Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Auditory Verbal Hallucinations in Patients With Borderline Personality Disorder Are Similar To Those in Schizophrenia
Caricato da
lizardocdDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Auditory Verbal Hallucinations in Patients With Borderline Personality Disorder Are Similar To Those in Schizophrenia
Caricato da
lizardocdCopyright:
Formati disponibili
Psychological Medicine (2012), 42, 18731878. f Cambridge University Press 2012 doi:10.
1017/S0033291712000165
O R I G I N A L AR T I C LE
Auditory verbal hallucinations in patients with borderline personality disorder are similar to those in schizophrenia
C. W. Slotema1*, K. Daalman2, J. D. Blom1, K. M. Diederen2, H. W. Hoek1,3,4, and I. E. C. Sommer2
1 2
Parnassia Bavo Psychiatric Institute, The Hague, The Netherlands Department of Psychiatry & Rudolf Magnus Institute for Neuroscience, University Medical Centre Utrecht, The Netherlands 3 Department of Psychiatry, University Medical Centre Groningen, University of Groningen, The Netherlands 4 Department of Epidemiology, Columbia University, New York, NY, USA
Background. Auditory verbal hallucinations (AVH) in patients with borderline personality disorder (BPD) are frequently claimed to be brief, less severe and qualitatively dierent from those in schizophrenia, hence the term pseudohallucinations . AVH in BPD may be more similar to those experienced by healthy individuals, who experience AVH in a lower frequency and with a more positive content than AVH in schizophrenia. In this study the phenomenology of AVH in BPD patients was compared to that in schizophrenia and to AVH experienced by non-patients. Method. In a cross-sectional setting, the phenomenological characteristics of AVH in 38 BPD patients were compared to those in 51 patients with schizophrenia/schizoaective disorder and to AVH of 66 non-patients, using the Psychotic Symptom Rating Scales (PSYRATS). Results. BPD patients experienced AVH for a mean duration of 18 years, with a mean frequency of at least daily lasting several minutes or more. The ensuing distress was high. No dierences in the phenomenological characteristics of AVH were revealed among patients diagnosed with BPD and those with schizophrenia/ schizoaective disorder, except for disruption of life , which was higher in the latter group. Compared to nonpatients experiencing AVH, BPD patients had higher scores on almost all items. Conclusions. AVH in BPD patients are phenomenologically similar to those in schizophrenia, and dierent from those in healthy individuals. As AVH in patients with BPD full the criteria of hallucinations proper, we prefer the term AVH over pseudohallucinations , so as to prevent trivialization and to promote adequate diagnosis and treatment. Received 25 October 2011 ; Revised 23 January 2012 ; Accepted 23 January 2012 ; First published online 16 February 2012 Key words : Auditory verbal hallucinations, borderline personality disorder, schizophrenia.
Introduction Since the 1940s transient psychotic episodes have been recognized as possible symptoms of borderline personality disorder (BPD ; Hoch & Polatin, 1949), but it took until 1987 before they were included in DSM-IIIR which stated that during extreme stress, transient psychotic symptoms may occur (APA, 1987). With the introduction of DSM-IV in 1994, all that remained of this criterion was transient, stress-related paranoid ideation (APA, 1994). As BPD is conceptualized as a combination of aective dysregulation, impulsivebehavioural dyscontrol, cognitive-perceptual symp-
* Address for correspondence : Dr C. W. Slotema, Parnassia Bavo Psychiatric Institute, Lijnbaan 4, 2512 VA, The Hague, The Netherlands. (Email : c.slotema@psyq.nl)
toms (such as suspiciousness, ideas of reference, paranoid ideation, illusions, derealization, depersonalization, and hallucination-like symptoms), and disturbed interpersonal relatedness (APA, 2000 ; Skodol et al. 2002), psychotic symptoms occurring in the context of BPD are by denition considered to be transient, and misperceptions to be at best hallucination-like in nature. And yet there is currently no consensus on the phenomenology and severity of hallucinations and other psychotic phenomena associated with BPD. As the diagnostic criteria of BPD fail to account for the occurrence of longer-lasting hallucinations, clinicians and researchers often nd themselves struggling for words when confronted with AVH experienced by patients thus diagnosed. This is reected in the BPD-related nomenclature, which features such varying terms as micropsychotic episodes (Solo, 1979),
1874
