Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Endocrine Pathophysiology Nursing Notes - Part 2
Caricato da
grad_nurse_2015Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Endocrine Pathophysiology Nursing Notes - Part 2
Caricato da
grad_nurse_2015Copyright:
Formati disponibili
Patho Wk 7: Endocrine
Part 2 - 1
ENDOCRINE PATHOPHYSIOLOGY PART 2
ENDOCRINE DISORDERS:
Primary Disorder = Defect within the gland
o Ex: Primary hypothyroidism
Secondary Disorder = Over/under stimulation
o Ex: Pituitary Secondary hyperaldosteronism or hypothyroidism
Hypersecretion = Hormone excess
ETIOLOGY:
o Over-stimulation
o Secreting tumors
o Ectopic hormone production
o Exogenous hormones (corticosteroids)
o Antibodies
o Gland destruction
TREATMENT:
o Surgery
o Chemical ablation
o Stop hormone replacement
Hyposecretion = Too little hormone
ETIOLOGY:
o Under-stimulation
o Autoimmunity
o Non-secreting tumor
o Ischemia
o Infarction
o Surgical removal (tx for hyperthyroid remove thyroid leads to hypothyroidism)
o Receptor defects
TREATMENT:
o Hormone replacement therapy
SIADH = Syndrome of Inappropriate ADH secretion
Hypersecretion of ADH causing excessive reabsorption of water by the kidney
CAUSES:
o Tumors
o Head trauma
o IV fluids
o PNA, Infxns, drugs
SIGNS/SYMPTOMS:
o Hyponatremia
o Hemodilution
o CNS changes (r/t how low Na+ level is)
TREATMENT = RAISE NA+ LEVEL
o Water restriction
o Administer sodium (hypertonic saline, 3%)
o Furosemide to block circulatory overload (pee out water)
o Chronic SIADH Give drugs to block the renal response to ADH
demeclocycline hydrochloride (tertracycline abx)
lithium
o Surgical removal of ADH-secreting tumors
Patho Wk 7: Endocrine
DIABETES INSIPIDUS
Hyposecretion of ADH or insensitivity to ADH
o Central (neurogenic) deficiency of ADH from posterior pituitary
o Nephrogenic renal insensitivity to ADH
Distal and collecting ducts of the nephrons fail to reabsorb water
o Psychogenic drinking too much water
CAUSES:
o Central brain injury, stroke, *pituitary tumors, infection
o Nephrogenic renal disease, medications (lithium, methicillin)
o Psychogenic polydipsia
SIGNS/SYMPTOMS:
o Hypernatremia
o Polyuria
o Dehydration
o Thirst
o Findings indicative of cause
TREATMENT:
o IM or intranasal administration of ADH
o Oral hypoglycemic agents (increase the response of the renal tubule to ADH)
o Thiazide diuretics (induce a state of salt depletion)
GROWTH HORMONE
1) GIGANTISM (Child) / ACROMEGALY (Adult) Hypersecretion of growth hormone
CAUSE:
o *Benign pituitary tumor
2)
SIGNS/SYMPTOMS: (pic)
o Increased ring, hat, shoe, and glove size
o Impotence in men
o Amenorrhea in women
o Deepening of the voice
o Thick, fleshy face
o Enlarged lips, nose, and ears
o Proganthism
o Enlarged internal organs
o Osteoporosis and arthritis develop
TREATMENT = SURGERY
o Transphenoidal hypophysectomy (remove pituitary)
Sequelae:
Transient devel of diabetes insipidus
Lifelong hormone replacement
o Radiation possibly considered
o Medications that block effects of growth hormone
DWARFISM Hyposecretion of growth hormone
CAUSE:
o Pituitary not producing adequate amounts
SIGNS/SYMPTOMS:
o Small stature
Part 2 - 2
Patho Wk 7: Endocrine
o
o
o
Slow growth rate
Late onset or absence of puberty
Normal intelligence!
