Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Journal Reading The Drowning Index
Caricato da
Yuliasminde SofyanaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Journal Reading The Drowning Index
Caricato da
Yuliasminde SofyanaCopyright:
Formati disponibili
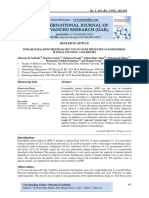
J Forensic Sci, March 2014, Vol. 59, No.
2
doi: 10.1111/1556-4029.12356
Available online at: onlinelibrary.wiley.com
PAPER
PATHOLOGY/BIOLOGY
Khalil S. Wardak,1 M.D.; Robert M. Buchsbaum,1,* M.D., J.D.; and Frozan Walyzada1
The Drowning Index: Implementation in
Drowning, Mechanical Asphyxia, and Acute
Myocardial Infarct Cases
ABSTRACT: Drowning is a diagnosis of exclusion based on circumstantial and autopsy correlation. Sugimura proposed a threshold value of
14.1 for the Drowning Index (DI), the ratio of lung and pleural fluid to spleen weight, as a surrogate marker to diagnose drowning. We questioned the use of DI in diagnosing drowning. We compared DI between three groupsdrowning, mechanical asphyxia, and myocardial infarct
seen at Broward MEO from 2008 to 2009. Only 9.4% of 53 drownings exceeded the DI threshold of 14.1, while 30% of 10 mechanical asphyxias and 40% of 10 myocardial infarcts had DI >14.1. Sensitivity for the DI test was <10% and specificity 6070%. Median DI values for
all groups were <10. MannWhitney U-test was not statistically significant between groups. The DI is neither sensitive nor specific and lacks
any utility in the diagnosis of drowning.
KEYWORDS: forensic science, drowning, drowning index, cause of death, asphyxia, myocardial infarct
In November 2009, Legal Medicine published an article by
Sugimura et al. (1) in which the Drowning Index (DI) was
applied to victims of drowning to show the DI in that group was
higher than for those dying of an acute cardiac event or mechanical asphyxia. The authors suggested the use of a ROC-generated
optimum DI threshold value of 14.1. Their paper was in
response to a paper that was put out by Nishitani et al. in 2005:
Weight ratio of the lungs and pleural effusion to the spleen in
the diagnosis of drowning. Nishitani asserted that an accurate
and reliable method of diagnosing death by drowning is an
important requirement in forensic autopsies (2). The Nishitani
study compared the ratio between the weight of the lungs and
pleural effusion to the weight of the spleen. The authors found
statistically significant intergroup differences in calculated DI
values between drowning, cardiac events, and asphyxia.
Drowning describes submersion resulting in death. The
asphyxia of drowning is usually due to aspiration of fluid, but it
may result from airway obstruction caused by laryngeal spasm
while the victim is gasping under water. Dry drowning is the
mechanism of drowning in which the victim develops laryngeal
spasm after the first gulp and never aspirates fluid, accounting
for 1020 percent of submersion deaths. As laryngeal spasm is a
functional effect that cannot be proven at autopsy, there has been
some controversy in the literature about whether or not the entity
of dry drowning actually exists, with the alternate view being
that these may be a subset of cardiac related deaths (3). More
1
Broward County Medical Examiner and Trauma Services, 5301 S.W.
31st Avenue, Fort Lauderdale, FL 33312, USA.
*
Present address: Philadelphia Medical Examiners Office, 321 University
Ave., Philadelphia, PA 19104, USA.
Received 20 Sept. 2012; and in revised form 23 Jan. 2013; accepted 3
Feb. 2013.
2014 American Academy of Forensic Sciences
commonly, wet drowning occurs in which water is aspirated
into the lungs. The result is either washout dilution of pulmonary
surfactant in freshwater drowning, or the production of an osmotic gradient in saltwater drowning, followed by ventilation/perfusion mismatch, hypoxia, and asphyxia (4,5).
Despite the cause of death, thoracic cavity fluid identified in
decomposing bodies exhibiting the appearance of pleural effusion when brought to autopsy after a postmortem interval greater
than 1 week is called postmortem decomposition fluid. The
occurrence of pleural effusion accompanying drowning, near
drowning, or during prolonged hospitalization following a near
drowning has not been demonstrated in the peer review literature
as one of the typical features of drowning or one of the standard
clinical management concerns.
For near drowning victims, current clinical practice includes
not only complete evaluation for associated trauma, but a minimum of 24 h of inpatient monitoring to detect abnormalities that
may arise in blood gases, pH, and renal and metabolic function.
Sequelae of near drowning such as the onset of pulmonary edema
may take up to a full day to manifest itself, and there may be later
pulmonary sequelae such as pneumonitis and atelectasis, so that
serial chest radiology is a necessary follow-up measure (6).