C. W. Slotema et al. services from the Parnassia Bavo Group and the University Medical Centre Utrecht (UMCU) and diagnosed with either BPD or schizophrenia/ schizoaective disorder were recruited from May 2007 until April 2011. Inclusion criteria for the patients diagnosed with BPD were : (1) aged o18 years, (2) AVH more than once per month, and for a duration of over 1 year, (3) the diagnosis BPD was conrmed with the aid of the Structured Clinical Interview for DSM-IV, Axis II personality disorders (SCID-II ; Maei et al. 1997), and (4) the patient did not meet the criteria for schizophrenia, schizoaective disorder, bipolar disorder, major depression with psychotic symptoms or schizotypal personality disorder according to the Comprehensive Assessment of Symptoms and History (CASH ; Andreasen et al. 1992) and the SCID-II. As a consequence, all BPD patients presenting with delusions were excluded. Patients diagnosed with schizophrenia/schizoaective disorder were allowed to participate if the following criteria were met : (1) aged o18 years, (2) AVH for at least once a month, and for a duration of over 1 year, and (3) a diagnosis of schizophrenia/ schizoaective disorder was established with the aid of CASH by a psychiatrist experienced in the eld of psychotic disorders. Reasons for exclusion in both groups were alcohol abuse of three or more units per day, the use of hard drugs during the month prior to inclusion, and the daily use of cannabis. Healthy females experiencing AVH were recruited with the help of a Dutch website called Explore Your Mind (www.verkenuwgeest.nl). They were selected if they had a high score on items 8 and 12 ( In the past, I have had the experience of hearing a persons voice and then found that no-one was there and I have been troubled by voices in my head , respectively) of the LaunaySlade Hallucination Scale (LSHS ; Laroi et al. 2004). In addition, the following inclusion criteria were used : (1) aged o18 years, (2) AVH at least once a month, and for a duration of over 1 year, (3) no diagnosed psychiatric disorder, other than depressive or anxiety disorder in complete remission, and (4) no alcohol or drug abuse for at least 3 months. The CASH and SCID-II were used to exclude a psychiatric diagnosis. The non-patients and some of the patients with schizophrenia/schizoaective disorder in this study show some overlap with the study of Daalman and colleagues (2011). The study was approved by the Institutional Review Board of the UMCU and the Parnassia Bavo Psychiatric Institute, The Netherlands. Prior to the onset of the study, the participants received oral and written information regarding the content and goals of
hysterical psychosis (Lotterman, 1985), factitious psychosis (Pope et al. 1985), quasi-psychotic thought (Zanarini et al. 1990), traumatic-intrusive hallucinosis (Yee et al. 2005), stress-related psychosis (Glaser et al. 2010), pseudohallucinations (Heins et al. 1990), and hallucination-like symptoms (Skodol et al. 2002). Like the DSM criteria, these terms would seem to suggest that psychotic symptoms in BPD are short-lasting, less severe, and qualitatively dierent from those in psychotic disorders such as schizophrenia. Then, AVH in BPD would be more similar to those perceived by non-patients, who experienced voices less frequently and with a shorter duration than patients with a psychotic disorder, and experienced lower levels of ensuing distress (Daalman et al. 2011). However, empirical evidence for this suggestion is virtually lacking. In fact, the few studies that explored BPD-related psychotic symptoms in a structural manner focused on the presence of auditory hallucinations which occurred in 21 % and 54 %, respectively (Chopra & Beatson, 1986 ; George & Solo, 1986). The prevalence of auditory verbal hallucinations (AVH) was 50 %, but this was explored in only one small study (Kingdon et al. 2010). In that study the phenomenology of AVH in 15 patients with BPD was compared to AVH in 35 patients with schizophrenia and 17 patients with both schizophrenia and BPD using the Psychotic Symptom Rating Scales (PSYRATS ; Haddock et al. 1999). The groups were similar in their experiences of voices, except for distress and negative content of voices (BPD alone greater than the other groups). What those studies indicate is that the occurrence and severity of AVH in BPD are underexposed and in need of further study. More specically, it would seem necessary to assess the phenomenological characteristics of AVH in BPD patients, and to determine whether they are perhaps more similar to the non-pathological types often encountered in the healthy population (Sommer et al. 2010 ; Daalman et al. 2011). We therefore performed a prospective, cross-sectional study to answer the following questions : (1) What are the phenomenological characteristics and the ensuing distress of AVH in BPD ? (2) What are the dierences and similarities between AVH in BPD, schizophrenia/schizoaective disorder, and healthy voice hearers ? Methods Participants In the present study we included only women, as the majority of the patients treated for BPD are female (Korzekwa et al. 2008). Patients receiving psychiatric
Similarity of AVH in BPD and schizophrenia
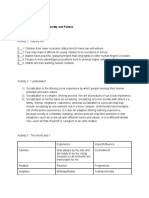
Table 1. Demographic data Schizophrenia/ schizoaective disorder (n=51) 37 (9.8) 49 (96) 8 (16) 35 (70) 15 (30) 6 (12) 29 (59) 12 (4.1)
1875
Controls with AVH (n=66) Age, mean (S.D.) Outpatient, n ( %) Medication, n ( %) Classic antipsychotics Atypical antipsychotics Antidepressive agents Mood stabilizers Benzodiazepines Years of education, mean (S.D.) 37 (11.4) 66 (100) 0 0 0 0 4 (6) 13 (2.2)
BPD (n=38) 34 (10.5) 38 (100) 7 (19) 13 (36) 21 (58) 3 (8) 14 (38) 10 (2.8)
p 0.28 0.13 <0.001 <0.001 0.02 <0.001 <0.001
AVH, Auditory verbal hallucinations ; BPD, borderline personality disorder ; S.D., standard deviation.
the study. Written informed consent was obtained from all the participants.