TREATMENT:
o Daily growth hormone injections, but not very successful
CUSHINGS SYNDROME Manifestation of hypercortisolism (PICS)
CAUSE:
o Hypersecretion of ACTH excess cortisol
o Adrenal tumors
o Exogenous Chronic steroid use
SIGNS/SYMPTOMS:
o Hyperglycemia
o Hypernatremia
o Hypokalemia
o Thin skin (striae)/truncal obesity
o *Moon face/buffalo hump
o *Elevated am cortisol
TREATMENT:
o DEC or d/c steroids
o Surgery if endogenous, ectopic
o Manage electrolyte imbalance
ADDISONS DISEASE Insufficient production of adrenocortical hormones
CAUSE:
o Autoimmune
o Cancer
o Pituitary failure
SIGNS/SYMPTOMS:
o Hypoglycemia
o Hyponatremia
o Hyperkalemia
o *Low am plasma cortisol
o Skin Hyperpigmentation (PIC)
TREATMENT:
o Endocrine referral
o Glucocorticoid and mineralocorticoid replacement (life-long!)
Hydrocortisone
Florinef
May progress to ADDISONIAN CRISIS
o Usually related to infection
o Metabolic acidosis
o Hemodynamic instability
o Death
o Want to avoid stress!
Must be treated with stress-dose hydrocortisone to prevent shock rxn
Part 2 - 3
Patho Wk 7: Endocrine
Part 2 - 4
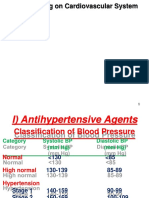
HYPERALDOSTERONISM Excessive secretion of aldosterone (in renin-angiotensin-aldo loop)
- Primary disorder = Conns Disease
- Secondary disorder
CAUSE:
o Adrenocortical neoplasm
o Sustained renin release (secondary)
SIGNS/SYMPTOMS:
o HTN difficult to control!
o Hypokalemia
Muscle weakness, weakness, paralysis, cardiac dysrhythmia
o Hypernatremia
TREATMENT:
o ACE inhibitor and/or surgery to remove gland
PHEOCHROMOCYTOMA Catecholamine-secreting tumor of the adrenal medulla resulting in excess catechols (epi/norpei)
SIGNS/SYMPTOMS:
o *Hypertension (labile)
o Tachycardia
o Palpitations, diaphoresis, and flushing
o N&V, blurred vision, and headaches
o Hyperventilation
o Hyperglycemia
o Appear nervous
TREATMENT:
o Surgery main tx
o Regitine
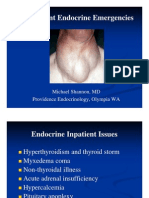
HYPOTHYROIDISM Absent or d level of circulating thyroid hormone
Cretinism (child)
Myxedema (adult)
CAUSES:
o Congenital
o Insufficient iodine in the diet
o Surgery: Partial or complete thyroidectomy
o Irradiation
o Amiodarone (Cardiac)
SIGNS/SYMPTOMS EVERYTHING SLOWS DOWN!
o No energy!
o d basal metabolic rate weight gain, fatigue
o Cold intolerance
o Edema/puffiness
o Mental retardation (child)
o Dry skin
o Myxedema coma profound hypothyroid state
LOC/confusion progressing to coma if not reversed
LABS: Elevated TSH, low-normal T4, low T3
TREATMENT:
o Thyroid hormone life-long!
HYPERTHYROIDISM : GRAVES DZ Excess production of thyroid hormone
CAUSES:
o More common in women (8:1)
Patho Wk 7: Endocrine
o
o
o
Part 2 - 5
Familial
May be autoimmune (antibodies to thyroid hormone)
Amiodarone can cause both hypo or hyper r/t mechanism
SIGNS/SYMPTOMS EVERYTHING SPEEDS UP!
o Goiter (PIC)
o d basal metabolic rate weight loss
o d heart rate (atrial fibrillation!)
o d blood pressure
o d GI motility
o Heat intolerance
o Nervousness
o *Exophthalmos (late finding) non-reversible!
