Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Team Nursing
Caricato da
sagami.gCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Team Nursing
Caricato da
sagami.gCopyright:
Formati disponibili
Brief History
During World War II, multilevel training programs were developed to teach auxiliary
personnel how to perform simple care and technical procedures. In the military, these trained
workers were called corpsmen. Outside of the military, there were 1- year programs developed to
teach technical nursing care. On- the- job training programs were established to produce what
would today be called nursing assistance. The model of the team nursing was developed after
war in an effort to utilize these trained workers and to ease the shortage of nurses that most
hospitals were experiencing and decrease the problems associated with the functional
organization of patient care. Many believed that despite the continued shortage of professional
nursing staff, a patient care system had to be developed that reduce the fragmented care that
accompanied functional nursing.
Description
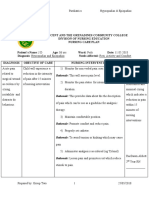
- Team nursing is a care delivery model that assigns staff to teams that then are responsible
for a group of patients. A unit may be divided into two teams, and each team is led by a
registered nurse.
- team leader supervises and coordinates all the care provided by those on his team. The
team is most commonly made up LPNs and UAP, but occasionally there is another RN.
Charge Nurse RN
RN RN
Team leader Team leader
RN LPN RN LPN
UAP UAP
15 Patients 15 Patients
Team Nursing Model (Heidenthal, 2003)
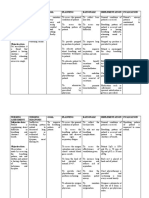
Charge Nurse
Nursing Staff
Nursing Staff
Nursing Staff
Nursing Staff
Nursing Staff
Nursing Staff
Patients/Clients
Patients/Clients
Patients/Clients
Team Nursing Model ( Marquis,2003)
- the nurse is responsible for knowing the condition and deeds of all the patients assigned
to the team and for planning individual care. The team leader’s duties vary depending on
the patient’s needs and the workload. These duties may include assisting team members,
giving direct personal care to patients, teaching, and coordinating patient activities.
- care is divided into the simplest components and then assigned to the appropriate care
provider.
- aside from supervision duties, the team leader also is responsible for providing
professional direction to those on his team regarding the care provided.
Through extensive team communication, comprehensive care can be provided for
patients despite a relatively high proportion of ancillary staff. This communication occurs
informally between the team leader and the individual team members and formally through
regular team planning conferences. A team should consist of not more than five people or it will
revert to more functional lines of organization.
Modular Nursing Delivery System
- is a kind of team nursing that divides a geographic space into modules of patient with
each module cared for by a team of staff led by an RN. The modules may vary in size,
but typically there is one RN with an LPN and nursing assistant to make up the team. In
this case, the RN is responsible for the overall care of the patient in her module.
- team nursing, as originally design, has undergone much modification in the last 25 years.
Most team nursing was never practiced in its purest form but was instead a combination
of team and functional structure. Recent attempts to refine and improve team nursing
have resulted in the concept of “modular nursing”, which is mini-team (two or three
members) approach.
- keeping the team small and attempting to assign personnel to the same team as often as
possible should allow the professional nurse more time for planning and coordinating
team members.
- smaller team requires less communication, allowing members better use of their time for
direct patient care activities.
Advantages and Disadvantages of Team Nursing
Team nursing allows members to contribute their own special expertise or skills. Team
leaders, then, should use their knowledge about each member’s abilities when making patient
assignments. Recognizing the individual worth of all employees and giving team members
autonomy result in high job satisfaction.
In team nursing and modular nursing, the RN is able to get work done through others, but
patients often receive fragmented, depersonalized care. Communication in these models is
complex. There is shared responsibility and accountability, which can cause confusion and lack
of accountability. These factors contribute to RN dissatisfaction with these models. These
models required the RN to have very good delegation and supervision skills.
Team nursing is usually associated with democratic leadership. Group members are given
as much autonomy as possible when performing assigned task, although the team shares
responsibility and accountability collectively. The need for excellent communication and
coordination skills makes implementing team nursing difficult and requires great self-discipline
on the part of the team members.