no diagnosis . The BenjaminiHochberg correction was used for multiple comparisons. Results Thirty-eight patients diagnosed with BPD, 51 patients with schizophrenia/schizoaective disorder (schizophrenia n=36, schizoaective disorder n=15), and 66 non-patients were included. The demographic data are presented in Table 1. All the participants were females. The mean ages of the three groups did not dier signicantly. Except for two patients in the schizophrenia/schizoaective disorder group, all of the patients were treated in an outpatient setting. Use of medication was higher in the patients with schizophrenia/schizoaective disorder. Patients with schizophrenia/schizoaective disorder and nonpatients had more years of education than patients with BPD. Three patients were excluded from the study as they had not experienced AVH in the recent months prior to inclusion. The results mentioned in the text below correspond to the mean score of the AVH-related items of the PSYRATS. Phenomenology of AVH and ensuing distress in BPD patients The mean scores of the AVH-related items of the PSYRATS are presented in Table 2 and Fig. 1. Patients diagnosed with BPD had experienced AVH for a long duration (mean 18 years). The majority of them experienced AVH more than once per day, with a duration of at least several minutes. The hallucinations were mostly experienced inside the head, and attributed to intracorporeal causes. Scores on the items negative content , distress , disruption of life , and controllability were high among this group. In 8 % of
Interviews and questionnaires The SCID-II was used to conrm the diagnosis of BPD and to exclude a schizotypal personality disorder. With the aid of the CASH, the diagnoses schizophrenia, schizoaective disorder, bipolar disorder, and major depression with psychotic symptoms were either conrmed or ruled out. The PSYRATS AVH-related items were used to describe the phenomenological characteristics and ensuing distress of AVH. The following dimensions of AVH were explored on a ve-point scale (04) : frequency, duration, perceived location, loudness, beliefs about origin, amount of negative content, degree of negative content, degree of distress, intensity of distress, disruption of life, and controllability. Furthermore, this questionnaire assessed the length of time experiencing hearing voices. Finally, a family history of schizophrenia was assessed in the patients with BPD.
Statistics A one-way analysis of variance (ANOVA) was performed to compare continuous demographic data among the three groups. In case of signicant dierences among the three groups, this variable was used as a covariate in the analysis of the AVH-related items of the PSYRATS. The dierences and similarities between AVH experienced by the members of the three groups were analysed by means of a Multivariate General Linear Model analysis with grouping variables BPD , schizophrenia/schizoaective disorder , and
1876
C. W. Slotema et al.
Table 2. Results of the Psychotic Symptom Rating Scales auditory verbal hallucination-related items Schizophrenia/ schizoaective disorder (n=66) 3.1 (0.9) 2.8 (1.1) 2.2 (1.2) 1.9 (0.9) 2.4 (1.3) 2.8 (1.2) 3.0 (1.1) 3.1 (1.1) 2.6 (0.8) 2.4 (0.8) 3.0 (1.1) 17 (11.7)
Controls with AVH (n=66) Frequency Duration Perceived location Loudness Beliefs about origin Amount of negative content Degree of negative content Amount of distress Intensity of distress Disruption of life Controllability Length of time AVH (years) 1.5 (1.2) 1.6 (0.8) 2.1 (1.2) 1.9 (0.6) 3.3 (1.1) 0.4 (1.0) 0.5 (1.1) 0.6 (1.2) 0.4 (0.9) 0.2 (0.6) 1.7 (1.4) 24 (15.7)
BPD (n=33) 2.8 (1.1) 2.7 (1.2) 1.7 (1.0) 2.1 (1.0) 2.1 (1.3) 2.8 (1.5) 2.7 (1.3) 3.0 (1.4) 2.7 (1.2) 1.8 (0.9) 2.9 (1.3) 18 (11.1)
F 37.055 27.097 1.817 0.037 12.726 66.934 76.033 75.542 106.988 126.550 20.654 4.161
p <0.001* <0.001* 0.17 1.0 <0.001* <0.001* <0.001* <0.001* <0.001* <0.001* <0.001* 0.018*
AVH, Auditory verbal hallucinations ; BPD, borderline personality disorder ; S.D. standard deviation ; F, F test, degrees of freedom 2. Values given are mean (S.D.) * Signicant after BenjaminiHochberg correction.
the patients with BPD only one family member was diagnosed with schizophrenia. Dierences and similarities between AVH and other hallucinations in BPD, schizophrenia/schizoaective disorder, and healthy subjects The results of the analyses are presented in Table 2 and Fig. 1. Signicant dierences were found for all AVH-related items between healthy individuals with AVH on the one hand, and the two other groups on the other, except for perceived location , and loudness . Post-hoc analyses revealed signicant dierences between the group without a diagnosis and the BPD group for all other items ( length of time experiencing AVH , F=4.967, df=1, p=0.028 ; other items Fo19.311, df=1, pf0.001). No signicant dierences were found between patients with BPD and those with schizophrenia/schizoaective disorder, except for disruption of life (F=11.236, df=1, p=0.001) which was higher in patients with schizophrenia/ schizoaective disorder. Furthermore, the mean age of onset of AVH was 13, 16, and 20 years for healthy subjects, BPD, and schizophrenia/schizoaective disorder, respectively. In 8 % of the patients with BPD one family member was diagnosed with schizophrenia.
4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0
No diagnosis BPD Schizophrenia/schizoaffective disorder
*
Disruption of life
Frequency
Duration
Degree of negative content
Fig. 1. Mean score on Auditory Verbal Hallucinations-related items of the Psychotic Symptom Rating Scales. BPD, Borderline personality disorder. * Signicantly dierent from the other two groups.