LABS: Low TSH, elevated T3 and T4
TREATMENT:
o Endocrine consult
o Symptom relief beta blocker (Propanolo/Inderal)
o *Surgery or Radioactive iodine Destroys goiter
HYPERTHYROIDISM: THYROTOXICOSIS Excess production (LOTS) of thyroid hormone
Inadequate control of hyperthyroidism (worst presentation)
Deadly hyper-metabolic state
CAUSE:
o Systemic infections
o Uncontrolled diabetes
o Stress: Trauma
o Myocardial infarction
o Thyroid ablation
o Thyroid medication overdose
PATHOPHYSIOLOGY:
o d basal metabolic activity (BMR)
o Stimulates beta adrenergic receptors
o d neural excitability (seizures)
o d heat production
o d cellular O2 consumption (inc metabolic demand)
o d energy production
o O2 demand exceeds O2 supply
o Tachycardia
o *Critically high fever
o Appetite s
o Carbohydrates, fats, and proteins, are mobilized to attempt to meet metabolic demands
PATHOPHYSIOLOGY: cont
o Nitrogen and uric acid excretion increases
o Metabolic acidosis
o Intestinal peristalsis increases
o Dehydration
o Malnutrition
o Tachy-arrhythmias, CHF, and pulmonary edema
THYROTOXICOSIS Goals of treatment = must turn off the mechanism! DEC production/release of thyroid hormone
Reduce production of thyroid hormone
o propylthiouracil (PTU)
o methimazole (Tapezole)
Patho Wk 7: Endocrine
Part 2 - 6
Reduce the release of thyroid hormone
o Iodine drugs (Sodium iodide, SSKI)
o Dexamethasone (Decadron)
Reduce conversion of T4 to T3
o Use acetaminophen instead of aspirin
Suppress adrenergic and catecholamine receptors (treating the symptoms)
o Propranolol (Inderal)
Control pyrexia
o Cooling blanket
o Acetaminophen
o Dantrolene last measure
Increase O2 supply (demand exceeding supply)
o 100% oxygen
Treat dehydration
o Give large volumes of IVF with glucose
Control metabolic acidosis
o 100% O2
o NaHCO3
Treat congestive heart failure
o Digitalis (Digoxin) myocardial contractility
o Diuretics fluid removal
HYPERparaTHYROIDISM
Primary hyperparathyroidism
o Excess secretion of PTH from one or more parathyroid glands (4 glands total)
o 85% caused by parathyroid adenomas
Secondary hyperparathyroidism r/t other diseases
o Increase in PTH secondary to a chronic disease
Renal failure
Dietary deficiency of vitamin D, calcium
CLINICAL SIGNS: (urine)
o Hypercalciuria
o Alkaline urine
o Hyperphosphaturia Predisposes to the formation of calcium stones
HYPOparaTHYROIDISM
Usually caused by parathyroid damage in thyroid surgery
Abnormally low PTH levels
o d serum calcium level
o d serum phosphate level
CLINICAL SIGNS:
o Hypocalcemia
Lowering of the threshold for nerve and muscle excitation
Muscle spasms; hyperreflexia; tonic-clonic convulsions; laryngeal spasms; death from asphyxiation
o Phosphate retention
ENDOCRINE PATHOPHYSIOLOGY PART 3
DIABETES MELLITUS
Chronic disorder of metabolism characterized by a lack of insulin
o Relative lack or Absolute lack (Type I)
o Characterized by hyperglycemia
o Approximately 14 million people affected
CLASSIFICATIONS:
Patho Wk 7: Endocrine
o
o
o
o
Type 1 (absolute)
Type 2
Secondary or other
Gestational
PREDISPOSING FACTORS:
o Genetics
o Diet high in saturated fats
o Obesity
o Pregnancy
o Autoimmunity
o Lack of insulin receptors on cells
INSULIN hormone secreted from islet of langerhan cells of pancreas
o Promotes glucose transport into cells
o s glucose utilization
o s glycogenesis & glycolysis
o s blood glucose
o Promotes fatty acid transport into cells
o Promotes lipogenesis (s fat storage)
o s fat mobilization
HYPOGLYCEMIA Serum glucose < 70 mg/dl
MANIFESTATIONS:
o Hunger, Weakness, Tremor
o Diaphoresis, Cold, Clammy
o Low plasma blood sugar
HYPERGLYCEMIA Serum glucose >105 (fasting) or >140 (postprandial)
Non-diabetic!