Disadvantages to team nursing are associated primarily with improper implementation
rather than with the philosophy itself. Frequently, insufficient time is allowed for team care
planning and communication. This can lead to blurred lines of responsibility, errors, and
fragmented patient care. For team nursing to be effective, the leader must have a good
communication, organizational, management, and leadership skills must be an excellent
practitioner.
References:
Heidenthal, Patricia Kelly. NURSING LEADERSHIP AND MANAGEMENT. 4th Edition.
Thomson Delmar Pte, LTD. 5 Shenton Way #01-01 UIC Building, Singapore. ©2003. p.
255-256.
Marquis, Bessie L. and Huston, Carol J. LEADERSHIP ROLES AND MANAGEMENT
FUNCTIONS IN NURSING: THEORY AND APPLICATION. 4th Edition. Lippincott
Williams & Wilkins. Philadelphia, U. S. A. © 2003. p. 213-214.
Potrebbero piacerti anche
- Team NursingDocumento4 pagineTeam NursingDawn NavarroNessuna valutazione finora
- Pregnancy Induced Hypertension Nursing Diagnosis NANDADocumento9 paginePregnancy Induced Hypertension Nursing Diagnosis NANDASanal S SalimNessuna valutazione finora
- StaffdevelopmentprogrammeDocumento43 pagineStaffdevelopmentprogrammeketaki maity100% (1)
- Nursing Care PlanDocumento3 pagineNursing Care PlanSophia Loraine Dorone Jesura100% (1)
- NCP Fever 1Documento11 pagineNCP Fever 1Deepak VermaNessuna valutazione finora
- Case Presentation On Parkinsonism 4th YearDocumento27 pagineCase Presentation On Parkinsonism 4th YearArchanaNessuna valutazione finora
- Birth AsphyxiaDocumento2 pagineBirth AsphyxiaTeslim Raji100% (3)
- Primary Nursing Care .Documento6 paginePrimary Nursing Care .Patel Amee100% (1)
- Unit2 Health Care Delivery SystemDocumento43 pagineUnit2 Health Care Delivery Systemprincess100% (2)
- Nursing Care Plan HyperthyroidismDocumento2 pagineNursing Care Plan HyperthyroidismAbdallah Alasal0% (1)
- Family Health Nursing: Ms - Neethu Vincent Asst Professor KVM College of NursingDocumento9 pagineFamily Health Nursing: Ms - Neethu Vincent Asst Professor KVM College of NursingNeethu VincentNessuna valutazione finora
- Effectiveness of Planned Teaching Programme On Knowledge Regarding Needle Stick Injury Among The Staff NursesDocumento3 pagineEffectiveness of Planned Teaching Programme On Knowledge Regarding Needle Stick Injury Among The Staff NursesInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Spina Bifida NCPDocumento3 pagineSpina Bifida NCPCarpz Darpz100% (2)
- Bronchial Asthma: Islamic University Nursing CollegeDocumento27 pagineBronchial Asthma: Islamic University Nursing CollegeRenuka SivaramNessuna valutazione finora
- Time Specific Objective Content Teachin G Learning Activity Av Aids EvaluationDocumento7 pagineTime Specific Objective Content Teachin G Learning Activity Av Aids Evaluationrittika dasNessuna valutazione finora
- Terminology CHNDocumento4 pagineTerminology CHNKailash NagarNessuna valutazione finora
- Skill 11 (1) ..Collection of Stool SpecimenDocumento1 paginaSkill 11 (1) ..Collection of Stool SpecimennetsquadNessuna valutazione finora
- Trends and Issues in Nursing PracticeDocumento2 pagineTrends and Issues in Nursing PracticeVanesa Guillano100% (1)
- Care of The Client With Pulmonary Tuberculosis Utilizing Orem's TheoryDocumento13 pagineCare of The Client With Pulmonary Tuberculosis Utilizing Orem's TheoryRazel Kinette AzotesNessuna valutazione finora
- Nicu Lesson PlanDocumento11 pagineNicu Lesson PlanSAYMABANUNessuna valutazione finora
- E-Learning, Telemadicin, Tele Nursing AssignmentDocumento22 pagineE-Learning, Telemadicin, Tele Nursing AssignmentBhawna Joshi100% (2)
- C12 P13 TubectomyDocumento24 pagineC12 P13 TubectomyRaviKurleNessuna valutazione finora