Discussion AVH in patients diagnosed with BPD are frequently claimed to be less severe and qualitatively dierent
from those in psychotic disorders, hence the somewhat trivializing terms pseudohallucination and transient psychotic symptom . In that case AVH among patients with BPD would be equal to those in a non-patient sample. The usage of those terms was not justied by our data. In contrast, we found that AVH
Similarity of AVH in BPD and schizophrenia experienced by BPD patients were severe, and that they lasted for lengthy periods of time, i.e. for a mean duration of 18 years. In the majority of these patients, the AVH were experienced at least daily, for at least several minutes. Moreover, 61 % of the BPD patients experienced those AVH only inside the head, and the majority had the conviction that their voices were internally generated. The scores on the items negative content , distress , and disruption of life were high among this group. For most of the time, the subjects experienced no control over their voices. When we compared the AVH experienced by the BPD group with the schizophrenia/schizoaective disorder group, no signicant dierences were revealed as regards their phenomenological characteristics. Neither did we nd any dierences on the items relating to their ensuing distress, except for disruption of life , which was scored higher by the latter group. These results conrm and extend the study by Kingdon and colleagues who also identied many similarities between AVH in BPD and in schizophrenia (Kingdon et al. 2010). However, in contrast to our results, the BPD patients in Kingdon et al.s sample presented with higher scores on the items distress and negative content of voices . These higher scores for BPD patients found in Kingdon et al. (2010), might occur by chance as the sample of BPD patients was small. In contrast, many signicant dierences were found between patients with BPD and the group of nonpatients experiencing AVH. In BPD, AVH occurred more frequently and for a longer duration. BPD patients presented with higher scores on ensuing distress (i.e. the items negative content , distress , and disruption to life ). Furthermore, the controllability of the voices was lower in BPD patients. Therefore, AVH in BPD patients are dierent from those in non-patients. This can be due to a dierence in severity or phenomenology of AVH. The higher scores for frequency, duration and distress of AVH among the BPD population t into the rst possibility ; the strong discrepancy in the content of the voices (i.e. a positive content in the majority of non-patients and a negative content in BPD patients) suggests a dierence in the phenomenology of AVH. The ndings of Sommer and colleagues (2010) indicate that the global level of functioning was lower and there was a general increased schizotypal and delusional tendency in a non-patient sample with AVH compared to individuals without AVH. Combining these results, we suggest a continuum in severity of AVH with non-patients and patients with schizophrenia on the borders. Our results imply that AVH in BPD patients are very similar to AVH in patients diagnosed with
1877
schizophrenia or schizoaective disorder. Combined with the high prevalence of AVH in BPD patients reported in the literature (Kingdon et al. 2010), more attention should be paid to the occurrence, concomitant distress, and treatment of AVH in BPD. Therefore, more research is needed, especially to nd a treatment method for this distressing symptom among this specic population. Limitations Although this is the largest study to date assessing the phenomenological characteristics of AVH in the context of BPD, the population sample of patients diagnosed with BPD can still be considered modest. And yet the majority of the dierences between AVH in BPD and in non-patients were highly signicant, with p values <0.001, while the similarities between AVH in BPD and in schizophrenia were striking. A sampling bias may have occurred due to the fact that only BPD patients reporting AVH for at least once per month were included. As only three patients were excluded for this reason, we do not think that the frequency criterion has resulted in a sampling bias. Another matter of concern is the possibility that the BPD patients might go on to develop a psychotic disorder such as schizophrenia in the future. However, we do not expect the patients in our sample to do so, given their relatively old age, and the fact that they have been experiencing AVH for a mean duration of 18 years already. A third limitation is that only females were included in this study. This yielded optimal uniformity among the groups, but reduced the possibility of extrapolating our ndings to male patients. However, the current results apply to 75 % of the BPD population, as BPD is diagnosed most frequently in women (Korzekwa et al. 2008). In sum, the patients diagnosed with BPD experienced AVH for long periods of time, with a high frequency, and high levels of ensuing distress. No dierences were found in the phenomenological characteristics of AVH, and in six out of seven of the PSYRATS items pertaining to the associated distress between patients diagnosed with BPD and those diagnosed with schizophrenia/schizoaective disorder. In comparison with healthy subjects experiencing AVH, the BPD patients scored much higher on almost all of those items. These results imply that AVH experienced by patients with BPD are hardly dierent from those experienced by patients diagnosed with schizophrenia/ schizoaective disorder. Therefore, it is neither justiable nor helpful to designate those AVH as hallucination-like symptoms , pseudohallucinations or
1878
C. W. Slotema et al.
abuse. Australian and New Zealand Journal of Psychiatry 24, 561565. Hoch P, Polatin P (1949). Pseudoneurotic forms of schizophrenia. Psychiatric Quarterly 23, 24876. Kingdon DG, Ashcroft K, Bhandari B, Gleeson S, Warikoo N, Symons M, Taylor L, Lucas E, Mahendra R, Ghosh S, Mason A, Badrakalimuthu R, Hepworth C, Read J, Mehta R (2010). Schizophrenia and borderline personality disorder : similarities and dierences in the experience of auditory hallucinations, paranoia, and childhood trauma. Journal of Nervous and Mental Disease 198, 399403. Korzekwa MI, Dell PF, Links PS, Thabane L, Webb SP (2008). Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Comprehensive Psychiatry 49, 380386. Laroi F, Marczewski P, Van der Linden M (2004). Further evidence of the multi-dimensionality of hallucinatory predisposition : factor structure of a modied version of the Launay-Slade Hallucinations Scale in a normal sample. European Psychiatry 19, 1520. Lotterman AC (1985). Prolonged psychotic states in borderline personality disorder. Psychiatric Quarterly 57, 3346. Maei C, Fossati A, Agostoni I, Barraco A, Bagnato M, Deborah D, Namia C, Novella L, Petrachi M (1997). Interrater reliability and internal consistency of the structured clinical interview for DSM-IV axis II personality disorders (SCID-II), version 2.0. Journal of Personality Disorders 11, 279284. Pope Jr. HG, Jonas JM, Hudson JI, Cohen BM, Tohen M (1985). An empirical study of psychosis in borderline personality disorder. American Journal of Psychiatry 142, 12851290. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ (2002). The borderline diagnosis I : psychopathology, comorbidity, and personality structure. Biological Psychiatry 51, 936950. Solo PH (1979). Physical restraint and the nonpsychotic patient : clinical and legal perspectives. Journal of Clinical Psychiatry 40, 302305. Sommer IE, Daalman K, Rietkerk T, Diederen KM, Bakker S, Wijkstra J, Boks MP (2010). Healthy individuals with auditory verbal hallucinations ; who are they ? Psychiatric assessments of a selected sample of 103 subjects. Schizophrenia Bulletin 36, 633641. Yee L, Korner AJ, McSwiggan S, Meares RA, Stevenson J (2005). Persistent hallucinosis in borderline personality disorder. Comprehensive Psychiatry 46, 147154. Zanarini MC, Gunderson JG, Frankenburg FR (1990). Cognitive features of borderline personality disorder. American Journal of Psychiatry 147, 5763.
