Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
January Case Study Edited
Caricato da
api-174496267Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
January Case Study Edited
Caricato da
api-174496267Copyright:
Formati disponibili
1
Amanuel Negussie Clinical Practicum I January 25, 2012
Papillary Thyroid Carcinoma History of Present Illness: DS is a 64 year old male with a left neck mass of thyroid cancer. In October 2012, the patient noticed a left neck mass that was approximately the size of half a baseball. A neck computed tomography (CT) study was performed and demonstrated a mass displacing the trachea and multiple abdominal lymph nodes. A chest CT also showed a mass extending to the mediastinum and multiple lung nodules, four of them with a size over 1 centimeter (cm). The patient also underwent a fine needle biopsy that showed a follicular neoplasm. In December 2012, DS underwent a total thyroidectomy. Operative reports mentioned extensive invasion and necrosis, including four major soft tissue masses in the region of the left thyroidectomy bed, the largest measuring 6.5x3.8x3 cm. The masses demonstrated moderate internal vascularity. No abnormality was seen with the right thyroid. The patient was released with a T3 staging. In January 2013, the patient took a thyroid replacement hormone and radioiodine ablation of 150 millicurie (mCi) of Iodine (I) -131. Past Medical History: DS has a past medical history of hypertension and dyslipidemia. He also had a total thyroidectomy, hormone replacement therapy, and radioiodine ablation. He has no known allergies. Family History: DS has an aunt who was previously diagnosed with Hodgkins lymphoma. Social History: DS is a self-employed individual. He is married and has no children. The patient denies the use of any drug, alcohol, and tobacco. Medication: DS is currently taking Aquaphone Healing Ointment, Decusate, Liothyronine, Sennosides, and Levothyroxine. He also takes Aspirin, Ibuprofen, Oxycodone, and Acetaminophen as needed for his pain. Diagnostic Imaging Studies: In early November, DS underwent a CT and ultrasound procedure that showed a large left thyroid mass extending into left lateral neck and mediastinal lymph nodes. Recommendations: Although the patient had a total thyroidectomy, hormone replacement therapy, and radioiodine ablation, he has a new mass growing in his left neck. For a recurrent
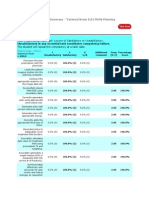
follicular cancer and for thyroid cancer that does not respond to I-131 treatment, external beam radiation treatment may be effective.2 As a result, external beam radiation therapy (EBRT) was recommended to control the new growing tumor. The Plan (Prescription): The radiation oncologists treatment recommendation to DS was three-dimentional (3D) conformal radiation therapy to the left neck mass. The radiation treatment plan was prescribed to 3000 centigray (cGy) at 300 cGy per fraction to the 98% isodose line for 10 fractions. Patient Setup/Immobilization: Patient was simulated supine with his neck extended using an aquaplast mask to immobilize head and shoulders (Figure 1). In addition, he was holding a shoulder strap to push the shoulder out of the treatment field. A Philips large bore 16 slice CT machine was used for the simulation. Head and neck images were taken at 0.3 cm slices. Anatomic Contouring: During simulation, the radiation oncologist put a wire marker on the scar across the neck where the surgery was performed. After the completion of CT scan, the CT slice images were imported to the Pinnacle3 9.0 radiation treatment planning system (TPS). The radiation oncologist then contoured the gross tumor volume (GTV) and planning target volume (PTV) on the TPS. Afterward, the certified medical dosimetrist (CMD) contoured the wire marker along with the body, left mastoid, spinal cord, mediastinum, trachea, vocal cords, and lips. Beam Isocenter/Arrangement: A Varian 21 IX 3994 linear accelerator (Linac) machine was used to treat the patient. The CMD placed a new calculation point within the GTV, because the isocenter placed by the radiation oncologist was close to the right field border. A two fields, anterior/posterior (AP) and posterior/anterior (PA), field arrangement was used. Gantry rotation was set at 0o for the AP and 180o for the PA, and the collimator was set at 0o for both fields. The AP field consisted of 6 megavolt (MV) and the PA consisted 18 MV beam energy. Treatment Planning: Each field has a multileaf collimator (MLC) blocking pattern which was constructed by the physician to define the treatment field. An enhanced dynamic wedge (EDW) of 15o was used on both treatment fields to account for the curvature of the neck, and reduce dose to the thinner part of the neck. Both the AP and PA fields were weighed proportional, 50% each. The plan was completed with a total monitor unit (MU) of 445, maximum dose of 3144.9 and a hot spot of 4% located within the GTV. Monitor Unit Check: The MU check was performed on MUcheck8.2.0 software. At our clinical site, a 3% deviation in MU is the tolerance for any 3DCRT plans. Anything outside this range
needs to be recalculated and fixed by the dosimetrists or physicists prior to treatment. The plan was approved with a 0.5% difference on the AP and -0.3% difference on the PA. Quality Assurance Checks: The treatment plan was later checked and approved by the radiation oncologist and medical physicist before the patient started his treatment. Conclusion: The challenge I faced when observing this treatment plan was understanding why the prescription was not calculated at the simulation isocenter (sim iso). However, after reviewing the International Committee on Radiation Units and Measurement (ICRU) 50 report, it was clear to me that a calculation point can be placed within the field if the sim iso is blocked or close to the field borders. According to the ICRU 50 report,1 a reference point should be clinically relevant and easy to define. It also suggests that the point should be selected where it should be accurately determined and cannot be affected by a steep dose gradient.1
Figures
Figure 1: Aquaplast immobilization mask
Figure 2: 3D AP and PA beam arrangement
Figure 3: Beams eye view (BEV) of the AP field
Figure 4: Beam and wedge arrangements
Figure 5: transverse, coronal, and sagittal view of dose distribution
Figure 6: Dose Volume Histogram (DVH)
10
References 1. ICRU Report 50. Prescribing, Recording, and Reporting, Photon Beam Therapy. Bethesda, MD.1993: 29-30. 2. Perez CA, Halperin EC, Brady LW. Principle & Practice of Radiation Oncology. 4th ed. U.S.A. Lippincott Williams &Wilkins; 2004: 1189-1190.