- Role of The Head NurseDocumento12 pagineRole of The Head Nurseمحمود على ما تفرج75% (4)
- Clinical Presentation TonsilectomyDocumento46 pagineClinical Presentation TonsilectomySREEDEVI T SURESH100% (1)
- Rationale: This Will Assess Pain LevelDocumento7 pagineRationale: This Will Assess Pain LevelCoreyNessuna valutazione finora
- Cva NCP AnxietyDocumento1 paginaCva NCP AnxietyQueenElsaDeVeraNessuna valutazione finora
- Seminar On DirectingDocumento22 pagineSeminar On DirectingChinchu MohanNessuna valutazione finora
- Schizophrenia Nursing ManagementDocumento56 pagineSchizophrenia Nursing ManagementHumphreyNessuna valutazione finora
- Conducting Normal DeliveryDocumento3 pagineConducting Normal DeliveryNishaThakuriNessuna valutazione finora
- Total Abdominal Hysterectomy Actual NCPDocumento1 paginaTotal Abdominal Hysterectomy Actual NCPDoreen ClaireNessuna valutazione finora
- Av AidsDocumento10 pagineAv AidsMadhu Bala100% (1)
- Nursing Care Plan of MeningitisDocumento2 pagineNursing Care Plan of MeningitisŦỏṯặ Łaẕỗzą100% (7)
- 11 Nursing Care PlansDocumento4 pagine11 Nursing Care Planseknok03Nessuna valutazione finora
- Drug Study ON Cabergolin EDocumento4 pagineDrug Study ON Cabergolin ESimran SimzNessuna valutazione finora
- The Incident ReportDocumento4 pagineThe Incident ReportJay PaulNessuna valutazione finora
- Problem Solving Approach Topic WordDocumento20 pagineProblem Solving Approach Topic Wordvani reddyNessuna valutazione finora
- Shoulder DystociaDocumento7 pagineShoulder DystociaYwagar YwagarNessuna valutazione finora
- NCPDocumento3 pagineNCPJerome Vergel RubianesNessuna valutazione finora
- Ocd First 3 PageDocumento5 pagineOcd First 3 Pagevikas takNessuna valutazione finora
- Chapter 004Documento21 pagineChapter 004HannaNessuna valutazione finora
- Session 8 Ethical Dilemma in Professional PracticeDocumento14 pagineSession 8 Ethical Dilemma in Professional PracticeSyed MaazNessuna valutazione finora
- Nursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDocumento5 pagineNursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDimpal Choudhary100% (1)
- Prepared By: Athulya G Ii Year MSC Nursing Upasana College of Nursing KollamDocumento25 paginePrepared By: Athulya G Ii Year MSC Nursing Upasana College of Nursing KollamGayathri RNessuna valutazione finora
- Staffing Pattern Old NewDocumento5 pagineStaffing Pattern Old NewsrinivasanaNessuna valutazione finora
- Code of Ethics and Professional ConductDocumento4 pagineCode of Ethics and Professional ConductMrs. Deepak100% (1)
- File1-Role of Nurse in EpidemiologyDocumento14 pagineFile1-Role of Nurse in EpidemiologyRufus Raj83% (23)
- Assignment On Staffing Pattern of Nursing Education Sub: Nursing ManagementDocumento6 pagineAssignment On Staffing Pattern of Nursing Education Sub: Nursing ManagementPrity DeviNessuna valutazione finora
- Nursing Care PlansDocumento6 pagineNursing Care PlansJhessa Curie PitaganNessuna valutazione finora
- Income Capital ItemsDocumento2 pagineIncome Capital ItemsDeepti KukretiNessuna valutazione finora
- Seminar Topic - Job Description of Departmental SisterDocumento18 pagineSeminar Topic - Job Description of Departmental Sistershubham rathod0% (1)
- Group DynamicsDocumento21 pagineGroup DynamicsPandiyan Dhyan100% (1)
- Application of Orem TheoryDocumento17 pagineApplication of Orem TheoryKit LaraNessuna valutazione finora
- A Descriptive Study To Assess The Knowledge and Practice Regarding Adverse Effects of Excessive Use of Mobile Phones Among Nursing Students of Selected Nursing College of BagalkotDocumento8 pagineA Descriptive Study To Assess The Knowledge and Practice Regarding Adverse Effects of Excessive Use of Mobile Phones Among Nursing Students of Selected Nursing College of BagalkotAnonymous izrFWiQNessuna valutazione finora