micropsychotic episodes . As a corollary, we argue that more attention should be paid to the occurrence, the associated distress, and the need for treatment of the AVH experienced by BPD patients. Acknowledgements The study was supported by grants from NWO ZonMW (Dutch Scientic Research FoundationDutch National Institute of Health Research) and Stichting tot Steun (Dutch Support Foundation). Declaration of Interest None. References
Andreasen NC, Flaum M, Arndt S (1992). The Comprehensive Assessment of Symptoms and History (CASH). An instrument for assessing diagnosis and psychopathology. Archives of General Psychiatry 49, 615623. APA (1987). Diagnostic and Statistical Manual of Mental Disorders : DSM-III-R (3rd edn revised). American Psychiatric Association : Washington, D.C. APA (1994). Diagnostic and Statistical Manual of Mental Disorders (4th edition). American Psychiatric Association : Washington, D.C. APA (2000). Diagnostic and Statistical Manual of Mental Disorders (4th edn, text revision). DSM-IV-TR. American Psychiatric Association : Washington, D.C. Chopra HD, Beatson JA (1986). Psychotic symptoms in borderline personality disorder. American Journal of Psychiatry 143, 16051607. Daalman K, Boks MP, Diederen KM, de Weijer AD, Blom JD, Kahn RS, Sommer IE (2011). The same or dierent ? a phenomenological comparison of auditory verbal hallucinations in healthy and psychotic individuals. Journal of Clinical Psychiatry 72, 320325. George A, Solo PH (1986). Schizotypal symptoms in patients with borderline personality disorders. American Journal of Psychiatry 143, 212215. Glaser JP, Van Os J, Thewissen V, Myin-Germeys I (2010). Psychotic reactivity in borderline personality disorder. Acta Psychiatrica Scandinavica 121, 125134. Haddock G, McCarron J, Tarrier N, Faragher EB (1999). Scales to measure dimensions of hallucinations and delusions : the psychotic symptom rating scales (PSYRATS). Psychological Medicine 29, 879889. Heins T, Gray A, Tennant M (1990). Persisting hallucinations following childhood sexual
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Potrebbero piacerti anche
- Schreber, Daniel Paul - Memoirs of My Nervous Illness (OCR)Documento242 pagineSchreber, Daniel Paul - Memoirs of My Nervous Illness (OCR)johnsmithxx92% (12)
- Mood Disorder Management ChartDocumento1 paginaMood Disorder Management ChartechopennerNessuna valutazione finora
- Worksheets From The BFRB Recovery WorkbookDocumento64 pagineWorksheets From The BFRB Recovery WorkbookMarla DeiblerNessuna valutazione finora
- The Self in PsychotherapyDocumento26 pagineThe Self in PsychotherapyccvmdNessuna valutazione finora
- APA DSM 5 Paraphilic DisordersDocumento2 pagineAPA DSM 5 Paraphilic DisordersAli FenNessuna valutazione finora
- Altman Self Rating ScaleDocumento2 pagineAltman Self Rating ScaleRifkiNessuna valutazione finora
- Jack The Ripper An Encyclopedia (2001)Documento320 pagineJack The Ripper An Encyclopedia (2001)John Cluley100% (2)
- Bessel+Van+Der+Kolk Effective TreatmentDocumento4 pagineBessel+Van+Der+Kolk Effective TreatmentAndrei95% (21)
- 1.3.+delusions+ +hallucinations-1Documento24 pagine1.3.+delusions+ +hallucinations-1Anonymous sSR6x6VC8aNessuna valutazione finora
- Schizophrenia Spectrum and Other Psychotic DisordersDocumento49 pagineSchizophrenia Spectrum and Other Psychotic DisordersNoelle Grace Ulep BaromanNessuna valutazione finora
- DID AssessmentDocumento2 pagineDID AssessmentGrace Yeseul SongNessuna valutazione finora
- Living With Serious Mental Illness.. The Role of Personal Loss in Recovery and Quality of LifeDocumento209 pagineLiving With Serious Mental Illness.. The Role of Personal Loss in Recovery and Quality of Lifeiain-suNessuna valutazione finora
- Assessing Emotional DamagesDocumento9 pagineAssessing Emotional DamagesMark LevyNessuna valutazione finora
- Assessment ToolsDocumento74 pagineAssessment ToolsSharvari ShahNessuna valutazione finora
- Adhd - Asrs .ScreenDocumento4 pagineAdhd - Asrs .ScreenKenth GenobisNessuna valutazione finora
- (Art) (Smalley, 2009) Mindfulness and ADHDDocumento12 pagine(Art) (Smalley, 2009) Mindfulness and ADHDvickyreyeslucanoNessuna valutazione finora
- Personality Disorders in AsiansDocumento3 paginePersonality Disorders in AsiansIvee van GoghsiaNessuna valutazione finora
- Atypical PsychosisDocumento10 pagineAtypical Psychosistsurmeli100% (1)
- Voices and Pseudo-Voices in Psychosis and OCD Differential DiagnosisDocumento5 pagineVoices and Pseudo-Voices in Psychosis and OCD Differential DiagnosisRobert A. LindsayNessuna valutazione finora