In protocols that manage hospitalized victims of near drowning, pleural effusion is not among their primary concerns. Of
those who survive a near drowning, majority of them are permanently disabled due to ischemic encephalopathy. However,
drowning victims do not have enough time to develop a pleural
effusion prior to their demise. Consequently, the characterization
of thoracic fluid at autopsy in a drowning victim with decomposition artifacts due to a week or longer postmortem time interval
as a pleural effusion is inaccurate and potentially misleading,
especially when used in an index based in part on the weight of
such fluids.
399
400
JOURNAL OF FORENSIC SCIENCES
Drowning is the ultimate cause of death in live bodies that are
submerged in water. Forensic autopsies of possible drowning
victims ought to answer questions regarding the victims preexisting medical condition or whether the victim was alive or
dead prior to becoming submerged.
Commonly seen autopsy findings of a drowning victim after
excluding blunt and sharp force injuries, gunshot wounds, boating injury such as propeller wounds, and dangerous aquatic life
are skin changes due to the effect of water, a white or rusty
brown foam issuing from the nose, hyperinflated lungs, and
buildup of fluid in the sphenoid sinuses (7). Central vein congestion and right ventricle dilatation are also common findings.
In this study, we analyzed the reproducibility of the Drowning
Index (DI). We retrospectively reviewed autopsy protocols that
listed drowning as a primary cause of death for 2008 and
2009 at the Broward County Medical Examiner and Trauma Services Division and compared this to other groups with causes of
death similar to those in the prior studies.
Methods
Study Design and Subjects
We went through all the cases that were determined to be
drowning from 2008 and 2009 and calculated the DI. We took
the total weight of the lungs and divided it by the weight of the
spleen. The autopsy reports made no mention of any pleural
effusions. Those identified with thoracic cavity fluids had more
than 2 weeks postmortem interval; therefore, those cases were
excluded from the study. For this study, we defined our confirmed drowning group of cases as deaths in which the decedent was either witnessed to become submerged under water, or
if unwitnessed, the body was found in the vicinity of water with
circumstances suggesting a drowning had occurred; in this group
of cases, all other causes of death were excluded at autopsy. At
Broward MEO, there was a total of 95 confirmed drownings in
2008 and 2009. To use the DI, those who did not have a spleen
and those with tissue or organ donation were excluded. We also
excluded any cases with a postmortem interval >2 weeks, leaving
us with 53 drowning victims, 39 men and 14 women. We did not
separate cases for statistical study based on gender or age.
We also selected for comparison with drowning two other
groups with diagnostic features similar to those used in Sugimuras study, namely all deaths due to mechanical asphyxia (primarily manual strangulation cases) and randomly selected
sudden cardiac deaths due to acute myocardial infarcts. These
latter two groups were subject to the same rules of exclusion
as used for the drowning group. This left us with 10 cases
of mechanical asphyxia and 10 cases of acute myocardial infarct.
Results
The goal of this study was to determine to what extent Sugimuras DI threshold test value of 14.1 was useful by seeing how
many cases in each group met their criteria for the diagnosis of
drowning. After calculating the DI of all the victims in the
drowning group (Table 1), we found that 5 of 53 cases (9.4%)
had DI values greater than 14.1, while the remaining 48 cases
(90.6%) had DI of less than 14.1. The probability for a drowning case to be reflected accurately by a DI exceeding the threshold value of 14.1 advanced by Sugimurathe sensitivity of the
testby the calculation for DI was 0.094. Conversely, the probability for a nondrowning case, such as mechanical asphyxia
(Table 2) to be reflected accurately by a DI lower than the
threshold value of 14.1the specificity of the testwas 0.70,
while the specificity of an acute myocardial infarct case was
0.60 (Table 3).
The MannWhitney U-test (also known as the Wilcoxon Rank
Sum test), a nonparametric statistic for comparing medians
between two subject groups at a time, was applied between pairs
of subject groupsdrowning versus mechanical asphyxia,
drowning versus acute myocardial infarct, and mechanical
asphyxia versus acute myocardial infarctto test the null
hypothesis of no difference between pairs of groups. (Table 4)
The MannWhitney U-test value of 308 for drowning versus
mechanical asphyxia gave a 2-tailed p value of 0.43039, not significant at the 0.05 p level. The MannWhitney U-test value of
264 for drowning versus acute myocardial infarct gave a 2-tailed
p value of 0.993372, not significant at the 0.05 p level. The
MannWhitney U-test value of 43 for mechanical asphyxia versus acute myocardial infarct gave a 2-tailed p value of 0.630528,
not significant at the 0.05 p level. Thus, all three comparisons of
pairs of groups were unable to reject the null hypothesis, suggesting there is no statistically significant DI difference between
the three decedent groups. (Table 4)
In addition, inspection of the medians for the three groups
showed that all three groups had median DI considerably below
two-thirds or less the value ofthe DI threshold value of 14.1
proposed by Sugimuras study. This suggests that any intrinsic
differences that might exist between the three groups do not
translate into a DI value that would be useful in discriminating
between deaths due to drowning and deaths due to other causes.