MANIFESTATIONS:
o Polydipsia
o Polyphagia
o Polyuria
o Dehydration
o Blurred vision
o Elevated plasma blood glucose
TYPE 1 DM absolute deficiency of insulin
CHARACTERISTICS:
o Onset in childhood and adolescence
o Catabolic state (breaking down)
o First development of ketosis (ketones present in urine)
o Autoimmune destruction of beta cells absolute deficiency of insulin!
Thought to be r/t genetic/environmental interaxn
o Requires life-long insulin therapy
o Presence of human leukocyte antigens
HLA-DR3 or HLA-DR4
PATHOPHYSIOLOGY:
o NO insulin production
o Beta cells non-functional
*LAB DIAGNOSIS: (Type 1 or Type 2!)
o Fasting glucose: >/= 126 on 2 separate occasions
o Random glucose: >/= 200 with polyuria, polydipsia, and weight loss
o Glucose tolerance test: Oral glucose ingested, test at intervals. If glucose >/= 200 at 2-hr interval
o HgbA1c: Normal 5.5 7%
Part 2 - 7
Patho Wk 7: Endocrine
Part 2 - 8
NOT used for diagnosis in Type 1
TREATMENT:
o Insulin Injections!!
o Endocrine consult
o Diabetes Educator referral
SOMOGYI EFFECT = Nocturnal hypoglycemia causing surge of counter-regulatory/compensatory hormone
o d am blood sugar but d 3am blood sugar (hypoglycemic)
Cortisol is released in response to the hypoglycemia, causing high am blood sugar
o TREAT: by lowering or deleting HS (bedtime) insulin dose
DAWN PHENOMENON = Decreased sensitivity to insulin at night
o d am blood sugar and d 3am blood sugar
o TREAT: by adding or increasing HS insulin dose
TREATMENT OF DM INSULIN!
Must be given parenterally
Used for both Type 1 (always) and Type 2
EXAMPLES:
o Regular insulin (short-acting)
o NPH insulin
o Intermediate acting insulin
o Long acting sustained release
o Mixed NPH/Regular
o Insulin pumps (infuses regular insulin)
DIABETIC KETOACIDOSIS (DKA) Acute complication of DM
Intracellular dehydration secondary to elevated blood glucose
SIGNS/SYMPTOMS:
o Hyperglycemia
o Polyuria/Polydipsia
o *Ketonuria/Ketonemia
o *Metabolic acidosis
o *HyperK+
o *Fruity breath
o Kussmauls respirations
o Changed LOC
o Orthostatic hypotension and tachycardia
o Elevated BUN/Cr
TREATMENT:
o Isotonic IVF (NS): 1 liter in 1 hour, then 500cc/hr
Change to NS or D5NS depending on glucose level
o Insulin/Glucose Stabilizer Protocols
o Bicarbonate gtt for severe acidosis
o May require intubation monitor WOB and oxygenation
o Do NOT treat initial hyperK+ will correct when you tx the glucose level and DKA (follow K levels)
TYPE 2 DM insulin resistance
Most common type of diabetes
Onset usually after the age of 40 (but getting much younger!)
