
- Icu Drug StudyDocumento7 pagineIcu Drug StudyHazel Palomares100% (1)
- Paeds EMQDocumento8 paginePaeds EMQfasdNessuna valutazione finora
- Clinicals ENTDocumento70 pagineClinicals ENTMarrow Pg42Nessuna valutazione finora
- Hyperthyroidism in Cats: Typical Clinical SignsDocumento5 pagineHyperthyroidism in Cats: Typical Clinical Signscarteparte100% (1)
- Fibrinolytic DisordersDocumento29 pagineFibrinolytic DisordersChelly JimenoNessuna valutazione finora
- UROLITHIASISDocumento84 pagineUROLITHIASISJheanAlphonsineT.MeansNessuna valutazione finora
- Case Report: Systemic Lupus ErythematosusDocumento32 pagineCase Report: Systemic Lupus ErythematosusdesmyyNessuna valutazione finora
- MIND DietDocumento21 pagineMIND DietFrank Lavilla100% (3)
- Stroke Scale NIHSS PDFDocumento4 pagineStroke Scale NIHSS PDFFilipa Figueiredo100% (1)
- Atlas de Enfermedades Maculares de GASSDocumento1.357 pagineAtlas de Enfermedades Maculares de GASSNidia M. Quispe RodríguezNessuna valutazione finora
- Glomerulonephritis - Symptoms and Causes - Mayo ClinicDocumento6 pagineGlomerulonephritis - Symptoms and Causes - Mayo ClinicUmi Khoirun NNessuna valutazione finora
- Kulit Emergency in DermatologyDocumento47 pagineKulit Emergency in DermatologyAulia Shabrina SyukharialNessuna valutazione finora
- General PhysiotherapyDocumento6 pagineGeneral Physiotherapysomebody_maNessuna valutazione finora
- Physiology Cardiovascular Physiology NotesDocumento13 paginePhysiology Cardiovascular Physiology Noteshedayatamin44Nessuna valutazione finora
- Diagnose Non SpesialistikDocumento12 pagineDiagnose Non SpesialistikMufthie PerdanaNessuna valutazione finora
- Ouabain - The Optimal Solution For The Problem of Myocardial InfarctionDocumento20 pagineOuabain - The Optimal Solution For The Problem of Myocardial InfarctionredsbooksNessuna valutazione finora
- T WaveDocumento15 pagineT WaveKay BristolNessuna valutazione finora
- Approach To Child With Fever: Liew Qian YiDocumento33 pagineApproach To Child With Fever: Liew Qian YinavenNessuna valutazione finora
- School of Health and Allied Health Sciences Nursing Department Self-Directed Learning (Nur 146 - Clinical Area)Documento5 pagineSchool of Health and Allied Health Sciences Nursing Department Self-Directed Learning (Nur 146 - Clinical Area)Milagros FloritaNessuna valutazione finora
- Multiple-Choice QuizDocumento6 pagineMultiple-Choice QuizHUAWEI HUAWEI100% (1)
- Ujian Journal Reading PPT Laringofaringeal RefluxDocumento25 pagineUjian Journal Reading PPT Laringofaringeal RefluxAlmira PutriNessuna valutazione finora
- Protein-Protein Interaction Analysis of Alzheimer's Disease and NAFLD Based On Systems Biology Methods Unhide Common Ancestor PathwaysDocumento7 pagineProtein-Protein Interaction Analysis of Alzheimer's Disease and NAFLD Based On Systems Biology Methods Unhide Common Ancestor PathwaysRicardo CastilloNessuna valutazione finora
- Dysphagia: - Dr. Arjun SainiDocumento80 pagineDysphagia: - Dr. Arjun SainiArjun SainiNessuna valutazione finora
- Core Knowledge OrthopaedicsDocumento2 pagineCore Knowledge OrthopaedicsIamTineshNessuna valutazione finora
- Medical-Surgical Nursing Exam 18 - Neurological Disorders (34 Items) - NurseslabsDocumento7 pagineMedical-Surgical Nursing Exam 18 - Neurological Disorders (34 Items) - NurseslabsRandySandoval100% (1)
- Patient M. G Drug 1 - Ob MaxDocumento5 paginePatient M. G Drug 1 - Ob MaxGrace MellaineNessuna valutazione finora
- Drug StudyDocumento7 pagineDrug StudySophia Rose Delos SantosNessuna valutazione finora
- Inflammation Digestive Tract Ileum Small Intestine Stomach: Crohn Disease Regional Enteritis Regional IleitisDocumento10 pagineInflammation Digestive Tract Ileum Small Intestine Stomach: Crohn Disease Regional Enteritis Regional IleitisOlivia BakerNessuna valutazione finora
- (WR) Group 2 - Ward Work 4Documento9 pagine(WR) Group 2 - Ward Work 4Rodrigo Joseph PaysonNessuna valutazione finora
- Jurnal Patologi AnatomiDocumento5 pagineJurnal Patologi Anatomiafiqzakieilhami11Nessuna valutazione finora
- Fundamentals of Pathology PathomaDocumento215 pagineFundamentals of Pathology Pathomaprachi jainNessuna valutazione finora
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Valutazione: 3 su 5 stelle3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 4.5 su 5 stelle4.5/5 (82)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (32)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 4 su 5 stelle4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDa EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesValutazione: 4.5 su 5 stelle4.5/5 (1412)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceDa EverandTo Explain the World: The Discovery of Modern ScienceValutazione: 3.5 su 5 stelle3.5/5 (51)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (46)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (60)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (328)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4.5 su 5 stelle4.5/5 (6)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingDa EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingValutazione: 1 su 5 stelle1/5 (1)