In fact, the median DI score for the drowning group8.00
was less than the median DI score for the mechanical asphyxia
group, at 9.38, suggesting DI scores would likely be higher in
the latter group for any given case. The DI median for the acute
myocardial infarct group, at 6.76, was only a little below that of
the other two groups, suggesting there is no utility in using the
DI to tell these three groups apart by the threshold criteria suggested in Sugimuras study.
Discussion
Drowning is a diagnosis of exclusion. There are signs that one
can see but they are not always present in each case. Foam from
the mouth and nose, mud or other debris in the mouth or nares,
hyperinflated lungs, water in the respiratory sinuses, and wrinkled/macerate/sloughed skin are all nonspecific indications that,
while not pathognomonic for drowning, can be used to help support the interpretive conclusion that the cause of death was due
to drowning (8). In addition, other soft signs that may support
the diagnosis of drowning include engorged central veins and
acute dilatation of the right ventricle of the heart.
The congestion of visceral organs is a nonspecific finding.
Diatoms in the lungs or in organs, in some corners still argued
to be a hallmark of drowning, are considered a nonspecific finding. Tests for diatoms are also not considered to be sufficiently
sensitive (9,10). There is still currently some advocacy for using
diatoms in conjunction with autopsy findings as a possible better
method of diagnosing drowning than the use of autopsy findings
alone, but this view is not universal (11).
Decomposed bodies can generally show lungs that are dark
red, and there may also be a dark red decomposition fluid that
accumulates in the pleural cavity due to transudation out of the
water-filled lungs. The weight of visceral organs varies among
individuals and can vary with disease conditions.
WARDAK AND BUCHSBAUM
THE DROWNING INDEX
401
TABLE 1Drowning victims organ weights and DI values (N = 53).
Case
Age/Sex
Right Lung
Weight (grams)
Left Lung
Weight (grams)
Total Lung
Weight (grams)
Pleural
Fluid (ml)
Spleen
Weight (grams)
DI Test
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
356
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
30/M
48/F
78/M
86/M
90/M
20/M
48/M
88/M
22/M
55/M
68/M
74/F
25/M
66/M
17/M
19/M
41/M
41/M
23/M
19/F
49/M
30/M
61/M
51/M
57/F
69/F
68/M
91/F
46/M
81/F
51/M
54/M
58/F
76/M
59/M
52/F
49/M
60/F
59/M
47/F
37/M
47/M
17/M
41/M
94/M
71/F
29/F
80/M
75/M
47/M
16/F
52/M
29/M
610
700
240
620
760
870
730
600
1000
580
710
360
490
750
630
700
610
920
350
410
1170
920
720
540
460
650
440
360
590
620
580
780
880
560
340
850
670
730
560
960
700
1120
820
910
400
350
840
460
690
770
540
1060
570
460
670
510
490
660
860
680
470
830
450
810
310
480
720
590
640
590
780
340
370
770
830
740
420
390
470
360
350
680
500
460
650
770
490
290
650
350
640
540
810
650
1000
710
1130
460
290
740
370
610
730
550
1070
530
1070
1370
750
1110
1420
1730
1410
1070
1830
1030
1520
670
970
1470
1220
1340
1220
1700
690
780
1940
1750
1460
960
850
1120
800
710
1270
1120
1040
1430
1650
1050
630
1500
1020
1370
1100
1770
1350
2120
1530
2040
860
640
1580
830
1300
1500
1090
2130
1100
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
50
200
120
180
60
150
260
160
130
120
300
80
150
180
100
100
160
290
90
170
280
160
110
90
200
110
100
130
230
90
210
220
170
180
80
100
40
120
110
350
120
260
180
90
80
80
200
90
250
230
310
180
150
21.40
6.85
6.25
6.17
23.67
11.53
5.42
66.9
14.08
8.58
5.07
8.38
6.47
8.17
12.20
13.40
7.50
5.86
7.67
4.59
6.93
10.94
13.27
10.67
4.25
10.18
8.00
5.46
5.52
12.44
4.95
6.50
9.71
5.83
7.88
15.00
25.50
11.42
10.00
5.06
11.25
8.15
8.50
22.67
10.75
8.00
7.90
9.22
5.20
6.52
3.52
11.83
7.33
Other Findings
Decomposed
HACVD
HACVD
FMIL
HACVD
Decomposed
HACVD, hypertensive atherosclerotic cardiovascular disease; FMIL, foreign matter in lung.
TABLE 2Mechanical asphyxia victims organ weights and DI values (N = 53).