Potrebbero piacerti anche
- Amanuel Negussie: Certificate of AttendanceDocumento1 paginaAmanuel Negussie: Certificate of Attendanceapi-174496267Nessuna valutazione finora
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDocumento1 paginaV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267Nessuna valutazione finora
- ImrtDocumento3 pagineImrtapi-174496267Nessuna valutazione finora
- For E-PortfolioDocumento14 pagineFor E-Portfolioapi-174496267Nessuna valutazione finora
- ElectronDocumento2 pagineElectronapi-174496267Nessuna valutazione finora
- Conference LogsDocumento1 paginaConference Logsapi-174496267Nessuna valutazione finora
- WK VII WikiDocumento6 pagineWK VII Wikiapi-174496267Nessuna valutazione finora
- WK II WikiDocumento4 pagineWK II Wikiapi-174496267Nessuna valutazione finora
- WK VI WikiDocumento4 pagineWK VI Wikiapi-174496267Nessuna valutazione finora
- Esophagus and ProstateDocumento3 pagineEsophagus and Prostateapi-174496267Nessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- MRCS September 2023Documento8 pagineMRCS September 2023Maira KhanNessuna valutazione finora
- Subitcha T S - Case of Thyroid SwellingDocumento26 pagineSubitcha T S - Case of Thyroid SwellingsnehaNessuna valutazione finora
- Assessment of Serum Minerals and Electrolytes in TDocumento5 pagineAssessment of Serum Minerals and Electrolytes in THasni M MarsaolyNessuna valutazione finora
- Physiology MCQDocumento32 paginePhysiology MCQdip171100% (4)
- Im Grave's DiseaseDocumento28 pagineIm Grave's DiseaseHidvardNessuna valutazione finora
- GoiterDocumento4 pagineGoiterNader Smadi100% (1)
- Hypertiroidismo Review Lancet 2022Documento17 pagineHypertiroidismo Review Lancet 2022Diana Catalina Avila BareñoNessuna valutazione finora
- Chapter 01Documento109 pagineChapter 01JoyceM Martinez HerediaNessuna valutazione finora
- CretinismDocumento15 pagineCretinismJoshua fuentesNessuna valutazione finora
- Veterinary Medical Terminology: Dr.H.HoseinzadehDocumento16 pagineVeterinary Medical Terminology: Dr.H.HoseinzadehJuk CondeNessuna valutazione finora
- Sumant Sharma MD CIC. Regional Lab Nejran. KKSADocumento58 pagineSumant Sharma MD CIC. Regional Lab Nejran. KKSADr Sumant SharmaNessuna valutazione finora
- Medical Surgical Nursing 1Documento43 pagineMedical Surgical Nursing 1Tifanny Shaine Tomas100% (2)
- Jim LaValle - Atlanta PresentationDocumento222 pagineJim LaValle - Atlanta Presentationtquint23100% (1)
- Thyroid CancerDocumento82 pagineThyroid Cancerom100% (1)
- Goiter: What Is The Thyroid Gland?Documento2 pagineGoiter: What Is The Thyroid Gland?Julio LeviNessuna valutazione finora
- Wayne Index HyperthyroidDocumento1 paginaWayne Index HyperthyroidJam Tangan IdNessuna valutazione finora
- Beta HCG: Test Result Units Reference IntervalDocumento3 pagineBeta HCG: Test Result Units Reference IntervalBALANessuna valutazione finora
- Atlas of Thyroid UltrasonographyDocumento399 pagineAtlas of Thyroid Ultrasonographynino.matasNessuna valutazione finora
- PD22 HAP1 L04 FinalDocumento49 paginePD22 HAP1 L04 FinalKa Yan LAUNessuna valutazione finora
- QualityDocumento4 pagineQualityNIGHT tubeNessuna valutazione finora
- Chapter 1-4Documento11 pagineChapter 1-4Vy ThachNessuna valutazione finora
- Chapter 3 - HypothyroidismDocumento59 pagineChapter 3 - HypothyroidismSteffi AraujoNessuna valutazione finora
- Iodine: A Century of Medical Fraud: D. Th. D. Gerson Therapist Adv. Dip. NatDocumento11 pagineIodine: A Century of Medical Fraud: D. Th. D. Gerson Therapist Adv. Dip. NatMaria ShipkaNessuna valutazione finora
- Absite Questions MissedDocumento11 pagineAbsite Questions MissedVikram Patel100% (1)
- Psychoimmunology Essay by DR Romesh Senewiratne-Alagaratnam (MD)Documento32 paginePsychoimmunology Essay by DR Romesh Senewiratne-Alagaratnam (MD)Dr Romesh Arya Chakravarti100% (2)
- Pathophysiology of Hyperthyroidism and Thyroid StormDocumento3 paginePathophysiology of Hyperthyroidism and Thyroid StormPen MontanteNessuna valutazione finora
- Endocrine System ReviewerDocumento23 pagineEndocrine System ReviewerKimberly Joy GregorioNessuna valutazione finora
- Endocrine SystemDocumento11 pagineEndocrine SystemDayledaniel SorvetoNessuna valutazione finora
- Free T3Documento1 paginaFree T3Jason Roy Edward NathanNessuna valutazione finora
- Endocrine Male-FemaleDocumento4 pagineEndocrine Male-FemaleMoatasem AhmedNessuna valutazione finora