Patho Wk 7: Endocrine
CHARACTERISTICS:
o Resistance to insulin action
o Defective glucose-mediated insulin secretion
May or may not require insulin therapy (b/c dont have absolute insulin deficiency)
o Absence of ketones
o Associated with Metabolic Syndrome
TREATMENT control blood sugar
o Oral Hypoglycemic Drugs
Stimulate beta cells to secrete insulin in pancreas
May increase cellular receptors for insulin
o Examples
Glyburide
Glucatrol
Tolinase
Diabenese
Diabeta
Glucophage
Januvia
METABOLIC SYNDROME type 2 DM precursor; however, it is NOT actually diabetes
CHARACTERISTICS:
O Central Obesity
o Insulin Resistance
o HTN
o d lipids
o d aldosterone
o d facial hair growth
o d skin pigmentation
o **d risk for CVD
TREATMENTS:
o Weight loss
o Blood sugar control
o Lipid management
o BP control
o Aldactone (K-sparing diuretic)
HYPEROSMOLAR HYPERGLYCEMIC NONKETOSIS (HHNK) Complication of DM
More common in Type II DM
High mortality
CHARACTERISTICS:
o *Extremely high glucose levels (>600mg/dl)
o Hyperosmolarity
o Osmotic diuresis (d/t hyperglycemia)
o Dehydration
o *Absence of ketones!! [differentiates btwn DKA (+ketones) and HHNK]
PRECIPITATING FACTORS:
o Stress
o Extensive burns
o Infection
o Myocardial infarction
o TPN or enteral feedings
o Glucocorticoids
o Thiazide diuretics
MANIFESTATIONS:
o *No metabolic acidosis, no ketones
o Polyuria
o Weakness
Part 2 - 9
Patho Wk 7: Endocrine
o
o
o
o
o
o
Obtundation
Dehydration
Serum osmolality >310 mOsm/kg
Elevated hematocrit (hyperosmolar state)
*HypoK+
Hypophosphatemia
TREATMENT Rehydrate!
o Normal saline for the first hour
o 1/2 normal saline
o D5W when the blood glucose between 250 to 300 mg/dl
o Regular insulin
o Treat the underlying cause
LONG-TERM COMPLICATIONS OF DIABETES TYPE 1 AND 2
Retinopathy (leading cause of blindness = diabetes)
Nephropathy (leading cause of ESRD = diabetes, 2nd leading cause = HTN)
Neuropathy, PVD, Arterial insufficiency (leading cause of non-traumatic amputations = diabetes)
o Cant feel their extremities, nerve damage, dec blood flow
Gastropathy N/V
Myocardial infarction
CVA/stroke
d susceptibility to infection
Part 2 - 10
Potrebbero piacerti anche
- Pharmacology HESI ReviewDocumento13 paginePharmacology HESI Reviewhkw0006164% (11)
- Endocrine NursingDocumento2 pagineEndocrine NursingUnclePorkchop94% (34)
- Hematological NursingDocumento4 pagineHematological Nursingkhaeydianco100% (5)
- Nursing Pharmacology Inflammation Study GuideDocumento11 pagineNursing Pharmacology Inflammation Study GuideChelsea Smith100% (1)
- Nursing PharmacologyDocumento22 pagineNursing PharmacologyDharren Rojan Garvida Agullana100% (2)
- Nervous SystemDocumento10 pagineNervous Systemshenric16Nessuna valutazione finora
- Pharmacology Study Notes - Adrenergic DrugsDocumento2 paginePharmacology Study Notes - Adrenergic Drugsstuckaluck83% (6)
- Gastrointestinal NursingDocumento8 pagineGastrointestinal Nursingohsnapitslei90% (10)
- Pharmacology Question BankDocumento24 paginePharmacology Question BankSiri SriNessuna valutazione finora
- Endocrine Pathophysiology Nursing NotesDocumento4 pagineEndocrine Pathophysiology Nursing Notesgrad_nurse_2015100% (2)
- 21st Century Managerial and Leadership SkillsDocumento19 pagine21st Century Managerial and Leadership SkillsRichardRaqueno80% (5)
- Endocrine NursingDocumento8 pagineEndocrine NursingBunny Bonny100% (5)