Case
1
2
3
4
5
6
7
8
9
10
Case Age/Sex
Right Lung
Weight (grams)
Left Lung
Weight (grams)
Total Lung
Weight (grams)
Pleural
Fluid(ml)
Spleen
Weight (grams)
DI Test
49/F
87/F
47/F
48/M
54/F
43/M
71/F
75/F
65/F
37/M
570
540
340
810
550
330
830
690
600
760
500
440
400
760
400
320
680
570
420
560
1070
980
740
1570
950
650
1510
1260
1020
1320
0
0
0
0
0
0
0
0
0
0
130
150
340
290
550
160
80
180
65
60
8.23
6.53
2.18
5.41
1.73
4.06
18.88
7.00
15.69
22.00
Other
Findings
402
JOURNAL OF FORENSIC SCIENCES
TABLE 3Acute myocardial infarct victims organ weights and DI values (N = 10).
Case
Case Age/Sex
Right Lung
Weight (grams)
Left Lung
Weight (grams)
Total Lung
Weight (grams)
Pleural
Fluid (ml)
Spleen
Weight (grams)
DI Test
64/M
47/F
67/F
50/M
44/M
58/M
30/M
64/M
57/M
78/M
590
670
780
1140
630
630
640
450
1050
460
630
700
510
1130
590
490
620
590
890
470
1220
1370
1290
2270
1220
1120
1260
1040
1940
930
0
0
200
0
0
0
0
0
0
0
150
90
140
130
230
200
230
300
90
60
8.13
15.22
10.64
17.46
5.30
5.60
5.48
3.47
21.56
15.50
1
2
3
4
5
6
7
8
9
10
Other
Findings
TABLE 4Statistical comparisons of 3 decedent groups DI values.
Parameter
Drowning Group
Mechanical Asphyxia Group
Acute Myocardial Infarct Group
N
DI median
DI range
D vs MA
MWU
p value
significance
MA vs AMI
MWU
p value
significance
AMI vs D
MWU
p value
significance
53
8.00
3.5225.50
10
9.38
1.7322.0
10
6.76
3.4721.56
308
0.43039
Not significant at 0.05 p level
43
0.630528
Not significant at 0.05 p level
264
0.993372
Not significant at 0.05 p level
DI, drowning index test result; D, drowning group; MA, mechanical asphyxia group; AMI, acute myocardial infarct group; MWU, MannWhitney U-test
raw score.
p value, two-tailed p level for which a significant statistical result rejecting the null hypothesis is p < 0.05.
There are natural disease processes that could result in heavy,
congested lungs, such as heart failure, bronchopneumonia,
chronic bronchitis, and/or cystic fibrosis. Some conditions can
result in hyperinflated but normally weighted lungs, such as
bronchial asthma, drug overdose, pneumothorax, and/or emphysema, in addition to being found in some drowning cases.
Reasons other than drowning that could result in splenomegaly
include infections such as tuberculosis, infectious mononucleosis,
hepatitis, syphilis, and subacute bacterial endocarditis; anemias
such as thalassemia, the earlier phases of sickle cell disease, and
hereditary spherocytosis; myeloproliferative diseases and leukemias; metabolic storage disorders; and miscellaneous other diseases such as systemic lupus erythematosus, cirrhosis of the
liver, amyloidosis, and sarcoidosis.
Reasons that a spleen may be underweight include the later
phases of sickle cell disease. There is also some evidence that
ulcerative colitis can be associated with a small spleen. Therefore, the spleen is an unreliable organ to be utilized as the
denominator in the calculation of the DI.
Pleural effusion is not one of the recognized, characteristic
findings in a drowning and/or a near drowning victim. The cessation of hydrostatic pressure after death ensues within a short
time period following the loss of consciousness. In fact, in the
absence of hydrostatic pressure, the onset of pleural effusion is
rare to impossible.
In fresh water drowning, after surfactant washout, the water is
rapidly absorbed, diluting the plasma and causing intravascular
hemolysis. In salt water drowning as may occur in the oceans,
water is markedly hypertonic and the resultant osmotic gradient
draws fluid from the vascular system into the lungs, decreasing
plasma volume. Although differences in the osmotic fluid concentration between drowning in fresh water versus salt water can
impact a victims condition if the victim survives, nevertheless,
either type of watery medium would not generate a pleural effusion.
In Nishitanis initial study using DI, with a threshold DI value
not stated but apparently close to 20 from the graphs shown in
that study, DI was considered to be a valuable indicator of the
diagnosis of drowning. Likewise, the subsequent study by Sugimura found a DI threshold of 14.1 to be a valuable indicator
of the diagnosis of drowning when compared to 47 cases of
mechanical asphyxia and 42 cases of acute cardiac death.