- Cognitive Behavioural Therapy (CBT)Documento9 pagineCognitive Behavioural Therapy (CBT)NiloofarNessuna valutazione finora
- Intake Assessment FormDocumento3 pagineIntake Assessment Formapi-608114435Nessuna valutazione finora
- Interview-Based Ratings of DSM-IV Axis IIDSM-5 Section II Personality Disorder Symptoms in Consecutively Admitted Insomnia PatientsDocumento25 pagineInterview-Based Ratings of DSM-IV Axis IIDSM-5 Section II Personality Disorder Symptoms in Consecutively Admitted Insomnia PatientsSiti Awalia RamadhaniNessuna valutazione finora
- Schizophrenia Spectrum and Other Psychotic DisordersDocumento41 pagineSchizophrenia Spectrum and Other Psychotic DisordersNoelle Grace Ulep BaromanNessuna valutazione finora
- Deficits of Cognitive Restructuring in Major Depressive DisorderDocumento6 pagineDeficits of Cognitive Restructuring in Major Depressive DisorderIntan YuliNessuna valutazione finora
- CDI Patient VersionDocumento9 pagineCDI Patient VersionalotfyaNessuna valutazione finora
- SchizophreniaDocumento2 pagineSchizophreniaIT’S ME HAYLA100% (1)
- The Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-AnalysisDocumento52 pagineThe Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-Analysiseduardobar2000100% (1)
- The Effects of Auditory Hallucination Symptom ManagementDocumento12 pagineThe Effects of Auditory Hallucination Symptom ManagementAndika FahruroziNessuna valutazione finora
- Cognitive DissonanceDocumento15 pagineCognitive DissonancecatalinbryllaNessuna valutazione finora
- Tools For The Detection of Lying and MalingeringDocumento11 pagineTools For The Detection of Lying and MalingeringFiraFurqaniNessuna valutazione finora
- Psychosis Neurosis and Othe Mental DisorderDocumento15 paginePsychosis Neurosis and Othe Mental DisorderEr Ankita ChaudharyNessuna valutazione finora
- APA DSM 5 ContentsDocumento9 pagineAPA DSM 5 ContentsRahmi Annisa MaharaniNessuna valutazione finora
- Violence Risk Assessment NotesDocumento7 pagineViolence Risk Assessment NotesTalib9876Nessuna valutazione finora
- Physical and Mental Disability TestDocumento9 paginePhysical and Mental Disability TestANITTA SNessuna valutazione finora
- Misophonia Assessment Questionnaire (Maq) : Name: - DateDocumento12 pagineMisophonia Assessment Questionnaire (Maq) : Name: - DateSoraia RomanelliNessuna valutazione finora
- BprsDocumento7 pagineBprsamyljf100% (1)
- CatDocumento12 pagineCatnini345Nessuna valutazione finora
- DSM 5 Intellectual Disability Fact SheetDocumento2 pagineDSM 5 Intellectual Disability Fact SheetMelissa Ortega MaguiñaNessuna valutazione finora
- ACT With DepressionDocumento9 pagineACT With DepressionRan Almog100% (1)
- Educating Students About Drug Use and Mental HealthDocumento16 pagineEducating Students About Drug Use and Mental Healthtoshir01Nessuna valutazione finora
- Relationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of PsychosisDocumento6 pagineRelationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of Psychosisaldrin19Nessuna valutazione finora
- TCPR Jan 07 AntidepDocumento8 pagineTCPR Jan 07 AntidepdcarlatNessuna valutazione finora
- Abnormal Psychology DisordersDocumento34 pagineAbnormal Psychology DisordersannaNessuna valutazione finora
- Jessica Nelson, M.D. Assistant Professor of Psychiatry: Psychotic DisordersDocumento107 pagineJessica Nelson, M.D. Assistant Professor of Psychiatry: Psychotic DisordersAhmad ibrahimNessuna valutazione finora
- Mental Status ExamDocumento7 pagineMental Status ExamDanielle BanNessuna valutazione finora
- Co-Occurring Disorders: Substance Use and Mental HealthDocumento52 pagineCo-Occurring Disorders: Substance Use and Mental HealthElisyah MarsiahNessuna valutazione finora
- Aspergers Syndrome Diagnosis and TreatmentDocumento7 pagineAspergers Syndrome Diagnosis and TreatmentTilahun MogesNessuna valutazione finora
- MH Assessment TemplateDocumento2 pagineMH Assessment TemplatetakemebrickNessuna valutazione finora
- Explore - Neural and Cognitive Basis of Spiritual ExperienceDocumento10 pagineExplore - Neural and Cognitive Basis of Spiritual ExperienceVanessa Leal100% (1)
- Gestalt TherapyDocumento3 pagineGestalt TherapyOscar Villados Jr.Nessuna valutazione finora
- ASRS-ADHD-self-report-scale-2 2Documento2 pagineASRS-ADHD-self-report-scale-2 2Alexys ArchieNessuna valutazione finora