- Endocrine DisordersDocumento16 pagineEndocrine DisordersEiffel AnchetaNessuna valutazione finora
- Pharmacology: A ReviewDocumento26 paginePharmacology: A Reviewjava_biscocho122988% (8)
- Top 400 Q & A Ms & FundaDocumento9 pagineTop 400 Q & A Ms & FundaericNessuna valutazione finora
- Neurologic Disorders - NCM 102 LecturesDocumento12 pagineNeurologic Disorders - NCM 102 LecturesBernard100% (4)
- Nursing Care of Client With Endocrine DisorderDocumento93 pagineNursing Care of Client With Endocrine DisorderApril_Anne_Vel_343Nessuna valutazione finora
- Med Surg NotesDocumento64 pagineMed Surg NotesRAYMUND IAN ABALOS100% (2)
- Endocrine Drug ChartDocumento1 paginaEndocrine Drug ChartJessicaNessuna valutazione finora
- Endocrine Disorders (Study Notes)Documento11 pagineEndocrine Disorders (Study Notes)Danelle Harrison, RN90% (10)
- Medical Surgical Nursing Review Notes 30pgsDocumento32 pagineMedical Surgical Nursing Review Notes 30pgsNormala Macabuntal SaripadaNessuna valutazione finora
- Neuro Study GuideDocumento11 pagineNeuro Study GuideEllen Hennings100% (1)
- Learning Packet in Level 1-NCM 106 NURSING PHARMACOLOGY: College of Nursing School Year 2020-2021Documento15 pagineLearning Packet in Level 1-NCM 106 NURSING PHARMACOLOGY: College of Nursing School Year 2020-2021Nur Sanaani100% (1)
- ENDOCRINE NURSING-FINAL HDDocumento15 pagineENDOCRINE NURSING-FINAL HDJayvee Novenario Casaljay100% (1)
- Autonomic DrugsDocumento107 pagineAutonomic DrugsMaria Mercedes LeivaNessuna valutazione finora
- Cardiovascular Med Surg Memory Notebook of NursingDocumento8 pagineCardiovascular Med Surg Memory Notebook of NursingdmsapostolNessuna valutazione finora
- Respiratory Drugs XL Chart 3Documento2 pagineRespiratory Drugs XL Chart 3cdp1587100% (1)
- MedSurg NeuroDocumento8 pagineMedSurg NeuroZachary T Hall100% (1)
- Drugs Acting On Cardiovascular SystemDocumento18 pagineDrugs Acting On Cardiovascular SystemIbrahem AlNessuna valutazione finora
- PharmacologyDocumento21 paginePharmacologyMaridel Estioco100% (3)
- Drugs WorksheetDocumento16 pagineDrugs Worksheetninja-2001Nessuna valutazione finora
- Drug Outline: Autonomic Nervous System Drug Class Drug OtherDocumento4 pagineDrug Outline: Autonomic Nervous System Drug Class Drug OtherCess Lagera YbanezNessuna valutazione finora
- Medical Surgical Nursing BulletsDocumento75 pagineMedical Surgical Nursing Bulletsmervilyn100% (3)
- Anti-Infectives and AntibioticsDocumento38 pagineAnti-Infectives and AntibioticsKarel Lu0% (1)
- Cheat Sheet - Growth and DevelopmentDocumento4 pagineCheat Sheet - Growth and Developmentdecsag06Nessuna valutazione finora
- Nursing Pharmacology Perfusion Study GuideDocumento9 pagineNursing Pharmacology Perfusion Study GuideChelsea SmithNessuna valutazione finora
- Cholinergics and Cholinergic BlockersDocumento5 pagineCholinergics and Cholinergic Blockersapi-3739910100% (3)
- Disorders of Cranial NervesDocumento3 pagineDisorders of Cranial Nervestheglobalnursing100% (2)
- Nursing Pharmacology HandoutsDocumento9 pagineNursing Pharmacology HandoutsVince LeonidaNessuna valutazione finora
- PharmacologyDocumento68 paginePharmacologyvansal liu80% (5)
- Neurologic DisordersDocumento51 pagineNeurologic DisordersYamSomandar100% (1)
- MEdical Surgical REVEWERDocumento86 pagineMEdical Surgical REVEWERennaedNessuna valutazione finora