We selected 10 cases from Broward MEOs database for
20082009 with the immediate cause of death mechanical
asphyxia and 10 other cases with the immediate cause of death
acute myocardial infarct and applied the DI formula to each of
these cases in turn. We found that 3 of the 10 cases of mechanical asphyxia met the criteria for drowning suggested by Sugimuras study, although none of the victims were recovered
from a body of water. Four of 10 cases of acute myocardial
infarct met the DI threshold criteria suggested by Sugimuras
study for drowning; microscopic review of these 10 cases
revealed compelling signs of acute cardiac death although none
of the victims in this group had been recovered from a body of
water.
WARDAK AND BUCHSBAUM
Conclusion
Drowning is a form of asphyxia caused by immersion, usually
in water. It is a diagnosis of exclusion for which circumstantial
information is vital. In this study, we analyzed the utility of the
drowning index (DI) in 53 confirmed drowning cases, for which
other causes of death were ruled out after a complete scene
investigation and a complete autopsy. We applied the drowning
index formula to 10 cases of sudden cardiac death by acute
myocardial infarct and 10 cases of mechanical asphyxia. The
sensitivity of the DI to confirm a case of drowning is very low
as the probability of diagnosing a drowning victim by the use of
this index is only 0.094. Regarding specificity, the probability of a
victim of mechanical asphyxia to be mislabeled as a drowning in a
scenario if the decedent were to be recovered from a body of water
would be 0.3, giving this test a specificity of only 0.70. Likewise,
the probability of a victim of an acute myocardial infarct to be mislabeled as a victim of drowning if the body were recovered from a
body of water would be 0.4, giving it a specificity of only 0.60. As
the sensitivity and specificity of the DI threshold are poor, DI is of
no value in the autopsy workup of a suspected drowning case.
Therefore, we cannot recommend it as an adjunct or surrogate
method for confirming, or diagnosing, drowning cases.
References
1. Sugimura T, Kashiwagi M, Matsusue A, Hara K, Kaguera M, Kubo S-I.
Application of the drowning index to actual drowning cases. Leg Med
(Tokyo) 2010;12(2):6872.
THE DROWNING INDEX
403
2. Nishitani Y, Fujii K, Okazaki S, Imabayashi K, Matsumoto H. Weight
ratio of the lungs and pleural effusion to the spleen in the diagnosis of
drowning. Leg Med (Tokyo) 2006;8(1):227.
3. Modell JH, Bellefleur M, Davis JH. Drowning without aspiration: is this
an appropriate diagnosis? J Forensic Sci 1999;44:111923.
4. Moore S. Drowning. Medscape; http://emedicine.medscape.com/article/
772753.
5. Edmonds C. Drowning syndromes: the mechanism. SPUMS J 1998;28
(1):19.
6. Nemer JA. Disorders related to environmental factors: near drowning. In:
McPhee SJ, Papadakis MA, Rabow MW, editors. Current medical
diagnosis and treatment, 51st edn. New York, NY: McGraw-Hill,
2012;1513.
7. Bell MD. Drowning. In: Dolinak D, Matshes EW, Lew EO, editors.
Forensic pathology: principles and practice. Burlington, MA: Elsevier,
2005;22737.
8. Spitz DJ. Investigation of bodies in water. In: Spitz WU, editor. Spitz
and Fischers medicolegal investigation of death, 4th edn. Springfield,
IL: Charles Thomas, 2006; 84679.
9. DiMaio VJ, DiMaio D. Forensic pathology, 2nd edn. Boca Raton, FL:
CRC Press, 2001.
10. DiMaio VJM, Dana SE. Handbook of forensic pathology, 2nd edn. Boca
Raton, FL: CRC Press, 2007.
11. Piette MH, DeLetter EA. Drowning: still a difficult diagnosis. Forensic
Sci Int 2006;162(12):19.
Additional information and reprint requests:
Khalil S. Wardak, M.D.