- Psychotherapy For Specific Phobia in Adults PDFDocumento6 paginePsychotherapy For Specific Phobia in Adults PDFdreamingNessuna valutazione finora
- Full Psychiatric AssessmentDocumento10 pagineFull Psychiatric AssessmentAdam GNessuna valutazione finora
- Effective Treatments For Juvenile OffendersDocumento8 pagineEffective Treatments For Juvenile OffendersAlguémNessuna valutazione finora
- Garb2005clinical Judgment and Decision MakingDocumento25 pagineGarb2005clinical Judgment and Decision MakingNicolas Di Persia100% (1)
- Where Is The Evidence For Evidence BasedDocumento11 pagineWhere Is The Evidence For Evidence BasedGabriela Ruggiero NorNessuna valutazione finora
- Introduction To Psychiatric Nursing: Mercedes A Perez-Millan MSN, ARNPDocumento33 pagineIntroduction To Psychiatric Nursing: Mercedes A Perez-Millan MSN, ARNPSachiko Yosores100% (1)
- Alcohol Misuse: Screening and Behavioral Counseling Interventions in Primary Care GuidelinesDocumento11 pagineAlcohol Misuse: Screening and Behavioral Counseling Interventions in Primary Care GuidelinesRosnerNessuna valutazione finora
- Group Therapy PDFDocumento2 pagineGroup Therapy PDFma maNessuna valutazione finora
- OCDDocumento96 pagineOCDarunvangili100% (1)
- Characteristics of Clinical PsychologistDocumento6 pagineCharacteristics of Clinical PsychologistMahnoor MalikNessuna valutazione finora
- Promoting Recovery in Early Psychosis: A Practice ManualDa EverandPromoting Recovery in Early Psychosis: A Practice ManualNessuna valutazione finora
- Capitulo BFRBDocumento9 pagineCapitulo BFRBlizardocdNessuna valutazione finora
- Pone 0261785Documento15 paginePone 0261785lizardocdNessuna valutazione finora
- The Person Behind The SyndromeDocumento241 pagineThe Person Behind The SyndromelizardocdNessuna valutazione finora
- Wernicke BioDocumento2 pagineWernicke BiolizardocdNessuna valutazione finora
- Pathological Grooming: Evidence For A Single Factor Behind Trichotillomania, Skin Picking and Nail BitingDocumento13 paginePathological Grooming: Evidence For A Single Factor Behind Trichotillomania, Skin Picking and Nail BitinglizardocdNessuna valutazione finora
- ECT ReviewDocumento6 pagineECT ReviewlizardocdNessuna valutazione finora
- Girls CharcotDocumento13 pagineGirls CharcotlizardocdNessuna valutazione finora
- Aggarwal Attitudes ECTDocumento7 pagineAggarwal Attitudes ECTlizardocdNessuna valutazione finora
- Musica LimbicaDocumento7 pagineMusica LimbicalizardocdNessuna valutazione finora
- Misunderstanding PsychopathologyDocumento12 pagineMisunderstanding Psychopathologylizardocd100% (1)
- Catatonia ReviewDocumento13 pagineCatatonia ReviewlizardocdNessuna valutazione finora
- La Silla de KraepelinDocumento3 pagineLa Silla de KraepelinlizardocdNessuna valutazione finora
- Do All Schizophrenia Patients Need Antipsychotic Treatment Continuously Throughout Their Lifetime? A 20-Year Longitudinal StudyDocumento12 pagineDo All Schizophrenia Patients Need Antipsychotic Treatment Continuously Throughout Their Lifetime? A 20-Year Longitudinal StudylizardocdNessuna valutazione finora
- 100 Años de Psiquiatria - KraepelinDocumento174 pagine100 Años de Psiquiatria - Kraepelinlizardocd100% (2)
- WC William NsDocumento6 pagineWC William NslizardocdNessuna valutazione finora
- WC William NsDocumento6 pagineWC William NslizardocdNessuna valutazione finora
- KRAEPELIN Clinical PsychiatryDocumento628 pagineKRAEPELIN Clinical Psychiatrylizardocd100% (3)
- Globalising Mental Health: A Neoliberal ProjectDocumento7 pagineGlobalising Mental Health: A Neoliberal ProjectlizardocdNessuna valutazione finora
- Management of Acute Stress, PTSD, and Bereavement WHO RecommendationsDocumento2 pagineManagement of Acute Stress, PTSD, and Bereavement WHO RecommendationslizardocdNessuna valutazione finora
- The Secret Art of ArtaudDocumento102 pagineThe Secret Art of ArtaudlizardocdNessuna valutazione finora
- Pseudohallucinations - A Pseudoconcept - A ReviewDocumento9 paginePseudohallucinations - A Pseudoconcept - A ReviewlizardocdNessuna valutazione finora
- The Death of Casagemas: Early Picasso, The Blue Period, Mortality, and RedemptionDocumento14 pagineThe Death of Casagemas: Early Picasso, The Blue Period, Mortality, and Redemptionlizardocd100% (5)
- Dylan Thomas (1914-1953), by Cohen SG, Rizzo PL.Documento11 pagineDylan Thomas (1914-1953), by Cohen SG, Rizzo PL.lizardocdNessuna valutazione finora
- The Failure of The Schizophrenia Concept and The Argument For Its Replacement by HebephreniaDocumento11 pagineThe Failure of The Schizophrenia Concept and The Argument For Its Replacement by HebephrenializardocdNessuna valutazione finora