- Endocrine SystemDocumento8 pagineEndocrine Systemtheglobalnursing80% (5)
- Communicable and Infectious Disease Nursing-NewDocumento15 pagineCommunicable and Infectious Disease Nursing-NewShandz de RosasNessuna valutazione finora
- Endocrine DisordersDocumento3 pagineEndocrine DisordersIrish OrleansNessuna valutazione finora
- 81 HematologyDocumento18 pagine81 HematologyLuis Perez100% (5)
- Nursing Lecture NeurologicalDocumento28 pagineNursing Lecture NeurologicalAedge010100% (1)
- Blue Print Final Class Med Surg IIDocumento9 pagineBlue Print Final Class Med Surg IIbaconhater100% (1)
- Medicationpart1 110202192115 Phpapp02Documento10 pagineMedicationpart1 110202192115 Phpapp02Jessamine Rochelle Reyes Esberto100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDa EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNessuna valutazione finora
- Endocrine System: Major Hormone Secreting Glands: 1. HypothalamusDocumento5 pagineEndocrine System: Major Hormone Secreting Glands: 1. HypothalamusSTEFFI GABRIELLE GOLEZNessuna valutazione finora
- Anaesthesia For Thyroid Surgery....Documento46 pagineAnaesthesia For Thyroid Surgery....Parvathy R NairNessuna valutazione finora
- Disease of Adrenal GlandDocumento47 pagineDisease of Adrenal GlandgibreilNessuna valutazione finora
- Endocrine EmergenciesDocumento33 pagineEndocrine EmergenciesbetyahNessuna valutazione finora
- NCMB 316 Cu13 ThyroidDocumento33 pagineNCMB 316 Cu13 ThyroidJanine Dela CruzNessuna valutazione finora
- Endocrine Reviews UndanaDocumento132 pagineEndocrine Reviews UndanaAndi Suchy Qumala SarieNessuna valutazione finora
- Diseases of The Endocrine SystemDocumento8 pagineDiseases of The Endocrine SystemMichelle HuangNessuna valutazione finora
- 1 - Endocrine DisordersDocumento55 pagine1 - Endocrine Disorderscephas chinkoliNessuna valutazione finora
- Rosh ReviewsDocumento19 pagineRosh ReviewsTracy NwanneNessuna valutazione finora
- Endocrine: - o in Males It Induces Sexual ArousalDocumento32 pagineEndocrine: - o in Males It Induces Sexual ArousalEmily CarlsonNessuna valutazione finora
- Thyrotoxicosis: By: DR Mukesh Kumar Samota PG (M.D. Medicine) Medical College Jhalawar (RajasthanDocumento40 pagineThyrotoxicosis: By: DR Mukesh Kumar Samota PG (M.D. Medicine) Medical College Jhalawar (RajasthanShravani ShagapuramNessuna valutazione finora
- Tyroid DiseasesDocumento40 pagineTyroid DiseasesValentina MilovaNessuna valutazione finora
- Acid Base Balance Pathophysiology NursingDocumento7 pagineAcid Base Balance Pathophysiology Nursinggrad_nurse_2015100% (2)
- Fluids and Electrolytes Pathophysiology NursingDocumento16 pagineFluids and Electrolytes Pathophysiology Nursinggrad_nurse_2015100% (3)
- Cancer Pathophysiology Nursing NotesDocumento8 pagineCancer Pathophysiology Nursing Notesgrad_nurse_2015100% (2)
- Guidelines Postpartum AssessmentDocumento2 pagineGuidelines Postpartum Assessmentgrad_nurse_2015100% (1)
- Charting GuidelinesDocumento4 pagineCharting Guidelinesgrad_nurse_2015Nessuna valutazione finora
- Pediatric Issues in MobilityDocumento5 paginePediatric Issues in Mobilitygrad_nurse_2015Nessuna valutazione finora
- Unit 1 NOTESDocumento11 pagineUnit 1 NOTESgrad_nurse_2015Nessuna valutazione finora
- CH 11Documento54 pagineCH 11Dragos PopescuNessuna valutazione finora
- Jury Assessment FormDocumento2 pagineJury Assessment FormMatias CANessuna valutazione finora