Associate Medical Examiner
Broward County Office of Medical Examiner and Trauma Services
5301 SW 31st Avenue
Fort Lauderdale, FL 33312, USA
E-mail: kwardak@broward.org
Potrebbero piacerti anche
- Jurnal ForensikDocumento15 pagineJurnal ForensikZoehelmy HusenNessuna valutazione finora
- Shock Management, by Ayman RawehDocumento15 pagineShock Management, by Ayman RawehaymxNessuna valutazione finora
- Tokyo Guidelines 2018 Diagnostic Criteria and Seve6706321783624012310Documento15 pagineTokyo Guidelines 2018 Diagnostic Criteria and Seve6706321783624012310Katrina bangaoetNessuna valutazione finora
- HerniaDocumento61 pagineHerniaAhmed HassanNessuna valutazione finora
- Ivc InjuryDocumento17 pagineIvc InjuryAnishChowdhuryNessuna valutazione finora
- Hernia World Conference ProgramDocumento112 pagineHernia World Conference ProgramYovan Prakosa100% (1)
- (Upgraded) BDH6 - Emergency Trauma & Non Trauma UroDocumento122 pagine(Upgraded) BDH6 - Emergency Trauma & Non Trauma Uronabila safiraNessuna valutazione finora
- Emergensi Urologi UiiDocumento83 pagineEmergensi Urologi UiitrianaamaliaNessuna valutazione finora
- Pembahasan UKDI CLINIC 3 Batch Mei 2016Documento662 paginePembahasan UKDI CLINIC 3 Batch Mei 2016widi kusumaNessuna valutazione finora
- Antibiotic Therapy For Peritonitis: Treatment Overview, Spontaneous Bacterial Peritonitis, Secondary and Tertiary PeritonitisDocumento7 pagineAntibiotic Therapy For Peritonitis: Treatment Overview, Spontaneous Bacterial Peritonitis, Secondary and Tertiary PeritonitisTias SubagioNessuna valutazione finora
- Blunt Adominal TraumaDocumento13 pagineBlunt Adominal TraumaIlham RamadhanNessuna valutazione finora
- Cervical Spine InjuriesDocumento18 pagineCervical Spine InjuriesAnnapurna DangetiNessuna valutazione finora
- Fistel Vesicovaginalis, Ureterocutaneous, Dan UreterorectalisDocumento24 pagineFistel Vesicovaginalis, Ureterocutaneous, Dan Ureterorectalismizz_jcNessuna valutazione finora
- Referat PeritonitisDocumento19 pagineReferat PeritonitisAdrian Prasetya SudjonoNessuna valutazione finora
- GossipybomaDocumento8 pagineGossipybomaDADDYTONessuna valutazione finora
- Colonoscopy: Dr. Aries Budianto, SPB (K) BDDocumento52 pagineColonoscopy: Dr. Aries Budianto, SPB (K) BDRisal WintokoNessuna valutazione finora
- Hernia UmbilikalisDocumento16 pagineHernia UmbilikalisWibhuti EmrikoNessuna valutazione finora
- An Approach To A Child With OedemaDocumento14 pagineAn Approach To A Child With OedemaAdlina PutriantiNessuna valutazione finora
- LBM 2 Uro SGD 21Documento33 pagineLBM 2 Uro SGD 21CALISTA DEMONTINessuna valutazione finora
- Erin's Rad ReviewDocumento111 pagineErin's Rad ReviewmadamzelleyNessuna valutazione finora
- Pembahasan CBT COMBO 3Documento802 paginePembahasan CBT COMBO 3Sari Dewi WiratsihNessuna valutazione finora
- Subcutaneous: EmphysemaDocumento70 pagineSubcutaneous: EmphysemaWer TeumeNessuna valutazione finora
- I. Similar To Rounded Abdomen Only Greater. Anticipated in Pregnancy, Also Seen in Obesity, Ascites, and Other Conditions IIDocumento3 pagineI. Similar To Rounded Abdomen Only Greater. Anticipated in Pregnancy, Also Seen in Obesity, Ascites, and Other Conditions IIroxanneNessuna valutazione finora
- 17 Brain VascularizationDocumento86 pagine17 Brain VascularizationMuhammad RidwanNessuna valutazione finora
- 2 - Kidney TraumaDocumento72 pagine2 - Kidney TraumaHendra SalehNessuna valutazione finora
- (26sept) Perdarahan Saluran Cerna - Dr. SalmanDocumento52 pagine(26sept) Perdarahan Saluran Cerna - Dr. SalmanAnonymous NDAtNJyKNessuna valutazione finora
- Vaginosis BakterialisDocumento9 pagineVaginosis BakterialisIntan PermataNessuna valutazione finora
- CLARA SKIN Who PDFDocumento154 pagineCLARA SKIN Who PDFhasnul ramadhaniNessuna valutazione finora
- Slide MANTAP BEDAH 2 PDFDocumento203 pagineSlide MANTAP BEDAH 2 PDFIni DiaNessuna valutazione finora
- Striktur UrethraDocumento7 pagineStriktur UrethraEl-yes Yonirazer El-BanjaryNessuna valutazione finora
- De La Maza, Maite Sainz, MD, Phd. Scleritis. 2010. (Diakses Tanggal)Documento1 paginaDe La Maza, Maite Sainz, MD, Phd. Scleritis. 2010. (Diakses Tanggal)fa dliNessuna valutazione finora