- Berrios - Delusional Parasitosis and Physical DiseaseDocumento9 pagineBerrios - Delusional Parasitosis and Physical DiseaselizardocdNessuna valutazione finora
- Psychosocial Modifiers of Drug Prescription: The Hidden Face of Pharmacology?Documento7 paginePsychosocial Modifiers of Drug Prescription: The Hidden Face of Pharmacology?lizardocdNessuna valutazione finora
- XOJane - My Former Friend's Death Was A Blessing - Amanda LaurenDocumento5 pagineXOJane - My Former Friend's Death Was A Blessing - Amanda LaurenMatthew Keys100% (3)
- REPORTDocumento11 pagineREPORTMuskan SukhejaNessuna valutazione finora
- 2ND CotDocumento14 pagine2ND CotJessa MolinaNessuna valutazione finora
- Italy vs. Norway - FinalDocumento12 pagineItaly vs. Norway - FinalLucija MajstrovićNessuna valutazione finora
- Personal Philosophy of Nursing-Nurs 401Documento7 paginePersonal Philosophy of Nursing-Nurs 401api-369824515Nessuna valutazione finora
- Significance and Beneficiaries of StudyDocumento22 pagineSignificance and Beneficiaries of StudyJehu Rey Obrero CabañesNessuna valutazione finora
- Precede/ProceedDocumento10 paginePrecede/ProceedOo OoNayNessuna valutazione finora
- MCS Summary Chapter 3 RendellDocumento3 pagineMCS Summary Chapter 3 RendellCaca LioniesaNessuna valutazione finora
- A Study of Cash Waqf ContributionDocumento17 pagineA Study of Cash Waqf Contributionwanda novitaNessuna valutazione finora
- Growth Mindset in The Music ClassroomDocumento11 pagineGrowth Mindset in The Music Classroomapi-659613441Nessuna valutazione finora
- Assignment Defense MechanismsDocumento4 pagineAssignment Defense MechanismsJamoi Ray VedastoNessuna valutazione finora
- Effective Adjustment To New EnvironmentDocumento23 pagineEffective Adjustment To New EnvironmentUtkarsh JaiswalNessuna valutazione finora
- Exploring The Coping Mechanism of Grade 10 Students in Facing StressDocumento40 pagineExploring The Coping Mechanism of Grade 10 Students in Facing StressYurie GuanzonNessuna valutazione finora
- Complete Bibliography: Erving Goffman S Writings: Anders Persson, Lund UniversityDocumento3 pagineComplete Bibliography: Erving Goffman S Writings: Anders Persson, Lund UniversityStefan BobocNessuna valutazione finora
- Anya S. Salik G12-STEM - Sison Understanding Culture, Society and Politics Quarter 1 - Module 5Documento3 pagineAnya S. Salik G12-STEM - Sison Understanding Culture, Society and Politics Quarter 1 - Module 5Naila SalikNessuna valutazione finora
- Implementing Project-Based Learning Challenges and SolutionsDocumento4 pagineImplementing Project-Based Learning Challenges and SolutionsConsultor Académico BooksNessuna valutazione finora
- Perception: - Dr. Preeti SurkutwarDocumento18 paginePerception: - Dr. Preeti SurkutwarTM TopChartsNessuna valutazione finora
- Division of Sta Rosa City: Republic of The Philippines Department of Education Region Iv-CalabarzonDocumento6 pagineDivision of Sta Rosa City: Republic of The Philippines Department of Education Region Iv-CalabarzonRowena Bathan Solomon100% (2)
- Lesson4 PDFDocumento17 pagineLesson4 PDFMiguel MartinezNessuna valutazione finora
- Self RegulationDocumento24 pagineSelf RegulationM Merllan MierNessuna valutazione finora
- Psychological Aspects of Stress and Adaptation - AmolDocumento12 paginePsychological Aspects of Stress and Adaptation - Amoldanimon1984Nessuna valutazione finora
- HRM in Thirukural-IraianbuDocumento15 pagineHRM in Thirukural-IraianbuGovindasamy Arumugam100% (1)
- Sociologicalperspectivesoneducation 161115200614Documento14 pagineSociologicalperspectivesoneducation 161115200614Anonymous 6gthRenNessuna valutazione finora
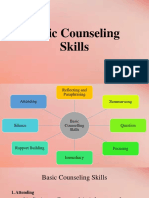
- Lesson On Counselling (Basic Skills On Counselling)Documento11 pagineLesson On Counselling (Basic Skills On Counselling)Alliyah PantinopleNessuna valutazione finora
- Peace Theme 6Documento30 paginePeace Theme 6Rx ChauNessuna valutazione finora
- ReflectionDocumento2 pagineReflectionRuffa AlarconNessuna valutazione finora
- Educ1 Module 1Documento10 pagineEduc1 Module 1Kristina Marie lagartoNessuna valutazione finora
- OB Unit-1Documento18 pagineOB Unit-1cat lostNessuna valutazione finora
- Role-Play Training Session: Bullying in The Workplace (Long Term Care Facility)Documento4 pagineRole-Play Training Session: Bullying in The Workplace (Long Term Care Facility)ruaaNessuna valutazione finora