- Structured Teaching Programme On Prevention of Ventilator Associated PneumoniaDocumento15 pagineStructured Teaching Programme On Prevention of Ventilator Associated PneumoniaSagiraju Srinu100% (1)
- Hospital OrientationDocumento82 pagineHospital OrientationDondee Pamposa100% (2)
- Independent Nurse Practice ANPDocumento12 pagineIndependent Nurse Practice ANPSamjhana Neupane50% (2)
- 2 NCM119 A Patient Care Delivery System Sept. 2 2021Documento6 pagine2 NCM119 A Patient Care Delivery System Sept. 2 2021Ghianx Carlox PioquintoxNessuna valutazione finora
- What Is The Team Nursing Model?Documento3 pagineWhat Is The Team Nursing Model?Sofia LopezNessuna valutazione finora
- AssigmentDocumento51 pagineAssigmenthalayehiahNessuna valutazione finora
- Mod Ali Ties of Nursing CareDocumento2 pagineMod Ali Ties of Nursing CareTintin AbalosNessuna valutazione finora
- Transcultural Nursing and SpecializationDocumento3 pagineTranscultural Nursing and Specializationsagami.gNessuna valutazione finora
- Membership in Professional Organization, Personal Image Building, Self-Governance, Independent Nursing Practice, Evidence-Based Practice, Nurse EntrepreneurDocumento18 pagineMembership in Professional Organization, Personal Image Building, Self-Governance, Independent Nursing Practice, Evidence-Based Practice, Nurse Entrepreneursagami.gNessuna valutazione finora
- Contemporary Nursing TheoriesDocumento13 pagineContemporary Nursing Theoriessagami.gNessuna valutazione finora
- Research: Its Nature, Types and Role in DevelopmentDocumento7 pagineResearch: Its Nature, Types and Role in Developmentsagami.g92% (24)
- PsychopharmacologyDocumento7 paginePsychopharmacologysagami.gNessuna valutazione finora
- Traditional Teaching Strategies - LecturingDocumento8 pagineTraditional Teaching Strategies - Lecturingsagami.g100% (2)
- Psych NSG Sample QuestionsDocumento7 paginePsych NSG Sample Questionspaul100% (8)
- Code of Ethics For Filipino NursesDocumento2 pagineCode of Ethics For Filipino NursesJessica Christel MaglalangNessuna valutazione finora
- Orientation of The Registered Nurses and Cetified Surgical Technologist To The Perioperative SettingDocumento6 pagineOrientation of The Registered Nurses and Cetified Surgical Technologist To The Perioperative SettingRudy DuterteNessuna valutazione finora
- Brochure Nursing Science2018Documento8 pagineBrochure Nursing Science2018YashantiniSugintharanYashaNessuna valutazione finora
- Professional Scope of Nursing Midwifery Practice March 2019Documento4 pagineProfessional Scope of Nursing Midwifery Practice March 2019dianaNessuna valutazione finora
- Doh DC 2018-0288Documento8 pagineDoh DC 2018-0288MenGuitarNessuna valutazione finora
- Curriculum Vitae - Carla CarnesDocumento2 pagineCurriculum Vitae - Carla Carnesccarnes2Nessuna valutazione finora
- Nursing and Midwifery Board Candidate Handbook RN OSCE ExaminationDocumento25 pagineNursing and Midwifery Board Candidate Handbook RN OSCE ExaminationkemalayazNessuna valutazione finora
- Alex Alas MSN, Agcns: 6285 Andersen Mills Heights - 336-837-7183Documento3 pagineAlex Alas MSN, Agcns: 6285 Andersen Mills Heights - 336-837-7183api-700587394Nessuna valutazione finora
- Assignment and Delegation Guidelines: For Registered Nurses and Licensed Practical NursesDocumento20 pagineAssignment and Delegation Guidelines: For Registered Nurses and Licensed Practical Nursesanna regarNessuna valutazione finora
- NSP II Project Directors Meeting 2017 NSP II Update: Peg Daw (MHEC) Oscar Ibarra (HSCRC)Documento37 pagineNSP II Project Directors Meeting 2017 NSP II Update: Peg Daw (MHEC) Oscar Ibarra (HSCRC)KyleRhayneDiazCaliwagNessuna valutazione finora