- Tokyo Guidelines 2018 Flowchart For The Management of Acute CholecystitisDocumento43 pagineTokyo Guidelines 2018 Flowchart For The Management of Acute Cholecystitisfranciscomejia14835Nessuna valutazione finora
- Bi-Rads: (Breast Imaging-Reporting and Data System)Documento30 pagineBi-Rads: (Breast Imaging-Reporting and Data System)Siti NirwanahNessuna valutazione finora
- Colonoscopy CecilDocumento14 pagineColonoscopy Cecilyaba100% (1)
- Jurnal Striktur NcbiDocumento5 pagineJurnal Striktur NcbiYohana Elisabeth GultomNessuna valutazione finora
- Xanthogranulomatous PyelonephritisDocumento14 pagineXanthogranulomatous PyelonephritisalaaNessuna valutazione finora
- K4. Diagnosis Holistik - EngDocumento21 pagineK4. Diagnosis Holistik - EngBevila KorspoilvilNessuna valutazione finora
- EmpyemaDocumento17 pagineEmpyemaNoviaCandraDwipaNessuna valutazione finora
- Case Report Session: Apendisitis AkutDocumento32 pagineCase Report Session: Apendisitis AkutAnonymous ckZmIgoNessuna valutazione finora
- Hirschsprung DiseaseDocumento20 pagineHirschsprung DiseaseIyan AsianaNessuna valutazione finora
- Guildelines For Hiv Testing NacoDocumento165 pagineGuildelines For Hiv Testing NacoNagendra Singh BeniwalNessuna valutazione finora
- Komplikasi Stroke PDFDocumento7 pagineKomplikasi Stroke PDFJose Hady PuteraNessuna valutazione finora
- Bilas LambungDocumento12 pagineBilas LambungNthie UnguNessuna valutazione finora
- Albumin in Liver Cirrhosis, SADocumento37 pagineAlbumin in Liver Cirrhosis, SADwinita ViviantiNessuna valutazione finora
- Referat Sle Cover PageDocumento3 pagineReferat Sle Cover PageFarhana Fefe Amani FeFeNessuna valutazione finora
- OsteosarkomaDocumento2 pagineOsteosarkomaLinawati DLNessuna valutazione finora
- A Guide For People Having A ColonosDocumento16 pagineA Guide For People Having A ColonossubhankarNessuna valutazione finora
- BPHDocumento10 pagineBPHMichelle SalimNessuna valutazione finora
- Chest TubeDocumento8 pagineChest TubeTaufik Nur YahyaNessuna valutazione finora
- Ruptur UrethraDocumento26 pagineRuptur UrethraTantigunadiNessuna valutazione finora
- Ileus - Prof - Bachtiar Murtala (PP) PDFDocumento37 pagineIleus - Prof - Bachtiar Murtala (PP) PDFAchmad Rizki AlhasaniNessuna valutazione finora
- Intrapleural Ruptured Hydatid Cyst of Liver Presented As Eosinophilic Pleural Effusion: Case ReportDocumento7 pagineIntrapleural Ruptured Hydatid Cyst of Liver Presented As Eosinophilic Pleural Effusion: Case ReportIJAR JOURNALNessuna valutazione finora
- Jejunum IleumDocumento55 pagineJejunum IleumDitas ChuNessuna valutazione finora
- Emergency Management of Chemical Burns PDFDocumento3 pagineEmergency Management of Chemical Burns PDFdeasyarizaniNessuna valutazione finora
- WIFI Score For Diabetes Foot UlcerDocumento17 pagineWIFI Score For Diabetes Foot Ulcertonylee24100% (1)
- Olanzapine Vs AripiprazoleDocumento8 pagineOlanzapine Vs AripiprazoleDivaviyaNessuna valutazione finora
- DrowningDocumento10 pagineDrowningTrue Crime ReviewNessuna valutazione finora
- RP 3Documento5 pagineRP 3Mrudula TompeNessuna valutazione finora
- Causes of Laryngeal Cartilage and Hyoid Bone Fractures Found at PostmortemDocumento6 pagineCauses of Laryngeal Cartilage and Hyoid Bone Fractures Found at PostmortemMyrellaAlexandraNessuna valutazione finora
- DrowningDocumento10 pagineDrowningadesamboraNessuna valutazione finora
- Psoriasis Global AssessmentDocumento3 paginePsoriasis Global AssessmentYuliasminde SofyanaNessuna valutazione finora
- Na Rro W Vs BR Oa D-Spe CTR Um An Tim Icr Obi Al TH Era Py For CH Ildr en Ho Spi Tali Zed Wi TH PNDocumento69 pagineNa Rro W Vs BR Oa D-Spe CTR Um An Tim Icr Obi Al TH Era Py For CH Ildr en Ho Spi Tali Zed Wi TH PNYuliasminde SofyanaNessuna valutazione finora
- Fisiologi DiuresisDocumento26 pagineFisiologi DiuresisYuliasminde SofyanaNessuna valutazione finora
- Yuliasminde Sofyana 12.06.0027 Winda Adriyanti Parmana 12.06.0029 M. Najif MauludiDocumento6 pagineYuliasminde Sofyana 12.06.0027 Winda Adriyanti Parmana 12.06.0029 M. Najif MauludiYuliasminde SofyanaNessuna valutazione finora