- Module2.Shs CGPDocumento54 pagineModule2.Shs CGPRommelyn Perez Pelicano75% (4)
- 3 C FamilyIImoot2015Documento3 pagine3 C FamilyIImoot2015ApoorvaChandraNessuna valutazione finora
- 4 5 and 6 - Approaches To HR MeasurementDocumento14 pagine4 5 and 6 - Approaches To HR MeasurementRahul RaoNessuna valutazione finora
- Lec 2 Ideology of PakDocumento49 pagineLec 2 Ideology of PakIshfa Umar0% (1)
- Week 1Documento3 pagineWeek 1Markdel John EspinoNessuna valutazione finora
- Junto, Brian Cesar S.Documento1 paginaJunto, Brian Cesar S.Brian Cesar JuntoNessuna valutazione finora
- Why Worldview - OutlineDocumento3 pagineWhy Worldview - OutlineDaveNessuna valutazione finora
- Jurnal Teori Pertukaran SosialDocumento11 pagineJurnal Teori Pertukaran SosialRhama PutraNessuna valutazione finora
- All IL Corporate Filings by The Save-A-Life Foundation (SALF) Including 9/17/09 Dissolution (1993-2009)Documento48 pagineAll IL Corporate Filings by The Save-A-Life Foundation (SALF) Including 9/17/09 Dissolution (1993-2009)Peter M. HeimlichNessuna valutazione finora
- Oracle Database Performance Tuning Advanced Features and Best Practices For DbasDocumento303 pagineOracle Database Performance Tuning Advanced Features and Best Practices For Dbassss pppNessuna valutazione finora
- Lecture05e Anharmonic Effects 2Documento15 pagineLecture05e Anharmonic Effects 2Saeed AzarNessuna valutazione finora
- Evaluation of UNHCR's Leadership of The Global Protection Cluster and Field Protection Clusters, 2017Documento101 pagineEvaluation of UNHCR's Leadership of The Global Protection Cluster and Field Protection Clusters, 2017andyfeatherstoneNessuna valutazione finora
- Ethical Hacking and Penetration Testing Guide - Baloch, RafayDocumento2 pagineEthical Hacking and Penetration Testing Guide - Baloch, RafayAyush PoptaniNessuna valutazione finora
- UTSDocumento2 pagineUTSJan JanNessuna valutazione finora
- G12 Folk DanceDocumento30 pagineG12 Folk DanceTremolo backNessuna valutazione finora
- Take Home Assignment 2Documento2 pagineTake Home Assignment 2Kriti DaftariNessuna valutazione finora
- Stetment 10 PDFDocumento4 pagineStetment 10 PDFvaraprasadNessuna valutazione finora
- Preliminary Basic Definitions Definition: 1 GraphDocumento27 paginePreliminary Basic Definitions Definition: 1 GraphramNessuna valutazione finora
- CrimLaw2 Reviewer (2007 BarOps) PDFDocumento158 pagineCrimLaw2 Reviewer (2007 BarOps) PDFKarla EspinosaNessuna valutazione finora
- I Wish If Only WorksheetDocumento3 pagineI Wish If Only WorksheetAMADOU SALLNessuna valutazione finora
- The Billionaire Brain WaveDocumento3 pagineThe Billionaire Brain WavelittlebirdshomeeducationNessuna valutazione finora
- Appointment Letter 17may2022Documento6 pagineAppointment Letter 17may2022Gaurav ChoudharyNessuna valutazione finora
- y D Starter PDFDocumento13 paginey D Starter PDFnazar750Nessuna valutazione finora
- Thermal Conductivity and Heat Transfer in Coal SlagDocumento17 pagineThermal Conductivity and Heat Transfer in Coal SlagBun YaminNessuna valutazione finora
- Analyses For Multi-Site Experiments Using Augmented Designs: Hij HijDocumento2 pagineAnalyses For Multi-Site Experiments Using Augmented Designs: Hij HijMustakiMipa RegresiNessuna valutazione finora
- In Defense of Imam BarbahariDocumento12 pagineIn Defense of Imam Barbahariiliaswa33Nessuna valutazione finora