- Expedited Licensing Process For Nurses Licensed in Designated Jurisdictions FAQDocumento5 pagineExpedited Licensing Process For Nurses Licensed in Designated Jurisdictions FAQVimal KumarNessuna valutazione finora
- Assignment of PatientsDocumento39 pagineAssignment of PatientsStephy Sojan100% (1)
- Iv AnsapDocumento7 pagineIv AnsapromeojrNessuna valutazione finora
- Nursing Practice IDocumento7 pagineNursing Practice IFaustine Salas100% (5)
- Resume2 Updated FinalDocumento3 pagineResume2 Updated Finalapi-527335577Nessuna valutazione finora
- NU RN Endorsement ApplicationDocumento7 pagineNU RN Endorsement ApplicationannealisangcoNessuna valutazione finora
- Nursing Opportunities AbroadDocumento133 pagineNursing Opportunities Abroadrandz c thinksNessuna valutazione finora
- Resume 1Documento3 pagineResume 1g_who19Nessuna valutazione finora
- 2010 NCLEX RN Detailed Test Plan EducatorDocumento68 pagine2010 NCLEX RN Detailed Test Plan Educatorshamy143Nessuna valutazione finora
- Test Taking StrategiesDocumento6 pagineTest Taking Strategiestmanare100% (1)
- Iv FormatDocumento1 paginaIv Formatinvictus0446Nessuna valutazione finora
- Nurs 250 Assignment 1Documento6 pagineNurs 250 Assignment 1api-325441744Nessuna valutazione finora
- Nursing PhilosophyDocumento5 pagineNursing Philosophyapi-532524779Nessuna valutazione finora
- Philippine Nursing Act of 2002 RevisedDocumento77 paginePhilippine Nursing Act of 2002 RevisedDave Misman100% (1)
- Your Connection - Summer2016Documento9 pagineYour Connection - Summer2016Ken KnickerbockerNessuna valutazione finora
- RN HealsDocumento2 pagineRN HealsDianne MacaraigNessuna valutazione finora
- Resume - Alanna SteeleDocumento4 pagineResume - Alanna Steeleapi-280544985Nessuna valutazione finora
- MSN Clinical HandbookDocumento34 pagineMSN Clinical HandbookJoYCeNessuna valutazione finora
- XVIII Q 10.00a Staffing Contingency Plan Template UADocumento11 pagineXVIII Q 10.00a Staffing Contingency Plan Template UAJomares SueltoNessuna valutazione finora
- PRC Cord DressingDocumento2 paginePRC Cord DressingMike Royzkie RodriguezNessuna valutazione finora
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (24)
- The Millionaire Fastlane: Crack the Code to Wealth and Live Rich for a LifetimeDa EverandThe Millionaire Fastlane: Crack the Code to Wealth and Live Rich for a LifetimeValutazione: 4.5 su 5 stelle4.5/5 (2)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- Summary of Noah Kagan's Million Dollar WeekendDa EverandSummary of Noah Kagan's Million Dollar WeekendValutazione: 5 su 5 stelle5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Summary: The 5AM Club: Own Your Morning. Elevate Your Life. by Robin Sharma: Key Takeaways, Summary & AnalysisDa EverandSummary: The 5AM Club: Own Your Morning. Elevate Your Life. by Robin Sharma: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (22)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Coaching Habit: Say Less, Ask More & Change the Way You Lead ForeverDa EverandThe Coaching Habit: Say Less, Ask More & Change the Way You Lead ForeverValutazione: 4.5 su 5 stelle4.5/5 (186)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDa EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningValutazione: 4 su 5 stelle4/5 (3)
- Gut: the new and revised Sunday Times bestsellerDa EverandGut: the new and revised Sunday Times bestsellerValutazione: 4 su 5 stelle4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosDa Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosValutazione: 4.5 su 5 stelle4.5/5 (207)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (44)