- Dijabetička KetoacidozaDocumento19 pagineDijabetička KetoacidozaToNijeToniNessuna valutazione finora
- Endothelial Dysfunction and Vascular Disease - A 30th Anniversary UpdateDocumento75 pagineEndothelial Dysfunction and Vascular Disease - A 30th Anniversary UpdateAna Clara RodriguesNessuna valutazione finora
- Study of The Consumer Preference For Milk Brands in Colombo DistrictDocumento74 pagineStudy of The Consumer Preference For Milk Brands in Colombo DistrictJanitha DissanayakeNessuna valutazione finora
- Endocrine Glands RevisedDocumento47 pagineEndocrine Glands RevisedXyress Archer GosinganNessuna valutazione finora
- School of Out-Of-BodyDocumento224 pagineSchool of Out-Of-Bodyrpandit075698100% (2)
- Drug Study NubainDocumento2 pagineDrug Study NubainampalNessuna valutazione finora
- HSCRP Level-0,5Documento10 pagineHSCRP Level-0,5Nova SipahutarNessuna valutazione finora
- Diagnosis & Management of Anaphylactic Shock NewDocumento6 pagineDiagnosis & Management of Anaphylactic Shock Newputri auliyahNessuna valutazione finora
- Introduction To PlantsDocumento32 pagineIntroduction To Plantslanie_bluegirlNessuna valutazione finora
- Occult Meaning of Colours Purple Haze, All in My BrainDocumento54 pagineOccult Meaning of Colours Purple Haze, All in My BrainrobinhoodlumNessuna valutazione finora
- Bronchiectasis Physiotherapy Assessment Form 2Documento4 pagineBronchiectasis Physiotherapy Assessment Form 2jefferyNessuna valutazione finora
- Skin - Structure and Function Flashcards - QuizletDocumento5 pagineSkin - Structure and Function Flashcards - QuizletDani AnyikaNessuna valutazione finora
- Human Excretory SystemDocumento6 pagineHuman Excretory SystemRahul SinghNessuna valutazione finora
- Lesson 4 - Circulatory SystemDocumento21 pagineLesson 4 - Circulatory Systemapi-307592530Nessuna valutazione finora
- Electrical Burn PathophysiologyDocumento1 paginaElectrical Burn PathophysiologydanicaNessuna valutazione finora
- Golnic Lipidai Fingernails 000029915Documento9 pagineGolnic Lipidai Fingernails 000029915Vita BūdvytėNessuna valutazione finora
- Pathology of Neurodegenerative DiseasesDocumento22 paginePathology of Neurodegenerative DiseasesKarel GuevaraNessuna valutazione finora
- Endocrine Organs 2004Documento323 pagineEndocrine Organs 2004Game TesterNessuna valutazione finora
- Women's Health MagazineDocumento140 pagineWomen's Health MagazineAgiimaa0% (1)
- CarbohydratesDocumento10 pagineCarbohydratesshajmalikNessuna valutazione finora
- Conventional Blood Banking and Blood Component Storage Regulation: Opportunities For ImprovementDocumento7 pagineConventional Blood Banking and Blood Component Storage Regulation: Opportunities For ImprovementKatona imreNessuna valutazione finora
- Newport, D.J. and Nemeroff, C.B. Neurobiology of Posttraumatic Stress Disorder. Cognitive Neuroscience JAARTALDocumento8 pagineNewport, D.J. and Nemeroff, C.B. Neurobiology of Posttraumatic Stress Disorder. Cognitive Neuroscience JAARTALg10564433Nessuna valutazione finora
- Manor Supplementary Notes PCOGDocumento32 pagineManor Supplementary Notes PCOGBenjamin TNessuna valutazione finora
- Anaphy Reviewer PrefinalsDocumento12 pagineAnaphy Reviewer PrefinalsNicole Faith L. NacarioNessuna valutazione finora
- Endocrine Physiology: Dale Buchanan Hales, PHD Department of Physiology & BiophysicsDocumento74 pagineEndocrine Physiology: Dale Buchanan Hales, PHD Department of Physiology & BiophysicsOngen AchillesNessuna valutazione finora
- List of Mineral Function and DeficiencyDocumento16 pagineList of Mineral Function and Deficiencyketavmodi100% (8)
- Body Systems Portfolio - Tommy JDocumento8 pagineBody Systems Portfolio - Tommy Japi-554072790Nessuna valutazione finora
- Emma Jordan - Research Final DraftDocumento7 pagineEmma Jordan - Research Final Draftapi-436829682Nessuna valutazione finora
- Photosynthesis Lab Using Co2 SensorDocumento5 paginePhotosynthesis Lab Using Co2 Sensorapi-287606445Nessuna valutazione finora
- Neurexan Patient Flyer ANG May 2010 7311Documento2 pagineNeurexan Patient Flyer ANG May 2010 7311Waqar GhoryNessuna valutazione finora